J Korean Med Sci.
2020 Oct;35(40):e325. 10.3346/jkms.2020.35.e325.
Lack of Association between Low Cumulative Dose of Hydroxyethyl Starch and Acute Kidney Injury in Patients with Acute Ischemic Stroke
- Affiliations
-
- 1Department of Neurology, Inha University Hospital, Incheon, Korea
- 2Department of Critical Care Medicine, Inha University Hospital, Incheon, Korea
- 3Department of Hospital Medicine, Inha University Hospital, Incheon, Korea
- 4Department of Neurology, Seoul National University Hospital, Seoul, Korea
- 5Department of Critical Care Medicine, Seoul National University Hospital, Seoul, Korea
- 6Department of Neurology, Chung-Ang University Hospital, Seoul, Korea
- KMID: 2507615
- DOI: http://doi.org/10.3346/jkms.2020.35.e325
Abstract
- Background
Hydroxyethyl starch (HES, 6% 130/0.4) has been used as a volume expander for the treatment of cerebral hypoperfusion in acute ischemic stroke. Although HES use was associated with renal failure in sepsis or critical illness, it still remains to be elucidated whether HES is linked to renal adverse events in patients with acute ischemic stroke.
Methods
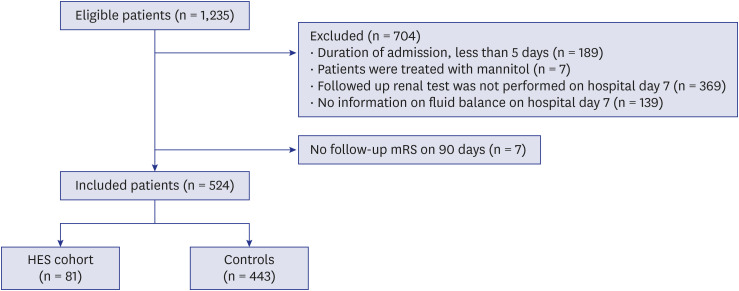
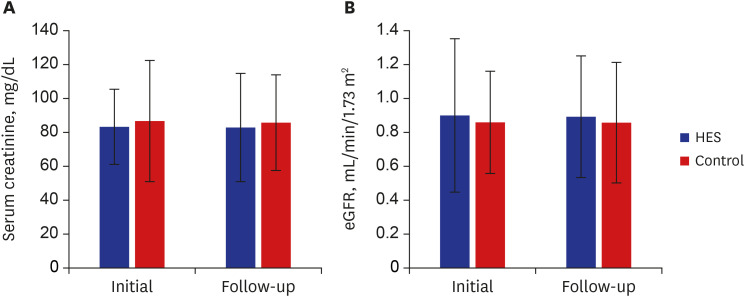
A total of 524 patients with acute ischemic stroke within 7 days of onset were included between January 2012 and May 2016. Renal function on admission and follow-up on day 7 ± 2 was assessed using serum creatinine (SCr) and estimated glomerular filtration rate (eGFR). Propensity score matching (PSM) was used to perform a 1:1 matched-pair analysis to minimize the group differences caused by covariates. The percentage of patients with newonset acute renal injury (AKI) using the Kidney Disease: Improving Global Outcomes or good functional outcome (modified Rankin Scale 0–2) at 90 days were compared between HES cohort and controls.
Results
Among the included patients (mean age, 68.6 years; male, 56.5%), 81 patients (15.5%) were HES cohort (median cumulative dose, 1,450 mL). Baseline renal function was better in HES cohort compared to that in the controls (SCr, 0.87 ± 0.43 mg/dL vs. 1.15 ± 1.15 mg/dL, P < 0.001; eGFR, 86.91 ± 24.27 mL/min vs. 74.55 ± 29.58 mL/min, P < 0.001), which became not significant in PSM cohort (72 pairs). The percentage of new-onset AKI did not differ between the HES cohort and controls (1.4% vs. 1.4%, P = 1.000). In addition, newonset AKI was not related to HES (odds ratio, 1.422; 95% confidence interval, 0.072–28.068; P = 0.817) after adjusting for confounders. HES cohort tended to have higher percentage of good functional outcome at 90 days compared to controls, which failed to reach statistical significance (68.1% vs. 54.2%, P = 0.087).
Conclusion
A low cumulative dose of HES was not associated with renal adverse events in patients with acute ischemic stroke.
Figure
Reference
-
1. Barron ME, Wilkes MM, Navickis RJ. A systematic review of the comparative safety of colloids. Arch Surg. 2004; 139(5):552–563. PMID: 15136357.
Article2. Aichner FT, Fazekas F, Brainin M, Pölz W, Mamoli B, Zeiler K. Hypervolemic hemodilution in acute ischemic stroke: the Multicenter Austrian Hemodilution Stroke Trial (MAHST). Stroke. 1998; 29(4):743–749. PMID: 9550505.3. van der Jagt M. Fluid management of the neurological patient: a concise review. Crit Care. 2016; 20(1):126. PMID: 27240859.
Article4. Bang OY, Chung JW, Kim SK, Kim SJ, Lee MJ, Hwang J, et al. Therapeutic-induced hypertension in patients with noncardioembolic acute stroke. Neurology. 2019; 93(21):e1955–e1963. PMID: 31645472.
Article5. Chang TS, Jensen MB. Haemodilution for acute ischaemic stroke. Cochrane Database Syst Rev. 2014; 8(8):CD000103.
Article6. Woessner R, Grauer MT, Dieterich HJ, Bepperling F, Baus D, Kahles T, et al. Influence of a long-term, high-dose volume therapy with 6% hydroxyethyl starch 130/0.4 or crystalloid solution on hemodynamics, rheology and hemostasis in patients with acute ischemic stroke. Results of a randomized, placebo-controlled, double-blind study. Pathophysiol Haemost Thromb. 2003; 33(3):121–126. PMID: 15170391.7. Myburgh JA, Finfer S, Bellomo R, Billot L, Cass A, Gattas D, et al. Hydroxyethyl starch or saline for fluid resuscitation in intensive care. N Engl J Med. 2012; 367(20):1901–1911. PMID: 23075127.
Article8. Perner A, Haase N, Guttormsen AB, Tenhunen J, Klemenzson G, Åneman A, et al. Hydroxyethyl starch 130/0.42 versus Ringer's acetate in severe sepsis. N Engl J Med. 2012; 367(2):124–134. PMID: 22738085.
Article9. Langeron O, Doelberg M, Ang ET, Bonnet F, Capdevila X, Coriat P. Voluven, a lower substituted novel hydroxyethyl starch (HES 130/0.4), causes fewer effects on coagulation in major orthopedic surgery than HES 200/0.5. Anesth Analg. 2001; 92(4):855–862. PMID: 11273914.
Article10. Visvanathan A, Dennis M, Whiteley W. Parenteral fluid regimens for improving functional outcome in people with acute stroke. Cochrane Database Syst Rev. 2015; 9(9):CD011138.
Article11. Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, et al. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis. 2009; 53(6):982–992. PMID: 19339088.
Article12. Levey AS, de Jong PE, Coresh J, El Nahas M, Astor BC, Matsushita K, et al. The definition, classification, and prognosis of chronic kidney disease: a KDIGO Controversies Conference report. Kidney Int. 2011; 80(1):17–28. PMID: 21150873.
Article13. Kasiske BL, Wheeler DC. Kidney disease: improving global outcomes--an update. Nephrol Dial Transplant. 2014; 29(4):763–769. PMID: 24286979.
Article14. Stevens PE, Levin A. Kidney Disease: Improving Global Outcomes Chronic Kidney Disease Guideline Development Work Group Members. Evaluation and management of chronic kidney disease: synopsis of the kidney disease: improving global outcomes 2012 clinical practice guideline. Ann Intern Med. 2013; 158(11):825–830. PMID: 23732715.
Article15. Hong KS, Kang DW, Koo JS, Yu KH, Han MK, Cho YJ, et al. Impact of neurological and medical complications on 3-month outcomes in acute ischaemic stroke. Eur J Neurol. 2008; 15(12):1324–1331. PMID: 19049549.
Article16. Weimar C, Mieck T, Buchthal J, Ehrenfeld CE, Schmid E, Diener HC, et al. Neurologic worsening during the acute phase of ischemic stroke. Arch Neurol. 2005; 62(3):393–397. PMID: 15767504.
Article17. Rubin DB. Estimating causal effects from large data sets using propensity scores. Ann Intern Med. 1997; 127(8 Pt 2):757–763. PMID: 9382394.
Article18. Zorrilla-Vaca A, Ziai W, Connolly ES Jr, Geocadin R, Thompson R, Rivera-Lara L. Acute kidney injury following acute ischemic stroke and intracerebral hemorrhage: a meta-analysis of prevalence rate and mortality risk. Cerebrovasc Dis. 2018; 45(1-2):1–9. PMID: 29176313.
Article19. Montomoli J, Donati A, Ince C. Acute kidney injury and fluid resuscitation in septic patients: are we protecting the kidney? Nephron. 2019; 143(3):170–173. PMID: 31394531.
Article20. Srisawat N, Kellum JA. Acute kidney injury: definition, epidemiology, and outcome. Curr Opin Crit Care. 2011; 17(6):548–555. PMID: 22027404.21. Bagshaw SM. Acute kidney injury: diagnosis and classification of AKI: AKIN or RIFLE? Nat Rev Nephrol. 2010; 6(2):71–73. PMID: 20111048.22. Siew ED, Matheny ME, Ikizler TA, Lewis JB, Miller RA, Waitman LR, et al. Commonly used surrogates for baseline renal function affect the classification and prognosis of acute kidney injury. Kidney Int. 2010; 77(6):536–542. PMID: 20042998.
Article23. Thomas ME, Blaine C, Dawnay A, Devonald MA, Ftouh S, Laing C, et al. The definition of acute kidney injury and its use in practice. Kidney Int. 2015; 87(1):62–73. PMID: 25317932.
Article24. Ostermann M, Joannidis M. Acute kidney injury 2016: diagnosis and diagnostic workup. Crit Care. 2016; 20(1):299. PMID: 27670788.
Article25. Luo X, Jiang L, Du B, Wen Y, Wang M, Xi X, et al. A comparison of different diagnostic criteria of acute kidney injury in critically ill patients. Crit Care. 2014; 18(4):R144. PMID: 25005361.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Recent findings on the use of hydroxyethyl starch
- Impact of hydroxyethyl starch 70/0.5 on acute kidney injury after gastroenterological surgery
- Role of T cells in ischemic acute kidney injury and repair
- Blood Pressure in Acute Ischemic Stroke
- Coagulation-Fibrinolysis system in acute progressive and non-progressive stroke: Preliminary study