Clin Endosc.
2020 Sep;53(5):562-567. 10.5946/ce.2020.022.
Comparison of Fentanyl versus Meperidine in Combination with Midazolam for Sedative Colonoscopy in Korea
- Affiliations
-
- 1Department of Internal Medicine, Dongguk University Ilsan Hospital, College of Medicine, Dongguk University, Goyang, Korea
- KMID: 2507590
- DOI: http://doi.org/10.5946/ce.2020.022
Abstract
- Background/Aims
Combination of midazolam and opioids is used widely for endoscopic sedation. Compared with meperidine, fentanyl is reportedly associated with rapid recovery, turnover rate of endoscopy room, and quality of endoscopy. We compared fentanyl with meperidine when combined with midazolam for sedative colonoscopy.
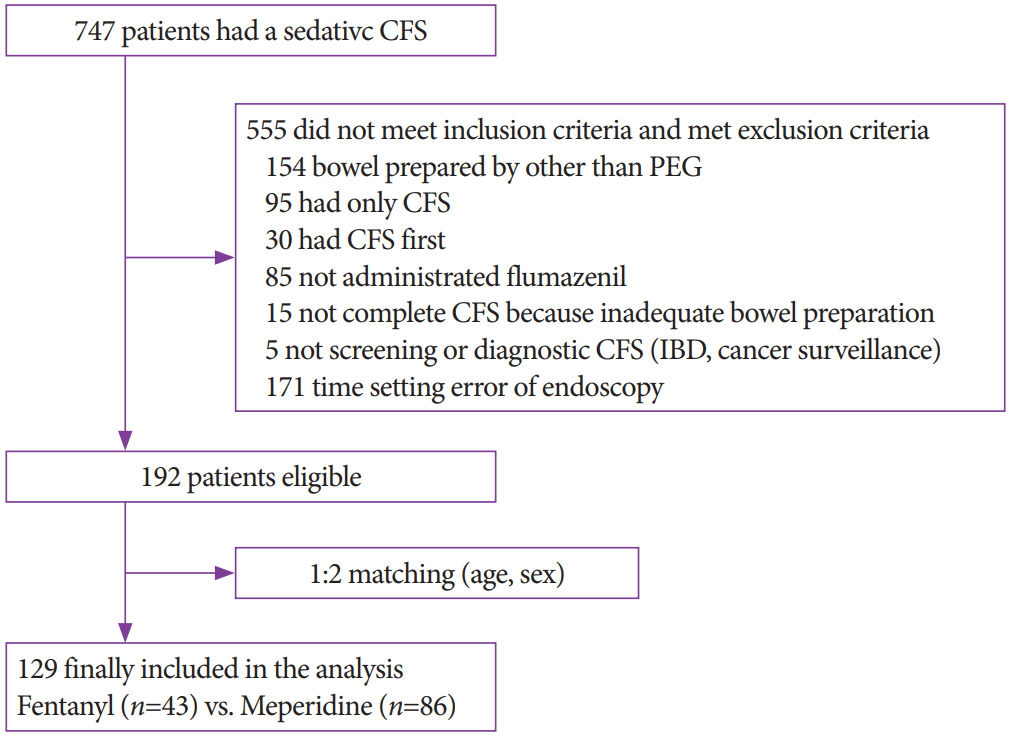
Methods
A retrospective, cross-sectional, 1:2 matching study was conducted. Induction and recovery time were compared as the primary outcomes. Moreover, cecal intubation time, withdrawal time, total procedure time of colonoscopy, paradoxical reaction, adenoma detection rate, and adverse effect of midazolam or opioids were assessed as the secondary outcomes.
Results
A total of 129 subjects (43 fentanyl vs. 86 meperidine) were included in the analysis. The fentanyl group showed significantly more rapid induction time (4.5±2.7 min vs. 7.5±4.7 min, p<0.001), but longer recovery time (59.5±25.6 min vs. 50.3±10.9 min, p=0.030) than the meperidine group. In multivariate analysis, the induction time of the fentanyl group was 3.40 min faster (p<0.001), but the recovery time was 6.38 min longer (p=0.046) than that of the meperidine group. There was no difference in withdrawal time and adenoma detection rate between the two groups.
Conclusions
The fentanyl group had more rapid sedation induction time but longer recovery time than the meperidine group.
Keyword
Figure
Cited by 1 articles
-
Risk Factors for Prolonged Hospital Stay after Endoscopy
Toshihiro Nishizawa, Shuntaro Yoshida, Osamu Toyoshima, Tatsuya Matsuno, Masataka Irokawa, Toru Arano, Hirotoshi Ebinuma, Hidekazu Suzuki, Takanori Kanai, Kazuhiko Koike
Clin Endosc. 2021;54(6):851-856. doi: 10.5946/ce.2020.292.
Reference
-
1. Jung KW, Won YJ, Kong HJ, Lee ES. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2016. Cancer Res Treat. 2019; 51:417–430.
Article2. Vital Statistics Division; Statistics Korea, Shin HY, Lee JY, et al. Cause-of-death statistics in 2016 in the Republic of Korea. J Korean Med Assoc. 2018; 61:573–584.
Article3. Pan J, Xin L, Ma YF, Hu LH, Li ZS. Colonoscopy reduces colorectal cancer incidence and mortality in patients with non-malignant findings: a meta-analysis. Am J Gastroenterol. 2016; 111:355–365.
Article4. Obara K, Haruma K, Irisawa A, et al. Guidelines for sedation in gastroenterological endoscopy. Dig Endosc. 2015; 27:435–449.
Article5. Triantafillidis JK, Merikas E, Nikolakis D, Papalois AE. Sedation in gastrointestinal endoscopy: current issues. World J Gastroenterol. 2013; 19:463–481.
Article6. Lee TH, Lee CK. Endoscopic sedation: from training to performance. Clin Endosc. 2014; 47:141–150.
Article7. Moon SH. Sedation regimens for gastrointestinal endoscopy. Clin Endosc. 2014; 47:135–140.
Article8. Cohen LB, Delegge MH, Aisenberg J, et al. AGA institute review of endoscopic sedation. Gastroenterology. 2007; 133:675–701.
Article9. Horn E, Nesbit SA. Pharmacology and pharmacokinetics of sedatives and analgesics. Gastrointest Endosc Clin N Am. 2004; 14:247–268.
Article10. Childers RE, Williams JL, Sonnenberg A. Practice patterns of sedation for colonoscopy. Gastrointest Endosc. 2015; 82:503–511.
Article11. Phillips SN, Fernando R, Girard T. Parenteral opioid analgesia: does it still have a role? Best Pract Res Clin Anaesthesiol. 2017; 31:3–14.
Article12. Hinkelbein J, Lamperti M, Akeson J, et al. European Society of Anaesthesiology and European Board of Anaesthesiology guidelines for procedural sedation and analgesia in adults. Eur J Anaesthesiol. 2018; 35:6–24.
Article13. Aldrete JA. The post-anesthesia recovery score revisited. J Clin Anesth. 1995; 7:89–91.
Article14. Jin EH, Hong KS, Lee Y, et al. How to improve patient satisfaction during midazolam sedation for gastrointestinal endoscopy? World J Gastroenterol. 2017; 23:1098–1105.
Article15. Hayee B, Dunn J, Loganayagam A, et al. Midazolam with meperidine or fentanyl for colonoscopy: results of a randomized trial. Gastrointest Endosc. 2009; 69(3 Pt 2):681–687.
Article16. Tegeder I, Lötsch J, Geisslinger G. Pharmacokinetics of opioids in liver disease. Clin Pharmacokinet. 1999; 37:17–40.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Midazolam versus Midazolam/Meperidine during Colonoscopy in a Prospective, Randomized, Double-Blind Study
- The effect of propofol for conscious sedation during colonoscopy-A Prospective, Randomized Study
- A Comparison of Fentanyl and Meperidine as Utilized in Patient Controlled Analgesia after Total Abdominal Hysterectomy
- Conscious Sedation with Midazolam Combined with Propofol for Colonoscopy
- Effect of Low - Dose Midazolam for Colonoscopy