Korean J Transplant.
2020 Sep;34(3):178-184. 10.4285/kjt.2020.34.3.178.
Korea-nationwide incidence of pediatric deceased donors and single-institutional status of liver transplantation using pediatric donor liver grafts
- Affiliations
-
- 1Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 2Department of Pediatrics, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2507162
- DOI: http://doi.org/10.4285/kjt.2020.34.3.178
Abstract
- Background
The present study intended to investigate the allocation status of pediatric deceased donor liver allografts. We analyzed the incidence of pediatric deceased donors in the Korean Network for Organ Sharing (KONOS) database and single-institutional status of liver transplantation (LT) using pediatric donors.
Methods
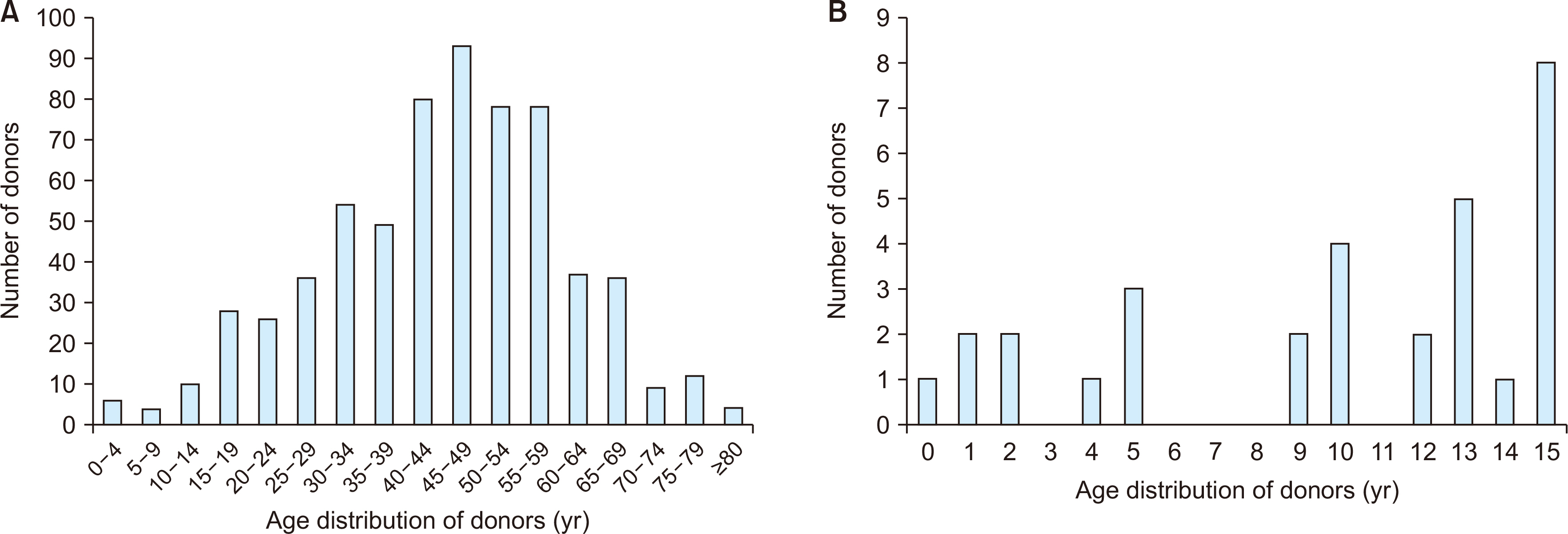
We assessed the nationwide incidence of pediatric donors aged ≤15 years and conducted single-center analysis of LT using pediatric donors.
Results
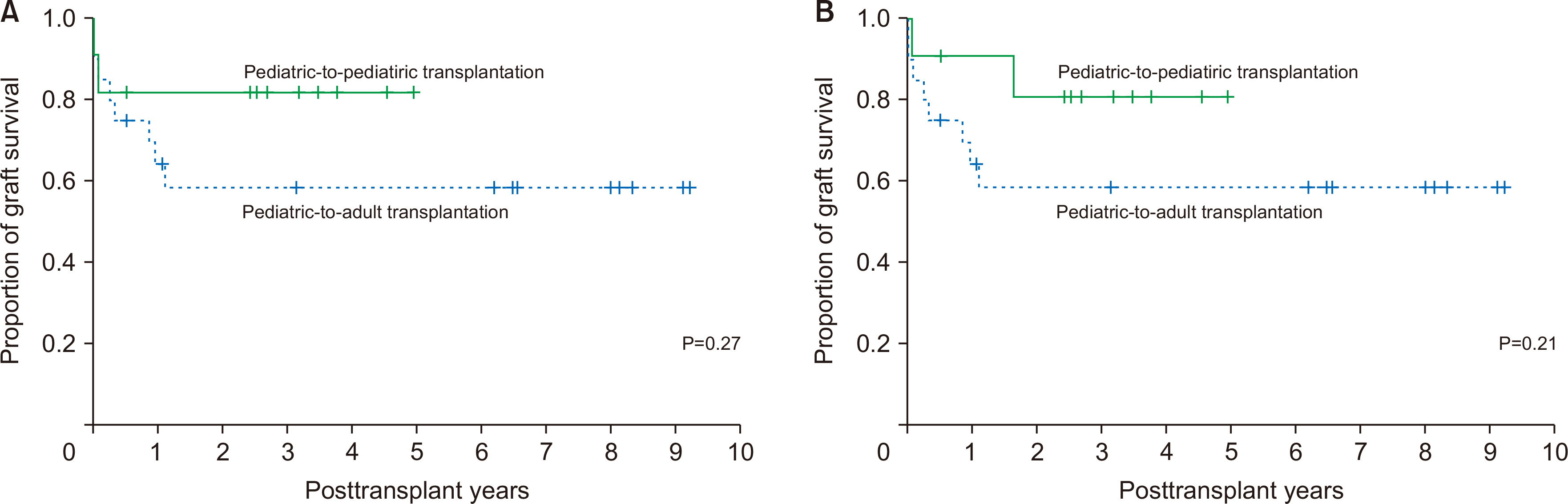
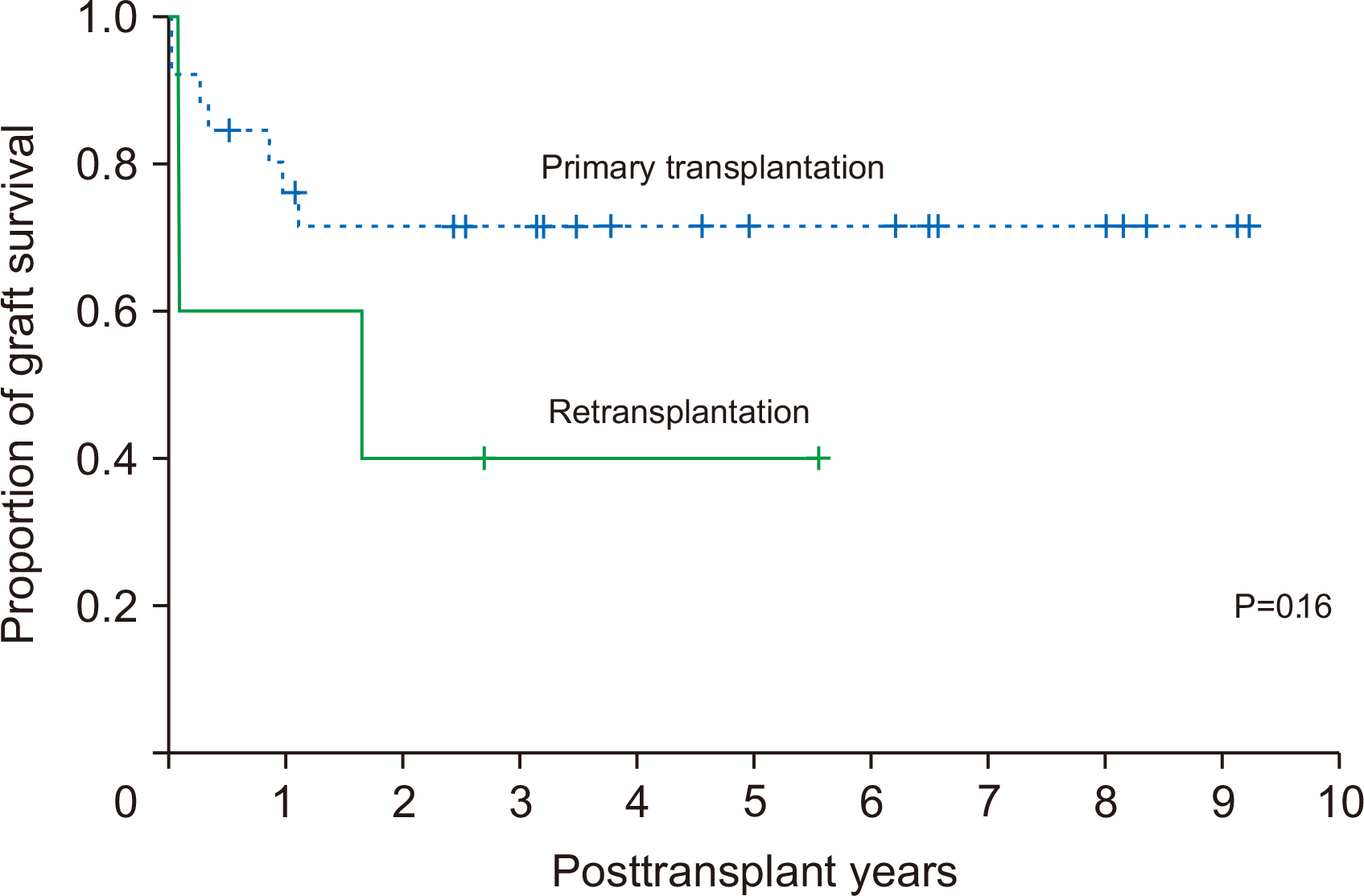
Between 2010 and 2019, pediatric donors aged ≤15 years accounted for 171 out of 4,395 donors (3.9%) in the KONOS database and 31 out of 640 liver donors (4.8%) in Asan Medical Center (AMC) database. In AMC, 11 (35.5%) and 20 (64.5%) grafts were allocated to pediatric recipients aged ≤15 years and adult recipients aged ≥19 years, respectively. All nine livers from donors aged ≤5 years were implanted in pediatric re-cipients aged ≤5 years. From 21 donors aged ≥9 years, 16 whole liver grafts and four split extended right liver grafts were implanted in 20 adult recipients and two split left lateral section grafts were implanted in two pediatric recipients. Four split liver grafts were implanted in other institutions. The overall patient survival rates at 1, 3, and 5 years were 90.9%, 80.8%, and 80.8%, respectively in pediatric-to-pediatric LT group and 69.6%, 58.4%, and 58.4%, respectively in pediatric-to-adult LT group (P=0.21).
Conclusions
More than half of the pediatric donor livers were allocated to adult patients. Recipient criteria for allocation of liver allografts from pediatric donors need revision for children on pediatric LT waitlist.
Keyword
Figure
Cited by 1 articles
-
Whole liver deceased donor liver transplantation for pediatric recipients: single-center experience for 20 years
Jung-Man Namgoong, Shin Hwang, Dae-Yeon Kim, Tae-Yong Ha, Gi-Won Song, Dong-Hwan Jung, Gil-Chun Park, Kyung Mo Kim, Seak Hee Oh
Korean J Transplant. 2020;34(4):249-256. doi: 10.4285/kjt.20.0036.
Reference
-
1. Emre S, Soejima Y, Altaca G, Facciuto M, Fishbein TM, Sheiner PA, et al. 2001; Safety and risk of using pediatric donor livers in adult liver transplantation. Liver Transpl. 7:41–7. DOI: 10.1053/jlts.2001.20940. PMID: 11150421.
Article2. Feng AC, Liao CY, Fan HL, Chen TW, Hsieh CB. 2015; A successful child-to-adult deceased donor liver transplantation: a case report and literature review. Ann Transplant. 20:21–4. DOI: 10.12659/AOT.893101. PMID: 25582243. PMCID: PMC4998643.
Article3. Zhang R, Zhu ZJ, Sun LY, Wei L, Qu W. 2018; Outcomes of liver transplantation using pediatric deceased donor livers: a single-center analysis of 102 donors. Chin Med J (Engl). 131:677–83. DOI: 10.4103/0366-6999.226901. PMID: 29521290. PMCID: PMC5865313.4. Lee S, Lee SK. 2019; Pediatric liver transplantation in Korea: long-term outcomes and allocations. J Korean Soc Transplant. 33:1–5. DOI: 10.4285/jkstn.2019.33.1.1.
Article5. Hwang S, Kim DY, Namgoong JM, Kim KM, Oh SH, Kim KH, et al. 2020; Living donor liver retransplantation for primary non-function of liver graft following multivisceral transplantation in a pediatric patient. Ann Hepatobiliary Pancreat Surg. 24:198–202. DOI: 10.14701/ahbps.2020.24.2.198. PMID: 32457267. PMCID: PMC7271102.
Article6. Kiuchi T, Kasahara M, Uryuhara K, Inomata Y, Uemoto S, Asonuma K, et al. 1999; Impact of graft size mismatching on graft prognosis in liver transplantation from living donors. Transplantation. 67:321–7. DOI: 10.1097/00007890-199901270-00024. PMID: 10075602.7. Vanatta JM, Esquivel CO. 2007; Status of liver transplantation in infants < 5 kg. Pediatr Transplant. 11:5–9. DOI: 10.1111/j.1399-3046.2006.00627.x. PMID: 17328158.8. Heffron TG, Welch D, Pillen T, Fasola C, Redd D, Smallwood GA, et al. 2005; Low incidence of hepatic artery thrombosis after pediatric liver transplantation without the use of intraoperative microscope or parenteral anticoagulation. Pediatr Transplant. 9:486–90. DOI: 10.1111/j.1399-3046.2005.00327.x. PMID: 16048601.
Article9. Shackleton CR, Goss JA, Swenson K, Colquhoun SD, Seu P, Kinkhabwala MM, et al. 1997; The impact of microsurgical hepatic arterial reconstruction on the outcome of liver transplantation for congenital biliary atresia. Am J Surg. 173:431–5. DOI: 10.1016/S0002-9610(97)00066-4. PMID: 9168083.
Article10. Ooi CY, Brandão LR, Zolpys L, de Angelis M, Drew W, Jones N, et al. 2010; Thrombotic events after pediatric liver transplantation. Pediatr Transplant. 14:476–82. DOI: 10.1111/j.1399-3046.2009.01252.x. PMID: 19849808. PMCID: PMC7520663.
Article11. Namgoong JM, Hwang S, Ahn CS, Jung DH, Park GC. 2020; Side-to-side portal vein reconstruction for infant-to-infant deceased donor whole liver transplantation: report of 2 cases with video. Ann Hepatobiliary Pancreat Surg. 24:301–4. DOI: 10.14701/ahbps.2020.24.3.301. PMID: 32843595. PMCID: PMC7452795.
Article12. United Network for Organ Sharing (UNOS). 2011. Organ distribution: allocation of livers [Internet]. UNOS;Richmond, VA: Available from: https://optn.transplant.hrsa.gov. cited 2020 Jun 30.13. United Network for Organ Sharing (UNOS). 2011. Ethical principles of pediatric organ allocation [Internet]. UNOS;Richmond, VA: Available from: https://optn.transplant.hrsa.gov. cited 2020 Jun 30.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Korea-nationwide incidence of pediatric deceased donors and single-institutional status of liver transplantation using pediatric donor liver grafts
- Whole liver deceased donor liver transplantation for pediatric recipients: single-center experience for 20 years
- Whole liver deceased donor liver transplantation for pediatric recipients: single-center experience for 20 years
- Pediatric liver transplantation in Korea: long-term outcomes and allocations
- Transplantation Techniques Unique in Pediatric Liver Transplantation