J Cerebrovasc Endovasc Neurosurg.
2020 Sep;22(3):156-164. 10.7461/jcen.2020.22.3.156.
Surgical strategy for patients with supratentorial spontaneous intracerebral hemorrhage: minimally invasive surgery and conventional surgery
- Affiliations
-
- 1Department of Neurosurgery, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2506762
- DOI: http://doi.org/10.7461/jcen.2020.22.3.156
Abstract
Objective
The role of surgery in spontaneous intracerebral hemorrhage (sICH) is still controversial. We aimed to investigate the effectiveness of minimally invasive surgery (MIS) compared to conventional surgery (CS) for supratentorial sICH.
Methods
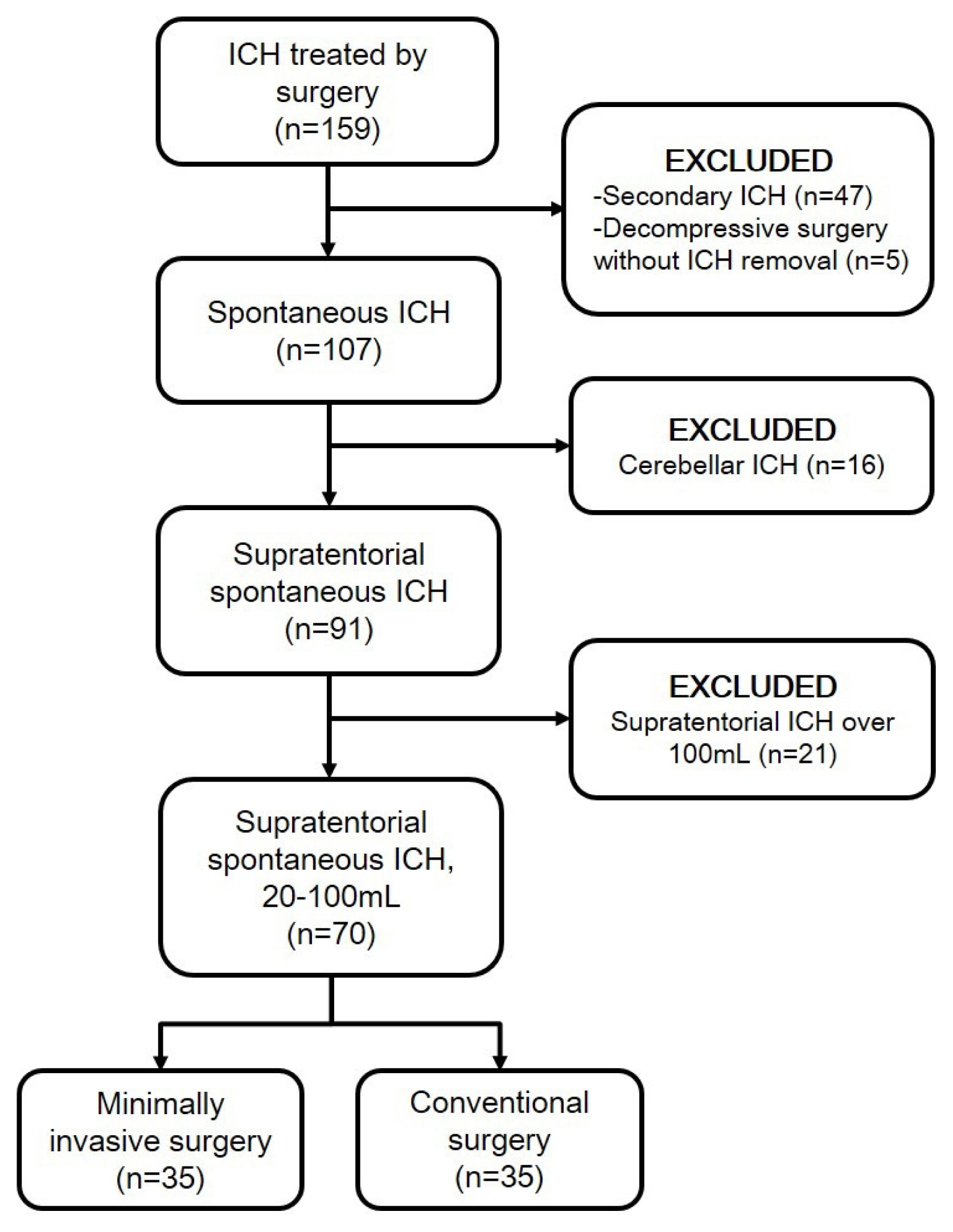
The medical data of 70 patients with surgically treated supratentorial sICH were retrospectively reviewed. MIS was performed in 35 patients, and CS was performed in 35 patients. The surgical technique was selected based on the neurological status and radiological findings, such as hematoma volume, neurological status and spot signs on computed tomographic angiography. Treatment outcomes, prognostic factors and the usefulness of the spot sign were analyzed.
Results
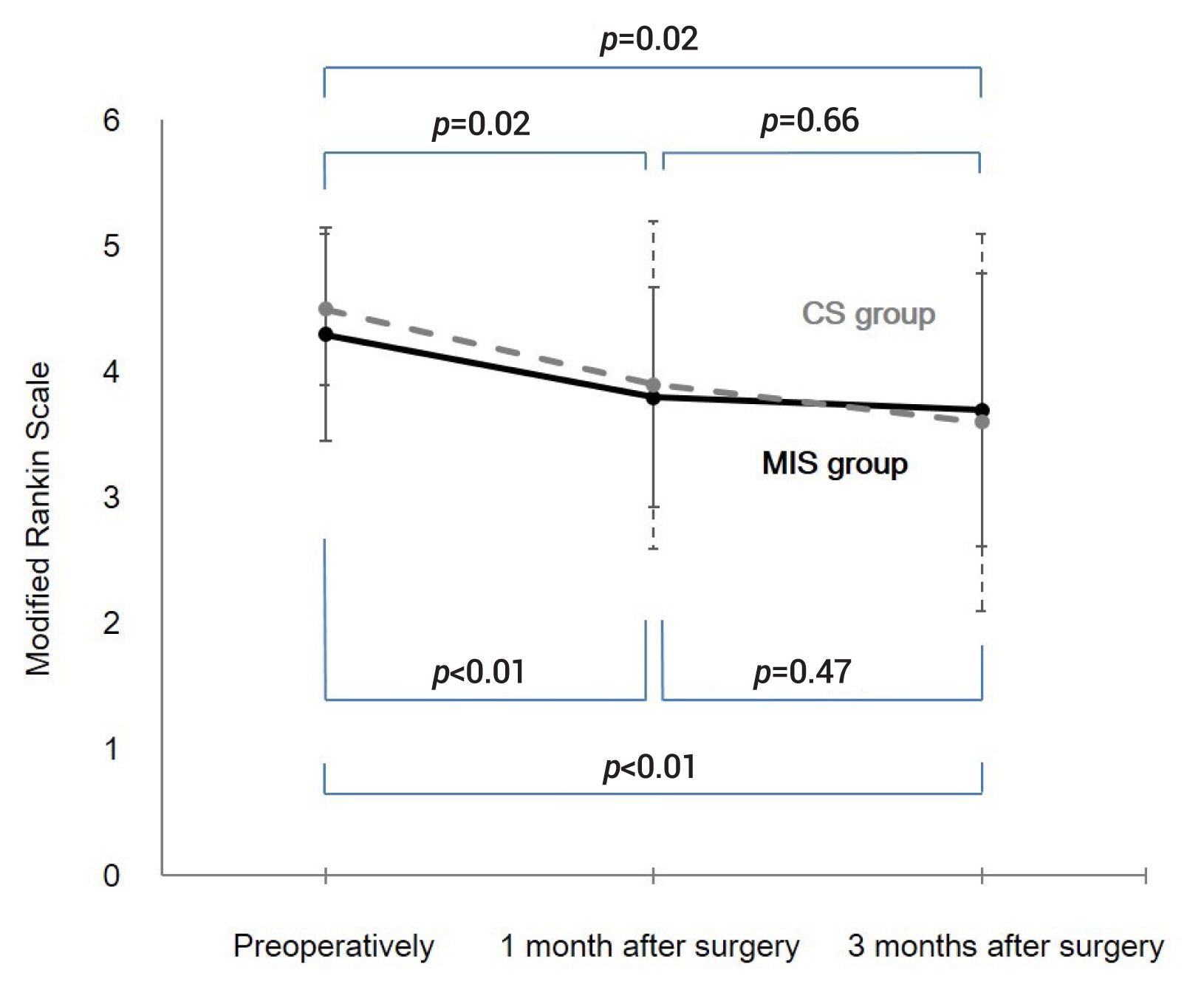
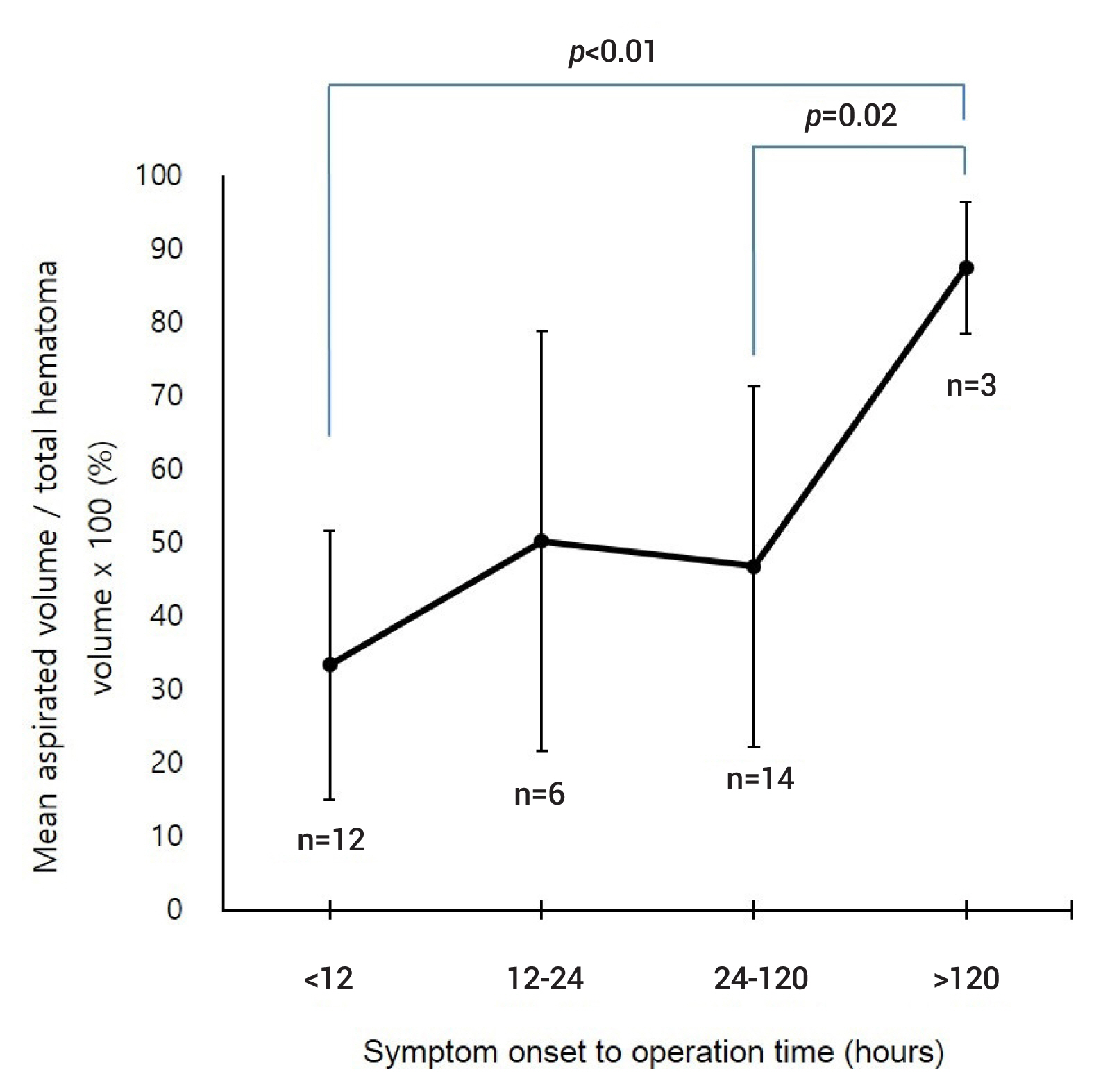
Clinical states in both groups were statistically similar, preoperatively, and in 1 and 3 months after surgery. Both groups showed significant progressive improvement till 3 months after surgery. Better preoperative neurological status, more hematoma removal and intensive care unit (ICU) stay ≤7 days were the significant prognostic factors for favorable 3-month clinical outcomes (odds ratio [OR] 0.31, 95% confidence interval [CI] 0.10-0.96, p=0.04; OR 1.04, 95% CI 1.01-1.08, p=0.02; OR 26.31, 95% CI 2.46-280.95, p=0.01, respectively). Initial hematoma volume and MIS were significant prognostic factors for a short ICU stay (≤7 days; OR 0.95; 95% CI 0.91-0.99; p=0.01; OR 3.91, 95% CI 1.03-14.82, p=0.045, respectively). No patients in the MIS group experienced hematoma expansion before surgery or postoperative rebleeding.
Conclusions
MIS was not inferior to CS in terms of clinical outcomes. The spot sign seems to be an effective radiological marker for predicting hematoma expansion and determining the surgical technique.
Keyword
Figure
Reference
-
1. Brouwers HB, Raffeld MR, van Nieuwenhuizen KM, Falcone GJ, Ayres AM, McNamara KA, et al. CT angiography spot sign in intracerebral hemorrhage predicts active bleeding during surgery. Neurology. 2014; Sep. 83(10):883–9.
Article2. Cho DY, Chen CC, Chang CS, Lee WY, Tso M. Endoscopic surgery for spontaneous basal ganglia hemorrhage: comparing endoscopic surgery, stereotactic aspiration, and craniotomy in noncomatose patients. Surg Neurol. 2006; Jun. 65(6):547–55.
Article3. Feigin VL, Lawes CM, Bennett DA, Barker-Collo SL, Parag V. Worldwide stroke incidence and early case fatality reported in 56 population-based studies: a systematic review. Lancet Neurol. 2009; Apr. 8(4):355–69.
Article4. Hanley DF, Thompson RE, Muschelli J, Rosenblum M, McBee N, Lane K, et al. Safety and efficacy of minimally invasive surgery plus alteplase in intracerebral haemorrhage evacuation (MISTIE): a randomised, controlled, open-label, phase 2 trial. Lancet Neurol. 2016; Nov. 15(12):1228–37.
Article5. Hanley DF, Thompson RE, Rosenblum M, Yenokyan G, Lane K, McBee N, et al. Efficacy and safety of minimally invasive surgery with thrombolysis in intracerebral haemorrhage evacuation (MISTIE III): a randomised, controlled, open-label, blinded endpoint phase 3 trial. Lancet. 2019; Mar. 393(10175):1021–32.6. Hemphill JC 3rd, Greenberg SM, Anderson CS, Becker K, Bendok BR, Cushman M, et al. Guidelines for the Management of Spontaneous Intracerebral Hemorrhage: A Guideline for Healthcare Professionals from the American Heart Association/American Stroke Association. Stroke. 2015; Jul. 46(7):2032–60.7. Keep RF, Hua Y, Xi G. Intracerebral haemorrhage: mechanisms of injury and therapeutic targets. Lancet Neurol. 2012; Aug. 11(8):720–31.
Article8. Mendelow AD, Gregson BA, Fernandes HM, Murray GD, Teasdale GM, Hope DT, et al. Early surgery versus initial conservative treatment in patients with spontaneous supratentorial intracerebral haematomas in the International Surgical Trial in Intracerebral Haemorrhage (STICH): a randomised trial. Lancet. 2005; Jan. 365(9457):387–97.
Article9. Mendelow AD, Gregson BA, Rowan EN, Murray GD, Gholkar A, Mitchell PM. Early surgery versus initial conservative treatment in patients with spontaneous supratentorial lobar intracerebral haematomas (STICH II): a randomised trial. Lancet. 2013; Aug. 382(9890):397–408.
Article10. Miki K, Yagi K, Nonaka M, Iwaasa M, Abe H, Morishita T, et al. Spot sign as a predictor of rebleeding after endoscopic surgery for intracerebral hemorrhage. J Neurosurg. 2019; May. 130(5):1485–90.
Article11. Mould WA, Carhuapoma JR, Muschelli J, Lane K, Morgan TC, McBee NA, et al. Minimally invasive surgery plus recombinant tissue-type plasminogen activator for intracerebral hemorrhage evacuation decreases perihematomal edema. Stroke. 2013; Mar. 44(3):627–34.
Article12. Nam TM, Kim YZ. A meta-analysis for evaluating efficacy of neuroendoscopic surgery versus craniotomy for supratentorial hypertensive intracerebral hemorrhage. J Cerebrovasc Endovasc Neurosurg. 2019; Mar. 21(1):11–7.
Article13. Newell DW, Shah MM, Wilcox R, Hansmann DR, Melnychuk E, Muschelli J, et al. Minimally invasive evacuation of spontaneous intracerebral hemorrhage using sonothrombolysis. J Neurosurg. 2011; Sep. 115(3):592–601.
Article14. Ren Y, Zheng J, Liu X, Li H, You C. Risk factors of rehemorrhage in postoperative patients with spontaneous intracerebral hemorrhage: a case-control study. J Korean Neurosurg Soc. 2018; Jan. 61(1):35–41.15. Sun S, Li Y, Zhang H, Gao H, Zhou X, Xu Y, et al. Neuroendoscopic surgery versus craniotomy for supratentorial hypertensive intracerebral hemorrhage: a systematic review and meta-analysis. World Neurosurg. 2020; Feb. 134:477–88.
Article16. Tang Y, Yin F, Fu D, Gao X, Lv Z, Li X. Efficacy and safety of minimal invasive surgery treatment in hypertensive intracerebral hemorrhage: a systematic review and meta-analysis. BMC Neurol. 2018; Sep. 18(1):136.
Article17. Uyttenboogaart M, Stewart RE, Vroomen PC, De Keyser J, Luijckx GJ. Optimizing cutoff scores for the Barthel index and the modified Rankin scale for defining outcome in acute stroke trials. Stroke. 2005; Sep. 36(9):1984–7.
Article18. Vespa PM, Martin N, Zuccarello M, Awad I, Hanley DF. Surgical trials in intracerebral hemorrhage. Stroke. 2013; Jun. 44(6 Suppl 1):S79–82.
Article19. Wada R, Aviv RI, Fox AJ, Sahlas DJ, Gladstone DJ, Tomlinson G, et al. CT angiography “spot sign” predicts hematoma expansion in acute intracerebral hemorrhage. Stroke. 2007; Apr. 38(4):1257–62.
Article20. Sirh S, Park HR. Optimal surgical timing of aspiration for spontaneous supratentorial intracerebral hemorrhage. J Cerebrovasc Endovasc Neurosurg. 2018; Jun. 20(2):96–105.
Article21. Wu TY, Sharma G, Strbian D, Putaala J, Desmond PM, Tatlisumak T, et al. Natural history of perihematomal edema and impact on outcome after intracerebral hemorrhage. Stroke. 2017; Apr. 48(4):873–9.
Article22. Xia Z, Wu X, Li J, Liu Z, Chen F, Zhang L, et al. Minimally invasive surgery is superior to conventional craniotomy in patients with spontaneous supratentorial intracerebral hemorrhage: a systematic review and meta-analysis. World Neurosurg. 2018; Jul. 115:266–73.
Article23. Yao Z, Hu X, You C, He M. Effect and feasibility of endoscopic surgery in spontaneous intracerebral hemorrhage: a systematic review and meta-analysis. World Neurosurg. 2018; May. 113:348–56.e2.
Article24. Zhou X, Chen J, Li Q, Ren G, Yao G, Liu M, et al. Minimally invasive surgery for spontaneous supratentorial intracerebral hemorrhage: a meta-analysis of randomized controlled trials. Stroke. 2012; Nov. 43(11):2923–30.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Optimal Surgical Timing of Aspiration for Spontaneous Supratentorial Intracerebral Hemorrhage
- The Management of Spontaneous Intracerebral Hemorrhage: Medical Versus Surgical Therapy for Spontaneous Intracerebral Hemorrhage
- A New Beginning for the Journal of Minimally Invasive Surgery for the International Recognition and Contribution of Scientific Development of Minimally Invasive Surgery
- Establishment of Minimally Invasive Thoracic Surgery Program
- Minimally Invasive Surgery for Esophageal Cancer