Routing to Endovascular Treatment of Ischemic Stroke in Korea: Recognition of Need for Process Improvement
- Affiliations
-
- 1Department of Neurology, Cerebrovascular Center, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea
- 2Department of Medicine, Gyeongsang National University College of Medicine, Jinju, Korea
- 3Department of Neurology, Inje University Ilsan Paik Hospital, Ilsan, Korea
- 4Department of Neurology, Nowon Eulji Medical Center, Eulji University, Seoul, Korea
- 5Department of Neurology, Chung-Ang University Hospital, Seoul, Korea
- 6Department of Neurology, Soonchunhyang University Hospital, Seoul, Korea
- 7Department of Neurology, Daejeon Eulji Medical Center, Eulji University, Daejeon, Korea
- 8Clinical Research Center, Asan Medical Center, Seoul, Korea
- 9Department of Biostatistics, Korea University College of Medicine, Seoul, Korea
- 10Health Insurance Review and Assessment Service, Wonju, Korea
- 11Department of Neurology, Gyeongsang National University College of Medicine, Jinju, Korea
- 12Department of Neurology, Northwestern University Feinberg School of Medicine, Chicago, IL, USA
- KMID: 2507826
- DOI: http://doi.org/10.3346/jkms.2020.35.e347
Abstract
- Background
To track triage, routing, and treatment status regarding access to endovascular treatment (EVT) after acute ischemic stroke (AIS) at a national level.
Methods
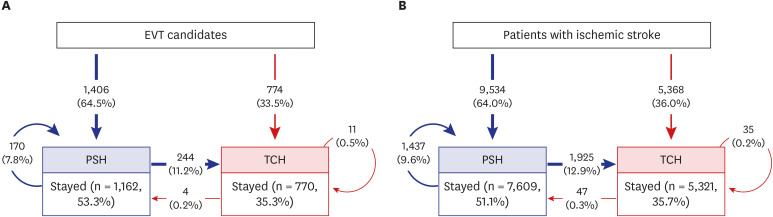
From national stroke audit data, potential candidates for EVT arriving within 6 hours with National Institute of Health Stroke Scale score of ≥ 7 were identified. Acute care hospitals were classified as thrombectomy-capable hospitals (TCHs, ≥ 15 EVT cases/year) or primary stroke hospital (PSH, < 15 cases/year), and patients' initial routes and subsequent inter-hospital transfer were described. Impact of initial routing to TCHs vs. PSHs on EVT and clinical outcomes were analyzed using multilevel generalized mixed effect models.
Results
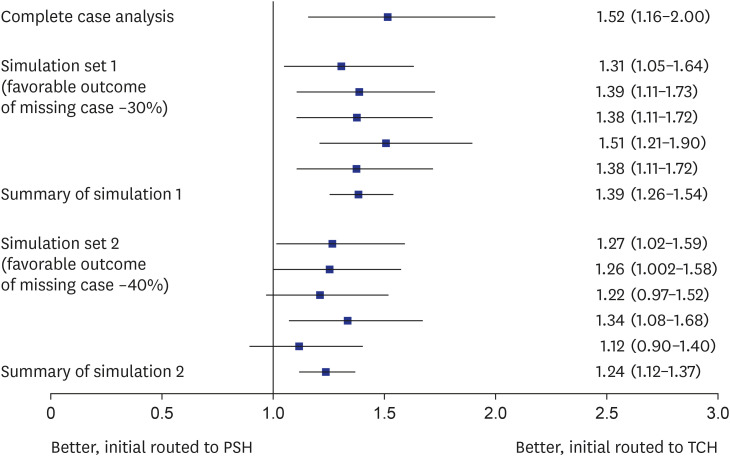
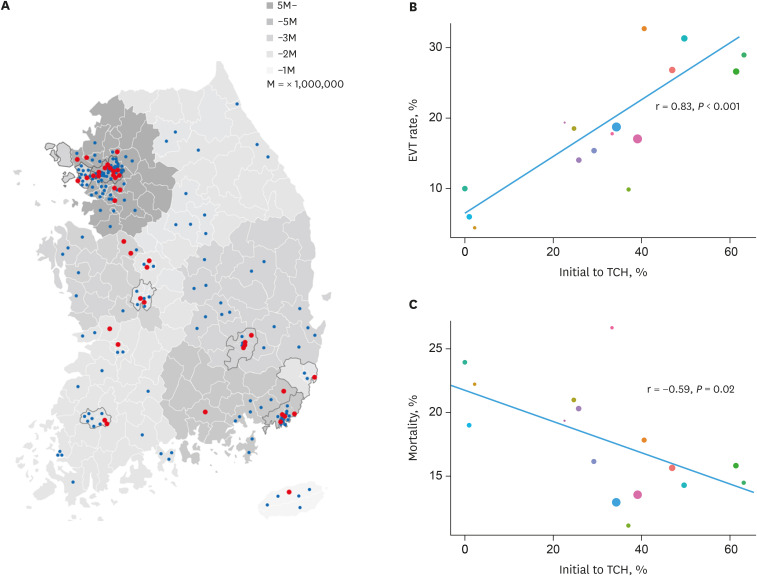
Out of 14,902 AIS patients, 2,180 (14.6%) were EVT candidates. Eighty-one percent of EVT candidates were transported by ambulance, but only one-third were taken initially to TCHs. Initial routing to TCHs was associated with greater chances of receiving EVT compared to initial routing to PSHs (33.3% vs 12.1%, P < 0.001; adjusted odds ratio [aOR], 2.21; 95% confidence interval [CI], 1.59–2.92) and favorable outcome (38.5% vs. 28.2%, P < 0.001; aOR, 1.52; 95% CI, 1.16–2.00). Inter-hospital transfers to TCHs occurred in 17.4% of those initially routed to a PSH and was associated with the greater chance of EVT compared to remaining at PSHs (34.8% vs. 7.5%, P < 0.001), but not with better outcomes.
Conclusion
Two-thirds of EVT candidates were initially routed to PSHs despite greater chance of receiving EVT and having favorable outcomes if routed to a TCH in Korea. Process improvement is needed to direct appropriate patients to TCHs.
Keyword
Figure
Cited by 2 articles
-
Effect of Transport Time on the Use of Reperfusion Therapy for Patients with Acute Ischemic Stroke in Korea
Jay Chol Choi, Joong-Goo Kim, Chul-Hoo Kang, Hee-Joon Bae, Jihoon Kang, Soo-Joo Lee, Jong-Moo Park, Tai Hwan Park, Yong-Jin Cho, Kyung Bok Lee, Jun Lee, Dong-Eog Kim, Jae-Kwan Cha, Joon-Tae Kim, Byung-Chul Lee, Ji-Sung Lee, Anthony S. Kim
J Korean Med Sci. 2021;36(11):e77. doi: 10.3346/jkms.2021.36.e77.Annual Case Volume and One-Year Mortality for Endovascular Treatment in Acute Ischemic Stroke
Jun Yup Kim, Jihoon Kang, Beom Joon Kim, Seong-Eun Kim, Do Yeon Kim, Keon-Joo Lee, Hong-Kyun Park, Yong-Jin Cho, Jong-Moo Park, Kyung Bok Lee, Jae-Kwan Cha, Ji Sung Lee, Juneyoung Lee, Ki Hwa Yang, Ock Ran Hong, Ji Hyeon Shin, Jung Hyun Park, Philip B. Gorelick, Hee-Joon Bae
J Korean Med Sci. 2022;37(36):e270. doi: 10.3346/jkms.2022.37.e270.
Reference
-
1. Alberts MJ, Latchaw RE, Jagoda A, Wechsler LR, Crocco T, George MG, et al. Revised and updated recommendations for the establishment of primary stroke centers: a summary statement from the brain attack coalition. Stroke. 2011; 42(9):2651–2665. PMID: 21868727.2. Abilleira S, Dávalos A, Chamorro A, Alvarez-Sabín J, Ribera A, Gallofré M, et al. Outcomes of intravenous thrombolysis after dissemination of the stroke code and designation of new referral hospitals in Catalonia: the Catalan Stroke Code and Thrombolysis (Cat-SCT) monitored study. Stroke. 2011; 42(7):2001–2006. PMID: 21566237.3. Saver JL, Goyal M, van der Lugt A, Menon BK, Majoie CBLM, Dippel DW, et al. Time to treatment with endovascular thrombectomy and outcomes from ischemic stroke: a meta-analysis. JAMA. 2016; 316(12):1279–1288. PMID: 27673305.4. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019; 50(12):e344–418. PMID: 31662037.
Article5. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. 2018 Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2018; 49(3):e46–110. PMID: 29367334.
Article6. Froehler MT, Saver JL, Zaidat OO, Jahan R, Aziz-Sultan MA, Klucznik RP, et al. Interhospital transfer before thrombectomy is associated with delayed treatment and worse outcome in the STRATIS registry (systematic evaluation of patients treated with neurothrombectomy devices for acute ischemic stroke). Circulation. 2017; 136(24):2311–2321. PMID: 28943516.7. Fang MC, Cutler DM, Rosen AB. Trends in thrombolytic use for ischemic stroke in the United States. J Hosp Med. 2010; 5(7):406–409. PMID: 20578049.
Article8. Scherf S, Limburg M, Wimmers R, Middelkoop I, Lingsma H. Increase in national intravenous thrombolysis rates for ischaemic stroke between 2005 and 2012: is bigger better? BMC Neurol. 2016; 16(1):53. PMID: 27103535.
Article9. Raychev RI, Stradling D, Patel N, Gee JR, Lombardi DA, Moon JL, et al. Evolution of a US county system for acute comprehensive stroke care. Stroke. 2018; 49(5):1217–1222. PMID: 29626136.
Article10. Yang JH, Kim SM, Han SJ, Knaak M, Yang GH, Lee KD, et al. The impact of Value Incentive Program (VIP) on the quality of hospital care for acute stroke in Korea. Int J Qual Health Care. 2016; 28(5):580–585. PMID: 27650012.
Article11. Kim JY, Lee KJ, Kang J, Kim BJ, Kim SE, Oh H, et al. Acute stroke care in Korea in 2013–2014: national averages and disparities. J Korean Med Sci. 2020; 35(20):e167. PMID: 32449325.
Article12. Park HK, Kim SE, Cho YJ, Kim JY, Oh H, Kim BJ, et al. Quality of acute stroke care in Korea (2008–2014): retrospective analysis of the nationwide and nonselective data for quality of acute stroke care. Eur Stroke J. 2019; 4(4):337–346. PMID: 31903432.
Article13. Heldner MR, Hsieh K, Broeg-Morvay A, Mordasini P, Bühlmann M, Jung S, et al. Clinical prediction of large vessel occlusion in anterior circulation stroke: mission impossible? J Neurol. 2016; 263(8):1633–1640. PMID: 27272907.
Article14. Lai SM, Duncan PW. Stroke recovery profile and the Modified Rankin assessment. Neuroepidemiology. 2001; 20(1):26–30. PMID: 11174042.
Article15. The Joint Commission. Certification for thrombectomy-capable stroke centers. Updated 2020. Accessed September 7, 2019. https://www.jointcommission.org/certification/certification_for_thrombectomycapable_stroke_centers.aspx.16. Kodankandath TV, Wright P, Power PM, Geronimo MD, Libman RB, Kwiatkowski T, et al. Improving transfer times for acute ischemic stroke patients to a comprehensive stroke center. J Stroke Cerebrovasc Dis. 2017; 26(1):192–195. PMID: 27743926.
Article17. Venema E, Groot AE, Lingsma HF, Hinsenveld W, Treurniet KM, Chalos V, et al. Effect of interhospital transfer on endovascular treatment for acute ischemic stroke. Stroke. 2019; 50(4):923–930. PMID: 30862265.
Article18. Gerschenfeld G, Muresan IP, Blanc R, Obadia M, Abrivard M, Piotin M, et al. Two paradigms for endovascular thrombectomy after intravenous thrombolysis for acute ischemic stroke. JAMA Neurol. 2017; 74(5):549–556. PMID: 28319240.
Article19. Sablot D, Gaillard N, Smadja P, Bonnec JM, Bonafe A. Thrombectomy accessibility after transfer from a primary stroke center: analysis of a three-year prospective registry. Int J Stroke. 2017; 12(5):519–523. PMID: 28375045.
Article20. Mohamad NF, Hastrup S, Rasmussen M, Andersen MS, Johnsen SP, Andersen G, et al. Bypassing primary stroke centre reduces delay and improves outcomes for patients with large vessel occlusion. Eur Stroke J. 2016; 1(2):85–92. PMID: 31008269.
Article21. Higashida R, Alberts MJ, Alexander DN, Crocco TJ, Demaerschalk BM, Derdeyn CP, et al. Interactions within stroke systems of care: a policy statement from the American Heart Association/American Stroke Association. Stroke. 2013; 44(10):2961–2984. PMID: 23988638.22. Détraz L, Ernst M, Bourcier R. Stroke transfer and its organizational paradigm: review of organizational paradigms and the impact on outcome. Clin Neuroradiol. 2018; 28(4):473–480. PMID: 30091041.23. Schlemm E, Ebinger M, Nolte CH, Endres M, Schlemm L. Optimal transport destination for ischemic stroke patients with unknown vessel status: use of prehospital triage scores. Stroke. 2017; 48(8):2184–2191. PMID: 28655816.24. Saposnik G, Baibergenova A, O'Donnell M, Hill MD, Kapral MK, Hachinski V, et al. Hospital volume and stroke outcome: does it matter? Neurology. 2007; 69(11):1142–1151. PMID: 17634420.
Article25. Song S, Saver J. Growth of regional acute stroke systems of care in the United States in the first decade of the 21st century. Stroke. 2012; 43(7):1975–1978. PMID: 22669404.
Article26. Meretoja A, Roine RO, Kaste M, Linna M, Roine S, Juntunen M, et al. Effectiveness of primary and comprehensive stroke centers: PERFECT stroke: a nationwide observational study from Finland. Stroke. 2010; 41(6):1102–1107. PMID: 20395609.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endovascular Treatment of Acute Ischemic Stroke
- Intravenous Thrombolysis and Endovascular Thrombectomy in Acute Ischemic Stroke with Minor Symptom
- Recent advances in ischemic stroke management
- Simultaneous Onset of Ischemic and Hemorrhagic Stroke Due To Intracranial Artery Dissection
- Endovascular Mechanical Thrombectomy for Acute Ischemic Stroke: A New Standard of Care