J Rheum Dis.
2020 Oct;27(4):285-289. 10.4078/jrd.2020.27.4.285.
Dermatomyositis Presenting as Life-threatening Hypercalcemia
- Affiliations
-
- 1Division of Endocrinology, Department of Medicine, Philippine General Hospital, University of the Philippines Manila, Manila, Philippines
- 2Division of Rheumatology, Department of Medicine, Philippine General Hospital, University of the Philippines Manila, Manila, Philippines
- 3Department of Dermatology, Philippine General Hospital, University of the Philippines Manila, Manila, Philippines
- 4Division of Oncology, Department of Medicine, Philippine General Hospital, University of the Philippines Manila, Manila, Philippines
- 5Department of Medicine, Philippine General Hospital, University of the Philippines Manila, Manila, Philippines
- KMID: 2506982
- DOI: http://doi.org/10.4078/jrd.2020.27.4.285
Abstract
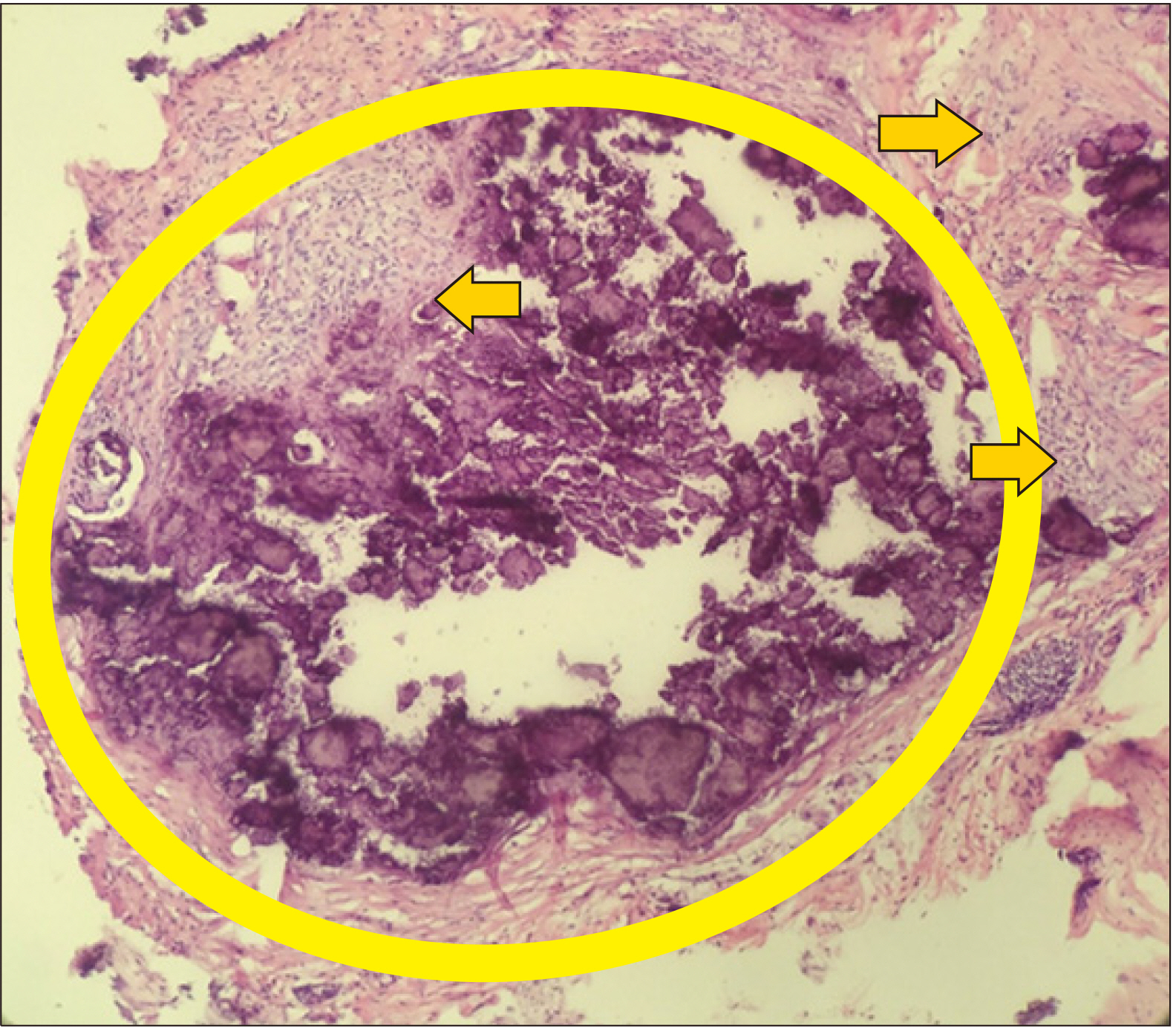
- Dermatomyositis is a rare disease characterized by classic skin lesions and muscle weakness. In rare cases, life-threatening hypercalcemia may develop caused by regression of dystrophic calcifications. Here we report a 36-year-old man who presented with progressive proximal weakness, difficulty in ambulation, and weight loss. He had the V-sign, Gottron’s papules, and hard, chalky nodules on both antecubital, thigh, and hip areas. Laboratory examinations revealed hypercalcemia (3.47 mmol/L) and shortened QT interval. Workup for malignancy and tuberculosis yielded negative results. Biopsy of the antecubital areas revealed calcinosis cutis. Serum calcium levels gradually normalized with hydration and steroids. Our case illustrated that a high index of suspicion for dermatomyositis is warranted for early diagnosis and ascertaining the etiology of hypercalcemia is vital in the management of this life-threatening complication. While hypercalcemia from dermatomyositis may respond to steroids, to date, individualization of treatment remains the standard of care.
Keyword
Figure
Reference
-
1. Hill CL, Zhang Y, Sigurgeirsson B, Pukkala E, Mellemkjaer L, Airio A, et al. 2001; Frequency of specific cancer types in dermatomyositis and polymyositis: a population-based study. Lancet. 357:96–100. DOI: 10.1016/S0140-6736(00)03540-6. PMID: 11197446.
Article2. Jakubaszek M, Kwiatkowska B, Maślińska M. 2015; Polymyositis and dermatomyositis as a risk of developing cancer. Reumatologia. 53:101–5. DOI: 10.5114/reum.2015.51510. PMID: 27407235. PMCID: PMC4847280.
Article3. Mattheou‐Vakali G, Ioannides D, Lazaridou E, Kalabalikis D, Batsios P, Minas A. 1997; Dermatomyositis sine myositis in five cases. J Eur Acad Dermatol Venereol. 8:208–11. DOI: 10.1111/j.1468-3083.1997.tb00480.x.4. Ni QF, Liu GQ, Pu LY, Kong LL, Kong LB. 2013; Dermatomyositis associated with gallbladder carcinoma: a case report. World J Hepatol. 5:230–3. DOI: 10.4254/wjh.v5.i4.230. PMID: 23671729. PMCID: PMC4248508.
Article5. Ghazi E, Sontheimer RD, Werth VP. 2013; The importance of including amyopathic dermatomyositis in the idiopathic inflammatory myositis spectrum. Clin Exp Rheumatol. 31:128–34. PMID: 23190767. PMCID: PMC3883437.6. Udkoff J, Cohen PR. 2016; Amyopathic dermatomyositis: a concise review of clinical manifestations and associated malignancies. Am J Clin Dermatol. 17:509. DOI: 10.1007/s40257-016-0199-z. PMID: 27256496.
Article7. Tiniakou E, Mammen AL. 2017; Idiopathic inflammatory myopathies and malignancy: a comprehensive review. Clin Rev Allergy Immunol. 52:20–33. DOI: 10.1007/s12016-015-8511-x. PMID: 26429706.
Article8. Sigurgeirsson B, Lindelöf B, Edhag O, Allander E. 1992; Risk of cancer in patients with dermatomyositis or polymyositis. A population-based study. N Engl J Med. 326:363–7. DOI: 10.1056/NEJM199202063260602. PMID: 1729618.9. Callen JP. 2002; When and how should the patient with dermatomyositis or amyopathic dermatomyositis be assessed for possible cancer? Arch Dermatol. 138:969–71. DOI: 10.1001/archderm.138.7.969. PMID: 12071827.
Article10. Wilsher ML, Holdaway IM, North JD. 1984; Hypercalcaemia during resolution of calcinosis in juvenile dermatomyositis. Br Med J (Clin Res Ed). 288:1345. DOI: 10.1136/bmj.288.6427.1345. PMID: 6424852. PMCID: PMC1440957.
Article11. Ostrov BE, Goldsmith DP, Eichenfield AH, Athreya BH. 1991; Hypercalcemia during the resolution of calcinosis universalis in juvenile dermatomyositis. J Rheumatol. 18:1730–4. PMID: 1787495.12. Shinjo SK, de Souza FHC. 2013; Update on the treatment of calcinosis in dermatomyositis. Rev Bras Reumatol. 53:211–4. DOI: 10.1016/S2255-5021(13)70025-7. PMID: 23856799.13. Terroso G, Bernardes M, Aleixo A, Madureira P, Vieira R, Bernardo A, et al. 2013; Therapy of calcinosis universalis complicating adult dermatomyositis. Acta Reumatol Port. 38:44–8. PMID: 24131911.14. Leclair V, Lundberg IE. 2018; New myositis classification criteria-what we have learned since Bohan and Peter. Curr Rheumatol Rep. 20:18. DOI: 10.1007/s11926-018-0726-4. PMID: 29550929. PMCID: PMC5857275.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Dermatomyositis First Presenting as Panniculitis
- A successful treatment of hypercalcemia with zoledronic acid in a 15-year-old boy with acute lymphoblastic leukemia
- Amyopathic Dermatomyositis with Interstitial Lung Disease: A Case Report
- A Case of Calciphylaxis Mimicking Dermatomyositis
- A Case of Amyopathic Dermatomyositis