J Korean Med Sci.
2020 Oct;35(40):e345. 10.3346/jkms.2020.35.e345.
Incidence and Risk Factors of Gastrointestinal and Hepatobiliary Complications after Spinal Fusion Surgery: a Retrospective Cohort Study
- Affiliations
-
- 1Department of Orthopaedic Surgery, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 2Department of Orthopaedic Surgery, Eunpyeong St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 3Department of Orthopaedic Surgery, Kyung-Hee University Hospital at Gandong, School of Medicine, Kyung Hee University, Seoul, Korea
- KMID: 2507618
- DOI: http://doi.org/10.3346/jkms.2020.35.e345
Abstract
- Background
Spinal surgery holds a higher chance of unpredicted postoperative medical complications among orthopedic surgeries. Several studies have analyzed the risk factors for diverse postoperative medical complications, but the majority investigated incidences of each complication qualitatively. Among gastrointestinal complications, reports regarding postoperative ileus were relatively frequent. However, risk factors or incidences of hepatobiliary complications have yet to be investigated. The purpose of this study was to examine the incidence of gastrointestinal complications after spinal surgery, quantitatively analyze the risk factors of frequent complications, and to determine cues requiring early approaches.
Methods
In total, 234 consecutive patients who underwent spinal fusion surgery performed by one senior doctor at our institute in one-year period were retrospectively enrolled for analyses. The primary outcomes were presence of paralytic ileus, elevated serum alanine transaminase (ALT) and aspartate transaminase (AST) levels, and elevated total bilirubin levels. Univariate logistic regression analyses of all variables were performed. In turn, significant results were reanalyzed by multivariate logistic regression. The variables used were adjusted with age and gender.
Results
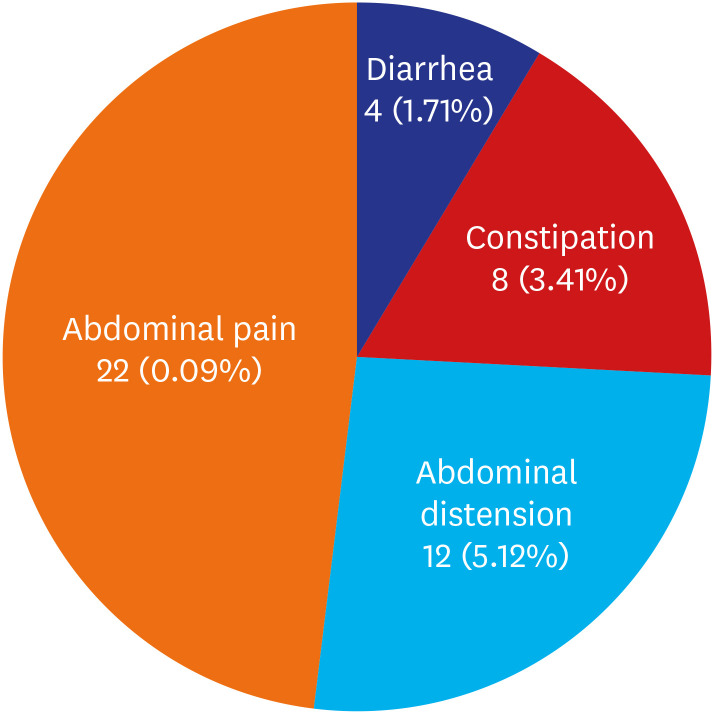
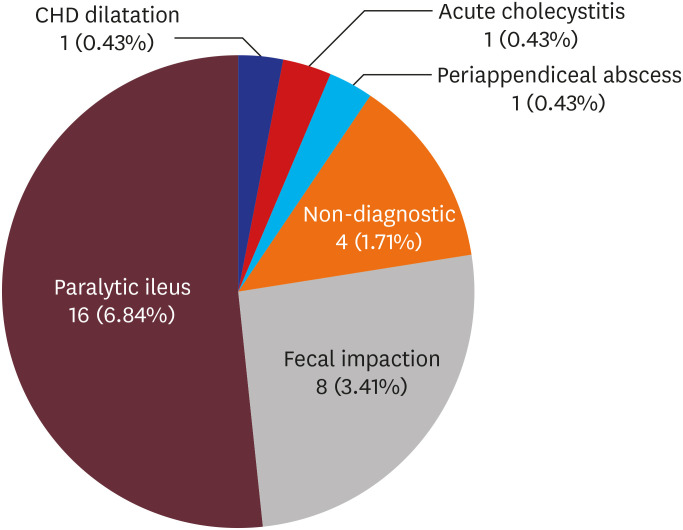
Gastrointestinal complications were observed in 15.8% of patients. Upon the risk factors of postoperative ileus, duration of anesthesia (odds ratio [OR], 1.373; P = 0.015), number of fused segments (OR, 1.202; P = 0.047), and hepatobiliary diseases (OR, 2.976; P = 0.029) were significantly different. For elevated liver enzymes, men (OR, 2.717; P = 0.003), number of fused segments (OR, 1.234; P = 0.033), and underlying hepatobiliary (OR, 2.704; P = 0.031) and rheumatoid diseases (OR, 5.021; P = 0.012) had significantly different results. Lastly, risk factors for total bilirubin elevation were: duration of anesthesia (OR, 1.431; P = 0.008), number of fused segments (OR, 1.359; P = 0.001), underlying hepatobiliary diseases (OR, 3.426; P = 0.014), and thoracolumbar junction involving fusions (OR, 4.134; P = 0.002) compared to lumbar spine limited fusions.
Conclusion
Patients on postoperative care after spinal surgery should receive direct attention as soon as possible after manifesting abdominal symptoms. Laboratory and radiologic results must be carefully reviewed, and early consultation to gastroenterologists or general surgeons is recommended to avoid preventable complications.
Keyword
Figure
Reference
-
1. Lee MJ, Konodi MA, Cizik AM, Bransford RJ, Bellabarba C, Chapman JR. Risk factors for medical complication after spine surgery: a multivariate analysis of 1,591 patients. Spine J. 2012; 12(3):197–206. PMID: 22245448.
Article2. Shapiro G, Green DW, Fatica NS, Boachie-Adjei O. Medical complications in scoliosis surgery. Curr Opin Pediatr. 2001; 13(1):36–41. PMID: 11176241.
Article3. Baron EM, Albert TJ. Medical complications of surgical treatment of adult spinal deformity and how to avoid them. Spine. 2006; 31(19):Suppl. S106–18. PMID: 16946627.
Article4. Sciubba DM, Yurter A, Smith JS, Kelly MP, Scheer JK, Goodwin CR, et al. A comprehensive review of complication rates after surgery for adult deformity: a reference for informed consent. Spine Deform. 2015; 3(6):575–594. PMID: 27927561.
Article5. Smith JS, Klineberg E, Lafage V, Shaffrey CI, Schwab F, Lafage R, et al. Prospective multicenter assessment of perioperative and minimum 2-year postoperative complication rates associated with adult spinal deformity surgery. J Neurosurg Spine. 2016; 25(1):1–14. PMID: 26918574.
Article6. Althausen PL, Gupta MC, Benson DR, Jones DA. The use of neostigmine to treat postoperative ileus in orthopedic spinal patients. J Spinal Disord. 2001; 14(6):541–545. PMID: 11723407.
Article7. Al Maaieh MA, Du JY, Aichmair A, Huang RC, Hughes AP, Cammisa FP, et al. Multivariate analysis on risk factors for postoperative ileus after lateral lumbar interbody fusion. Spine. 2014; 39(8):688–694. PMID: 24480952.
Article8. Oh CH, Ji GY, Yoon SH, Hyun D, Park HC, Kim YJ. Paralytic ileus and prophylactic gastrointestinal motility medication after spinal operation. Yonsei Med J. 2015; 56(6):1627–1631. PMID: 26446646.
Article9. Ichinose K, Yanagi F, Higashi K, Kozuma S, Akasaka T. Recurrent transient increases in liver enzymes specifically after isoflurane anesthesia. Masui. 1999; 48(4):421–423. PMID: 10339946.10. Obata R, Bito H, Ohmura M, Moriwaki G, Ikeuchi Y, Katoh T, et al. The effects of prolonged low-flow sevoflurane anesthesia on renal and hepatic function. Anesth Analg. 2000; 91(5):1262–1268. PMID: 11049919.
Article11. Ottinger LW. Acute cholecystitis as a postoperative complication. Ann Surg. 1976; 184(2):162–165. PMID: 952563.
Article12. Floman Y, Micheli LJ, Barker WD, Hall JE. Acute cholecystitis following the surgical treatment of spinal deformities in the adult: a report of three cases. Clin Orthop Relat Res. 1980; (151):205–209.13. Rochling FA. Evaluation of abnormal liver tests. Clin Cornerstone. 2001; 3(6):1–12.
Article14. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987; 40(5):373–383. PMID: 3558716.
Article15. Radovanovic D, Seifert B, Urban P, Eberli FR, Rickli H, Bertel O, AMIS Plus Investigators, et al. Validity of Charlson Comorbidity Index in patients hospitalised with acute coronary syndrome. Insights from the nationwide AMIS Plus registry 2002–2012. Heart. 2014; 100(4):288–294. PMID: 24186563.
Article16. Quan H, Li B, Couris CM, Fushimi K, Graham P, Hider P, et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol. 2011; 173(6):676–682. PMID: 21330339.
Article17. Fineberg SJ, Nandyala SV, Kurd MF, Marquez-Lara A, Noureldin M, Sankaranarayanan S, et al. Incidence and risk factors for postoperative ileus following anterior, posterior, and circumferential lumbar fusion. Spine J. 2014; 14(8):1680–1685. PMID: 24184650.
Article18. Asha MJ, Choksey MS, Shad A, Roberts P, Imray C. The role of the vascular surgeon in anterior lumbar spine surgery. Br J Neurosurg. 2012; 26(4):499–503. PMID: 22577849.
Article19. Vilz TO, Stoffels B, Strassburg C, Schild HH, Kalff JC. Ileus in adults. Dtsch Arztebl Int. 2017; 114(29-30):508–518. PMID: 28818187.
Article20. Ogilvy AJ, Smith G. The gastrointestinal tract after anaesthesia. Eur J Anaesthesiol Suppl. 1995; 10:35–42. PMID: 7641642.21. Behm B, Stollman N. Postoperative ileus: etiologies and interventions. Clin Gastroenterol Hepatol. 2003; 1(2):71–80. PMID: 15017498.
Article22. Artinyan A, Nunoo-Mensah JW, Balasubramaniam S, Gauderman J, Essani R, Gonzalez-Ruiz C, et al. Prolonged postoperative ileus-definition, risk factors, and predictors after surgery. World J Surg. 2008; 32(7):1495–1500. PMID: 18305994.
Article23. Kurz A, Sessler DI. Opioid-induced bowel dysfunction: pathophysiology and potential new therapies. Drugs. 2003; 63(7):649–671. PMID: 12656645.24. Marchant MH Jr, Viens NA, Cook C, Vail TP, Bolognesi MP. The impact of glycemic control and diabetes mellitus on perioperative outcomes after total joint arthroplasty. J Bone Joint Surg Am. 2009; 91(7):1621–1629. PMID: 19571084.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Perioperative Risk Factors Related to Lumbar Spine Fusion Surgery in Korean Geriatric Patients
- The Efficacy and Perioperative Complications Associated with Lumbar Spinal Fusion Surgery, Focusing on Geriatric Patients in the Republic of Korea
- Pseudarthrosis of the Cervical Spine: Risk Factors, Diagnosis and Management
- Adjacent Segment Pathology after Lumbar Spinal Fusion
- Comparison of Different Approaches in Lumbosacral Spinal Fusion Surgery: A Systematic Review and Meta-Analysis