Ann Lab Med.
2020 Nov;40(6):466-473. 10.3343/alm.2020.40.6.466.
Proenkephalin Predicts Organ Failure, Renal Replacement Therapy, and Mortality in Patients With Sepsis
- Affiliations
-
- 1Department of Laboratory Medicine, Konkuk University School of Medicine, Seoul, Korea
- 2Sphingotec GmbH, Hennigsdorf, Germany
- 3Department of Medical-Surgery Sciences and Translational Medicine, School of Medicine and Psychology, Sapienza–University, Sant’ Andrea Hospital, Rome, Italy
- KMID: 2507792
- DOI: http://doi.org/10.3343/alm.2020.40.6.466
Abstract
- Background
Kidney failure occurs frequently and is associated with high mortality during sepsis. Proenkephalin (PENK) is an emerging biomarker of kidney function. We explored whether PENK levels could predict severity, organ failure, and mortality in septic patients.
Methods
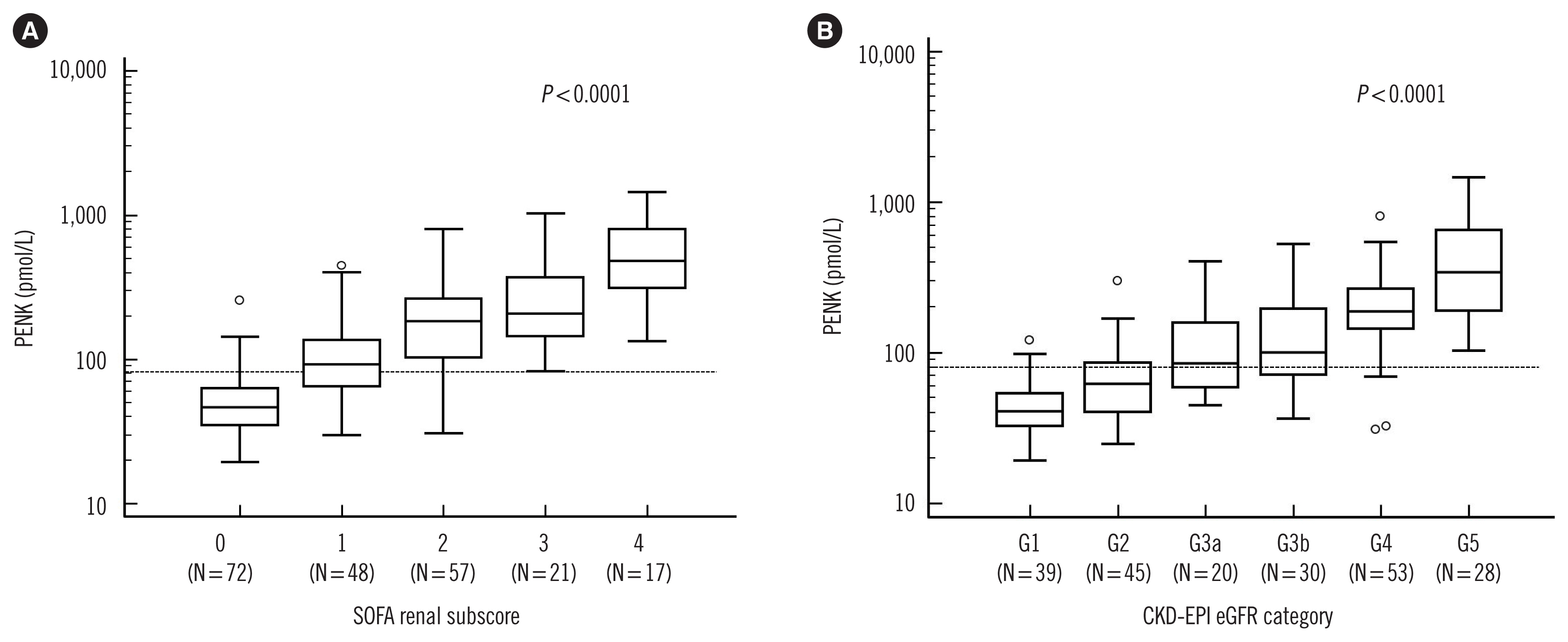
We measured the PENK level in the plasma of 215 septic patients using the sphingotest penKid assay (Sphingotec GmbH, Hennigsdorf, Germany). This was analyzed in terms of sepsis severity, vasopressor use, 30-day mortality, sequential organ failure assessment (SOFA) renal subscore, the Chronic Kidney Disease Epidemiology Collaboration estimated glomerular filtration rate (CKD-EPI eGFR) categories, and renal replacement therapy (RRT) requirement.
Results
The PENK levels were significantly higher in patients with septic shock, vasopressor use, and non-survivors than in patients with solitary sepsis, no vasopressor use, and survivors, respectively (P = 0.02, P = 0.007, P < 0.001, respectively). The PENK levels were significantly associated with SOFA renal subscore and CKD-EPI eGFR categories (both P < 0.001). The distribution of lower eGFR ( < 60 mL/min/1.73 m2 ), RRT requirement, SOFA renal subscore, and the number of organ failures differed significantly according to the PENK quartile (P for trend < 0.001 or 0.017). The 30-day mortality rate also differed significantly according to the PENK quartile (P for trend < 0.001).
Conclusions
PENK could be an objective and reliable marker to predict severity, organ failure, and 30-day mortality in septic patients.
Keyword
Figure
Cited by 1 articles
-
Biomarker-Guided Risk Assessment for Acute Kidney Injury: Time for Clinical Implementation?
Christian Albert, Michael Haase, Annemarie Albert, Antonia Zapf, Rüdiger Christian Braun-Dullaeus, Anja Haase-Fielitz
Ann Lab Med. 2021;41(1):1-15. doi: 10.3343/alm.2021.41.1.1.
Reference
-
1. Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016; 315:801–10.
Article2. Bellomo R, Kellum JA, Ronco C, Wald R, Martensson J, Maiden M, et al. Acute kidney injury in sepsis. Intensive Care Med. 2017; 43:816–28.
Article3. Ronco C, Bellomo R, Kellum JA. Acute kidney injury. Lancet. 2019; 394:1949–64.
Article4. Rangaswami J, Bhalla V, Blair JEA, Chang TI, Costa S, Lentine KL, et al. Cardiorenal syndrome: classification, pathophysiology, diagnosis, and treatment strategies: a scientific statement from the American Heart Association. Circulation. 2019; 139:e840–78.
Article5. Lee SA, Cozzi M, Bush EL, Rabb H. Distant organ dysfunction in acute kidney injury: a review. Am J Kidney Dis. 2018; 72:846–56.
Article6. Poston JT, Koyner JL. Sepsis associated acute kidney injury. BMJ. 2019; 364:k4891.
Article7. Kellum JA, Bellomo R, Ronco C. Progress in prevention and treatment of acute kidney injury: moving beyond kidney attack. JAMA. 2018; 320:437–8.8. KDIGO clinical practice guideline for acute kidney injury. Kidney Int Suppl. 2012; 2:1–141.9. Palevsky PM, Liu KD, Brophy PD, Chawla LS, Parikh CR, Thakar CV, et al. KDOQI US commentary on the 2012 KDIGO clinical practice guideline for acute kidney injury. Am J Kidney Dis. 2013; 61:649–72.
Article10. Vincent JL, Moreno R, Takala J, Willatts S, De Mendonça A, Bruining H, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the working group on sepsis-related problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996; 22:707–10.11. Joannidis M, Forni LG. Clinical review: timing of renal replacement therapy. Crit Care. 2011; 15:223.
Article12. Ernst A, Köhrle J, Bergmann A. Proenkephalin A 119–159, a stable proenkephalin A precursor fragment identified in human circulation. Peptides. 2006; 27:1835–40.
Article13. Beunders R, Struck J, Wu AHB, Zarbock A, Di Somma S, Mehta RL, et al. Proenkephalin (PENK) as a novel biomarker for kidney function. J Appl Lab Med. 2017; 2:400–12.
Article14. Beunders R, van Groenendael R, Leijte G, Kox M, Pickkers P. Proenkephalin compared to conventional methods to assess kidney function in critically ill sepsis patients. Shock. 2020; Jan. 21. DOI: 10.1097/SHK.0000000000001510.
Article15. Marino R, Struck J, Hartmann O, Maisel AS, Rehfeldt M, Magrini L, et al. Diagnostic and short-term prognostic utility of plasma pro-enkephalin (pro-ENK) for acute kidney injury in patients admitted with sepsis in the emergency department. J Nephrol. 2015; 28:717–24.
Article16. Kim H, Hur M, Lee S, Marino R, Magrini L, Cardelli P, et al. Proenkephalin, neutrophil gelatinase-associated lipocalin, and estimated glomerular filtration rates in patients with sepsis. Ann Lab Med. 2017; 37:388–97.
Article17. Caironi P, Latini R, Struck J, Hartmann O, Bergmann A, Bellato V, et al. Circulating proenkephalin, acute kidney injury, and its improvement in patients with severe sepsis or shock. Clin Chem. 2018; 64:1361–9.
Article18. Hollinger A, Wittebole X, François B, Pickkers P, Antonelli M, Gayat E, et al. Proenkephalin A 119–159 (Penkid) is an early biomarker of septic acute kidney injury: the Kidney in Sepsis and Septic Shock (Kid-SSS) Study. Kidney Int Rep. 2018; 3:1424–33.
Article19. Moledina DG. Penkid: a novel biomarker of reduced GFR in sepsis. Kidney Int Rep. 2018; 4:17–9.
Article20. Shah KS, Taub P, Patel M, Rehfeldt M, Struck J, Clopton P, et al. Proenkephalin predicts acute kidney injury in cardiac surgery patients. Clin Nephrol. 2015; 83:29–35.
Article21. Emmens JE, Ter Maaten JM, Damman K, van Veldhuisen DJ, de Boer RA, Struck J, et al. Proenkephalin, an opioid system surrogate, as a novel comprehensive renal marker in heart failure. Circ Heart Fail. 2019; 12:e005544.
Article22. Kanagala P, Squire IB, Jones DJL, Cao TH, Chan DCS, McCann G, et al. Proenkephalin and prognosis in heart failure with preserved ejection fraction: a GREAT network study. Clin Res Cardiol. 2019; 108:940–9.
Article23. Donato LJ, Meeusen JW, Lieske JC, Bergmann D, Sparwaßer A, Jaffe AS. Analytical performance of an immunoassay to measure proenkephalin. Clin Biochem. 2018; 58:72–7.
Article24. Wu AHB, Anand I. The biological variation of plasma proenkephalin: data from a stable heart failure cohort. Clin Chem Lab Med. 2019; 57:e105–7.
Article25. Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009; 150:604–12.
Article26. Cole TJ. Too many digits: the presentation of numerical data. Arch Dis Child. 2015; 100:608–9.
Article27. Legrand M, Hollinger A, Vieillard-Baron A, Dépret F, Cariou A, Deye N, et al. One-year prognosis of kidney injury at discharge from the ICU: a multicenter observational study. Crit Care Med. 2019; 47:e953–61.28. Rosenqvist M, Bronton K, Hartmann O, Bergmann A, Struck J, Melander O. Proenkephalin a 119–159 (penKid)–a novel biomarker for acute kidney injury in sepsis: an observational study. BMC Emerg Med. 2019; 19:75.29. Thomas ME, Blaine C, Dawnay A, Devonald MA, Ftouh S, Laing C, et al. The definition of acute kidney injury and its use in practice. Kidney Int. 2015; 87:62–73.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Circulating Biologically Active Adrenomedullin Predicts Organ Failure and Mortality in Sepsis
- Renal Replacement Therapies on the Outcomes of Acute Renal Failure Patients in ICU
- Simultaneous Extracorporeal Membrane Oxygenation, Renal Replacement Therapy, and Plasma Exchange for Thrombocytopenia-Associated Multiple Organ Failure
- Continuous Renal Replacement Therapy (CRRT) in Intensive Care Unit (ICU) Patients with Acute Renal Failure
- Influence of Daily Fluid Balance prior to Continuous Renal Replacement Therapy on Outcomes in Critically Ill Patients