J Korean Med Sci.
2020 Oct;35(40):e366. 10.3346/jkms.2020.35.e366.
Cardiac Manifestations of Coronavirus Disease 2019 (COVID-19): a Multicenter Cohort Study
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Yongin Severance Hospital, Yonsei University College of Medicine, Yongin, Korea
- 2Division of Cardiology, Department of Internal Medicine, Yeungnam University Medical Center, Daegu, Korea
- 3Department of Internal Medicine, Yeungnam University Medical Center, Daegu, Korea
- 4Data Science Team (Biostatistician), Center for Digital Health, Yongin Severance Hospital, Yonsei University College of Medicine, Yongin, Korea
- 5Division of Cardiology, Department of Internal Medicine, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- 6Division of Cardiology, Department of Internal Medicine, Cardiovascular Center, Keimyung University Dongsan Hospital, Keimyung University School of Medicine, Daegu, Korea
- 7Chungju Medical Center, Chungju, Korea
- KMID: 2507620
- DOI: http://doi.org/10.3346/jkms.2020.35.e366
Abstract
- Background
This study aimed to investigate the cardiac manifestations of coronavirus disease 2019 (COVID-19).
Methods
From February to March 2020, we prospectively and retrospectively enrolled consecutive patients diagnosed with COVID-19. Patient's data such as the demographic characteristics, symptoms, vital signs, laboratory and radiologic findings, electrocardiographic, and echocardiographic data, including the global longitudinal strain (GLS) of both ventricles, were obtained.
Results
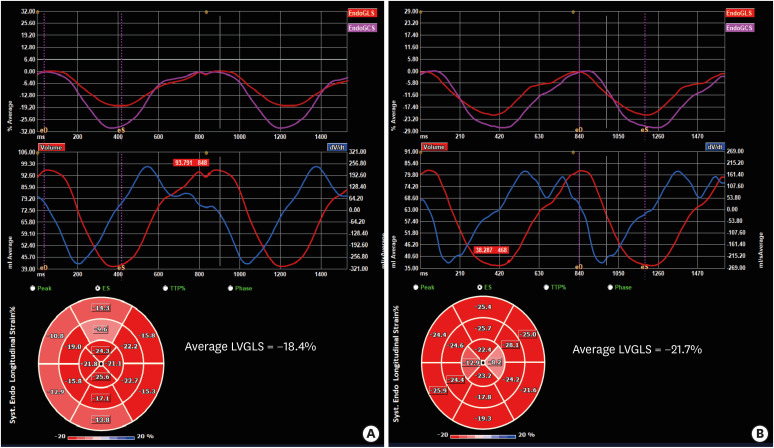
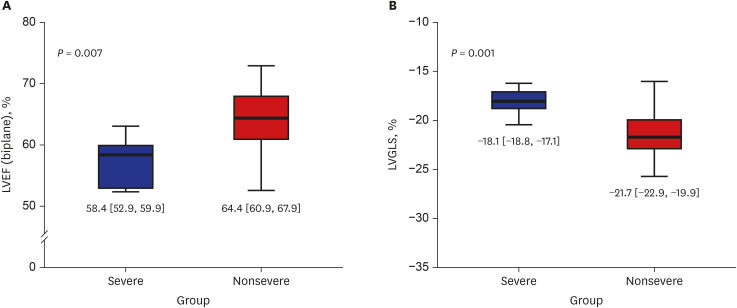
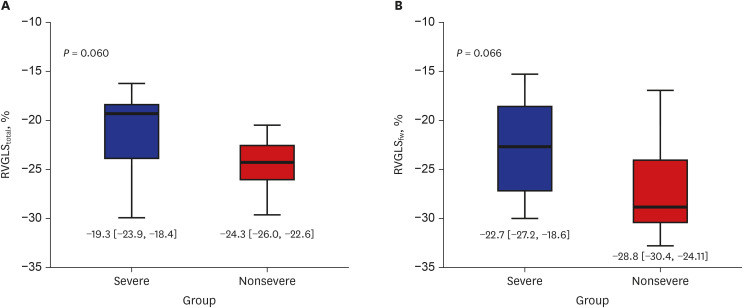
Forty patients (median age, 58 years; 50% men) were enrolled in the initial analysis. Patients were classified into severe and nonsevere groups based on the current guidelines. The 13 patients in the severe group were significantly older, had a greater prevalence of bilateral pneumonia and leukocytosis, and higher aspartate transaminase levels than patients in the nonsevere group. Patients in the severe group had a slightly lower left ventricular ejection fraction (LVEF) than those in the nonsevere group (median [interquartile range], 61.0% [58.5%, 62.3%] vs. 66.7% [60.6%, 69.8%], P = 0.015). In a subgroup of 34 patients in whom GLS could be analyzed, patients in the severe group had a significantly impaired left ventricular GLS (LVGLS) than those in the nonsevere group (−18.1% [−18.8%, −17.1%] vs. −21.7% [−22.9%, −19.9%], P = 0.001). There were no significant differences in total wall (RVGLS total , −19.3% [−23.9%, −18.4%] vs. −24.3% [−26.0%, −22.6%], P = 0.060) and free wall (RVGLS fw , −22.7% [−27.2%, −18.6%] vs. −28.8% [−30.4%, −24.1%], P = 0.066) right ventricle GLS (RVGLS).
Conclusion
Patients with severe COVID-19 had lower LVEF and LVGLS. RVGLS was not different between patients with severe and nonsevere COVID-19.
Keyword
Figure
Reference
-
1. Lu R, Zhao X, Li J, Niu P, Yang B, Wu H, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020; 395(10224):565–574. PMID: 32007145.2. World Health Organization. Coronavirus Disease (COVID-2019) Situation Report-107. Geneva: World Health Organization;2020.3. Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020; 382(18):1708–1720. PMID: 32109013.4. Deng SQ, Peng HJ. Characteristics of and public health responses to the coronavirus disease 2019 outbreak in China. J Clin Med. 2020; 9(2):575.
Article5. Mehra MR, Desai SS, Kuy S, Henry TD, Patel AN. Cardiovascular disease, drug therapy, and mortality in COVID-19. N Engl J Med. 2020; 382(26):2582.
Article6. Guo T, Fan Y, Chen M, Wu X, Zhang L, He T, et al. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19). JAMA Cardiol. 2020; 5(7):811–818. PMID: 32219356.
Article7. Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020; 8(5):475–481. PMID: 32105632.
Article8. Metlay JP, Waterer GW, Long AC, Anzueto A, Brozek J, Crothers K, et al. Diagnosis and treatment of adults with community-acquired pneumonia. an official clinical practice guideline of the American Thoracic Society and Infectious Diseases Society of America. Am J Respir Crit Care Med. 2019; 200(7):e45–67. PMID: 31573350.
Article9. Vink AS, Neumann B, Lieve KVV, Sinner MF, Hofman N, El Kadi S, et al. Determination and interpretation of the QT interval. Circulation. 2018; 138(21):2345–2358. PMID: 30571576.
Article10. Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015; 28(1):1–39.e14. PMID: 25559473.
Article11. Mor-Avi V, Lang RM, Badano LP, Belohlavek M, Cardim NM, Derumeaux G, et al. Current and evolving echocardiographic techniques for the quantitative evaluation of cardiac mechanics: ASE/EAE consensus statement on methodology and indications endorsed by the Japanese Society of Echocardiography. Eur J Echocardiogr. 2011; 12(3):167–205. PMID: 21385887.
Article12. Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol. 1996; 49(12):1373–1379. PMID: 8970487.
Article13. World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013; 310(20):2191–2194. PMID: 24141714.14. Karakas M, Haase T, Zeller T. Linking the sympathetic nervous system to the inflammasome: towards new therapeutics for atherosclerotic cardiovascular disease. Eur Heart J. 2018; 39(1):70–72. PMID: 29020243.
Article15. Paonessa JR, Brennan T, Pimentel M, Steinhaus D, Feng M, Celi LA. Hyperdynamic left ventricular ejection fraction in the intensive care unit. Crit Care. 2015; 19(1):288. PMID: 26250903.
Article16. Vieillard-Baron A, Prin S, Chergui K, Dubourg O, Jardin F. Hemodynamic instability in sepsis: bedside assessment by Doppler echocardiography. Am J Respir Crit Care Med. 2003; 168(11):1270–1276. PMID: 14644922.17. Liu H, Jayakumar S, Traboulsi M, Lee SS. Cirrhotic cardiomyopathy: Implications for liver transplantation. Liver Transpl. 2017; 23(6):826–835. PMID: 28407402.
Article18. Ruiz-del-Árbol L, Serradilla R. Cirrhotic cardiomyopathy. World J Gastroenterol. 2015; 21(41):11502–11521. PMID: 26556983.19. Zamorano JL, Lancellotti P, Rodriguez Muñoz D, Aboyans V, Asteggiano R, Galderisi M, et al. 2016 ESC position paper on cancer treatments and cardiovascular toxicity developed under the auspices of the ESC Committee for practice guidelines: the task force for cancer treatments and cardiovascular toxicity of the European Society of Cardiology (ESC). Eur J Heart Fail. 2017; 19(1):9–42. PMID: 27565769.20. Yingchoncharoen T, Gibby C, Rodriguez LL, Grimm RA, Marwick TH. Association of myocardial deformation with outcome in asymptomatic aortic stenosis with normal ejection fraction. Circ Cardiovasc Imaging. 2012; 5(6):719–725. PMID: 23008423.
Article21. Kim HM, Cho GY, Hwang IC, Choi HM, Park JB, Yoon YE, et al. Myocardial strain in prediction of outcomes after surgery for severe mitral regurgitation. JACC Cardiovasc Imaging. 2018; 11(9):1235–1244. PMID: 29778855.22. Sugimoto T, Dulgheru R, Bernard A, Ilardi F, Contu L, Addetia K, et al. Echocardiographic reference ranges for normal left ventricular 2D strain: results from the EACVI NORRE study. Eur Heart J Cardiovasc Imaging. 2017; 18(8):833–840. PMID: 28637227.23. Kaul S, Tei C, Hopkins JM, Shah PM. Assessment of right ventricular function using two-dimensional echocardiography. Am Heart J. 1984; 107(3):526–531. PMID: 6695697.
Article24. Rudski LG, Lai WW, Afilalo J, Hua L, Handschumacher MD, Chandrasekaran K, et al. Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr. 2010; 23(7):685–713. PMID: 20620859.25. Lu KJ, Chen JX, Profitis K, Kearney LG, DeSilva D, Smith G, et al. Right ventricular global longitudinal strain is an independent predictor of right ventricular function: a multimodality study of cardiac magnetic resonance imaging, real time three-dimensional echocardiography and speckle tracking echocardiography. Echocardiography. 2015; 32(6):966–974. PMID: 25287078.
Article26. Carluccio E, Biagioli P, Alunni G, Murrone A, Zuchi C, Coiro S, et al. Prognostic value of right ventricular dysfunction in heart failure with reduced ejection fraction: superiority of longitudinal strain over tricuspid annular plane systolic excursion. Circ Cardiovasc Imaging. 2018; 11(1):e006894. PMID: 29321212.
Article27. Li Y, Li H, Zhu S, Xie Y, Wang B, He L, et al. Prognostic value of right ventricular longitudinal strain in patients with COVID-19. JACC Cardiovasc Imaging. Forthcoming. 2020; DOI: 10.1016/j.jcmg.2020.04.014.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cardiovascular Manifestations of COVID-19
- Treatment for Immune Thrombocytopenia in Coronavirus Disease 2019 (COVID-19) Infection after COVID-19 Vaccination: A Case Report
- COVID-19 from the Perspective of a Gastroenterologist
- Clinical implications of coronavirus disease 2019 in neonates
- COVID-19 and Cancer: Questions to Be Answered