J Korean Med Sci.
2020 Sep;35(37):e313. 10.3346/jkms.2020.35.e313.
Blood Transfusion for Elderly Patients with Hip Fracture: a Nationwide Cohort Study
- Affiliations
-
- 1Department of Preventive Medicine, Eulji University School of Medicine, Daejeon, Korea
- 2Department of Orthopaedic Surgery, Eulji University Hospital, Daejeon, Korea
- 3Department of Orthopaedic Surgery, Gyeongsang National University Hospital, Jinju, Korea
- 4Department of Orthopaedic Surgery, Ajou University Medical Center, Suwon, Korea
- 5Department of Orthopaedic Surgery, Yeungnam University Medical Center, Daegu, Korea
- 6Department of Orthopedic Surgery, Chung-Ang University College of Medicine, Seoul, Korea
- 7Department of Orthopedic Surgery, Chung-Ang University College of Medicine, Seoul, Korea
- KMID: 2506562
- DOI: http://doi.org/10.3346/jkms.2020.35.e313
Abstract
- Background
This nationwide study aimed to investigate the blood transfusion status of elderly hip fracture patients and to examine the effect of packed red blood cell transfusion on all-cause mortality.
Methods
From the Korean National Health Insurance Service-Senior cohort consisting of 588,147 participants aged over 60 years in 2002, a total of 14,744 new-onset hip fracture patients aged 65–99 years were followed up for 11 years. The adjusted hazard ratios (aHRs), risk ratios, and their 95% confidence intervals were estimated by the Cox proportional hazard model and Poisson regression model.
Results
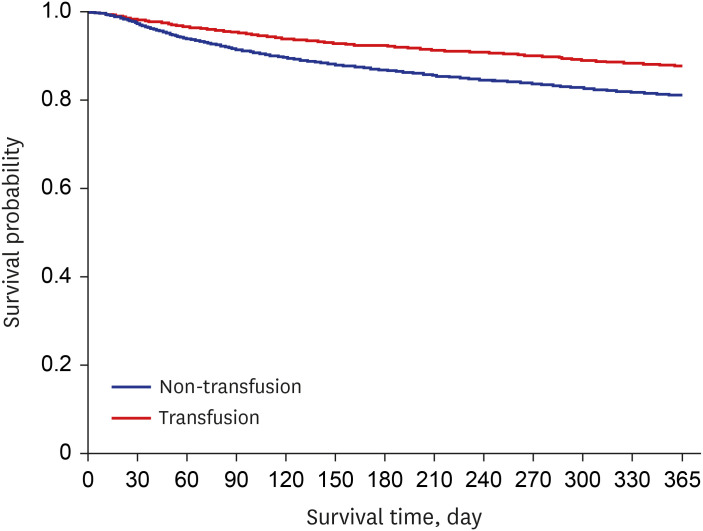
There were 10,973 patients (74.42%) in the transfusion group and 3,771 (25.58%) patients in the non-transfusion group. The mean volume of blood transfusion was 1,164.51 mL (± 865.25; median, 800 mL; interquartile range, 640–1,440). In the multivariable-adjusted Cox proportional hazard model, the transfusion group had 1.34-fold more risk of all-cause mortality than the non-transfusion group (aHR, 1.34; 95% confidence interval [CI], 1.26–1.42). In the multivariate-adjusted Poisson regression model, hip fracture patients in the transfusion group were 1.43 (adjusted risk ratio [aRR], 1.43; 95% CI, 1.09–1.87; p = 0.009) folds more likely to die within 30 days than those in the non-transfusion group. The mortality risk was highest at 90 days (aRR, 1.64; 95% CI, 1.40–1.93; p < 0.001) and slightly decreased at 180 days (aRR, 1.58; 95% CI, 1.40–1.79; p < 0.001) and 1 year (aRR, 1.43; 95% CI, 1.31–1.58; p < 0.001).
Conclusion
In this nationwide representative cohort study, blood transfusion was performed in 75% of hip fracture patients. Even after adjusting for comorbidity and anticoagulant use, the postoperative results (hospitalization, mortality) of the transfusion group did not show significantly worse results than the non-transfusion group. Therefore, adequate patient blood management can only improve the patient's outcome after hip fracture surgery.
Figure
Cited by 1 articles
-
Effect of a Patient Blood Management Program on the Appropriateness of Red Blood Cell Transfusion and Clinical Outcomes in Elderly Patients Undergoing Hip Fracture Surgery
Jong Hun Kim, Hyeon Ju Shin, Hae Sun You, Yoonsun Park, Ki Hoon Ahn, Jae Seung Jung, Seung-Beom Han, Jong Hoon Park,
J Korean Med Sci. 2023;38(8):e64. doi: 10.3346/jkms.2023.38.e64.
Reference
-
1. Napolitano LM, Kurek S, Luchette FA, Anderson GL, Bard MR, Bromberg W, et al. Clinical practice guideline: red blood cell transfusion in adult trauma and critical care. J Trauma. 2009; 67(6):1439–1442. PMID: 20009700.
Article2. Morris R, Rethnam U, Russ B, Topliss C. Assessing the impact of fracture pattern on transfusion requirements in hip fractures. Eur J Trauma Emerg Surg. 2017; 43(3):337–342. PMID: 26972432.
Article3. Shander A, Hofmann A, Isbister J, Van Aken H. Patient blood management--the new frontier. Best Pract Res Clin Anaesthesiol. 2013; 27(1):5–10. PMID: 23590911.4. Sambandam B, Batra S, Gupta R, Agrawal N. Blood conservation strategies in orthopedic surgeries: a review. J Clin Orthop Trauma. 2013; 4(4):164–170. PMID: 26403876.
Article5. Chen X, Mao G, Leng SX. Frailty syndrome: an overview. Clin Interv Aging. 2014; 9:433–441. PMID: 24672230.6. Smith RW, Freeston IL, Brown BH. A real-time electrical impedance tomography system for clinical use--design and preliminary results. IEEE Trans Biomed Eng. 1995; 42(2):133–140. PMID: 7868140.
Article7. Beal EW, Bagante F, Paredes A, Akgul O, Merath K, Cua S, et al. Perioperative use of blood products is associated with risk of morbidity and mortality after surgery. Am J Surg. 2019; 218(1):62–70. PMID: 30509453.
Article8. Bernard AC, Davenport DL, Chang PK, Vaughan TB, Zwischenberger JB. Intraoperative transfusion of 1 U to 2 U packed red blood cells is associated with increased 30-day mortality, surgical-site infection, pneumonia, and sepsis in general surgery patients. J Am Coll Surg. 2009; 208(5):931–937. PMID: 19476865.
Article9. Ferraris VA, Davenport DL, Saha SP, Austin PC, Zwischenberger JB. Surgical outcomes and transfusion of minimal amounts of blood in the operating room. Arch Surg. 2012; 147(1):49–55. PMID: 22250113.
Article10. Tinmouth AT, McIntyre LA, Fowler RA. Blood conservation strategies to reduce the need for red blood cell transfusion in critically ill patients. CMAJ. 2008; 178(1):49–57. PMID: 18166731.
Article11. Glassou EN, Kristensen N, Møller BK, Erikstrup C, Hansen TB, Pedersen AB. Impact of preadmission anti-inflammatory drug use on the risk of RBC transfusion in elderly hip fracture patients: a Danish nationwide cohort study, 2005–2016. Transfusion. 2019; 59(3):935–944. PMID: 30610758.
Article12. Xiao C, Zhang S, Long N, Yu W, Jiang Y. Is intravenous tranexamic acid effective and safe during hip fracture surgery? An updated meta-analysis of randomized controlled trials. Arch Orthop Trauma Surg. 2019; 139(7):893–902. PMID: 30637503.
Article13. Kadar A, Chechik O, Steinberg E, Reider E, Sternheim A. Predicting the need for blood transfusion in patients with hip fractures. Int Orthop. 2013; 37(4):693–700. PMID: 23381612.
Article14. Park JH, Kim HS, Yoo JH, Kim JH, Sung KH, Kim JY, et al. Perioperative blood loss in bipolar hemiarthroplasty for femoral neck fracture: analysis of risk factors. Hip Pelvis. 2013; 25(2):110–114.
Article15. Seong SC, Kim YY, Park SK, Khang YH, Kim HC, Park JH, et al. Cohort profile: the National Health Insurance Service-National Health Screening Cohort (NHIS-HEALS) in Korea. BMJ Open. 2017; 7(9):e016640.
Article16. Lee J, Lee JS, Park SH, Shin SA, Kim K. Cohort profile: the national health insurance service–national sample cohort (NHIS-NSC), South Korea. Int J Epidemiol. 2017; 46(2):e15. PMID: 26822938.
Article17. Park C, Jang S, Jang S, Ha YC, Lee YK, Yoon HK, et al. Identification and validation of osteoporotic hip fracture using the national health insurance database. J Korean Hip Soc. 2010; 22(4):305–311.
Article18. Lee YK, Ha YC, Choi HJ, Jang S, Park C, Lim YT, et al. Bisphosphonate use and subsequent hip fracture in South Korea. Osteoporos Int. 2013; 24(11):2887–2892. PMID: 23681088.
Article19. Jang SY, Cha YH, Mun YS, Kim SH, Kim HY, Choy WS. Acute cholecystitis in elderly patients after hip fracture: a nationwide cohort study. J Korean Med Sci. 2019; 34(5):e36. PMID: 30718989.
Article20. Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005; 43(11):1130–1139. PMID: 16224307.
Article21. Kanis JA, Odén A, McCloskey EV, Johansson H, Wahl DA, Cooper C, et al. A systematic review of hip fracture incidence and probability of fracture worldwide. Osteoporos Int. 2012; 23(9):2239–2256. PMID: 22419370.
Article22. Lee YK, Kim JW, Lee MH, Moon KH, Koo KH. Trend in the age-adjusted incidence of hip fractures in South Korea: systematic review. Clin Orthop Surg. 2017; 9(4):420–423. PMID: 29201294.
Article23. Schilling PL, Hallstrom BR, Birkmeyer JD, Carpenter JE. Prioritizing perioperative quality improvement in orthopaedic surgery. J Bone Joint Surg Am. 2010; 92(9):1884–1889. PMID: 20686063.
Article24. Lawrence VA, Silverstein JH, Cornell JE, Pederson T, Noveck H, Carson JL. Higher Hb level is associated with better early functional recovery after hip fracture repair. Transfusion. 2003; 43(12):1717–1722. PMID: 14641869.
Article25. Foss NB, Kristensen MT, Kehlet H. Anaemia impedes functional mobility after hip fracture surgery. Age Ageing. 2008; 37(2):173–178. PMID: 18349013.
Article26. Willems JM, de Craen AJ, Nelissen RG, van Luijt PA, Westendorp RG, Blauw GJ. Haemoglobin predicts length of hospital stay after hip fracture surgery in older patients. Maturitas. 2012; 72(3):225–228. PMID: 22525146.
Article27. Engoren M, Mitchell E, Perring P, Sferra J. The effect of erythrocyte blood transfusions on survival after surgery for hip fracture. J Trauma. 2008; 65(6):1411–1415. PMID: 19077635.
Article28. Ashworth A, Klein AA. Cell salvage as part of a blood conservation strategy in anaesthesia. Br J Anaesth. 2010; 105(4):401–416. PMID: 20802228.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The incidence of hip fracture and mortality rate after hip fracture in Korea: A nationwide population-based cohort study
- Acute Cholecystitis in Elderly Patients after Hip Fracture: a Nationwide Cohort Study
- Effect of Opioids on All-cause Mortality and Sustained Opioid Use in Elderly Patients with Hip Fracture: a Korea Nationwide Cohort Study
- The Prevalence of Clostridium difficile Colitis and Effect on All-Cause Mortality in Elderly Patients after Hip Fracture Surgery: A Korean Nationwide Cohort Study
- Patient Blood Management in Hip Replacement Arthroplasty