Obstet Gynecol Sci.
2020 Sep;63(5):586-593. 10.5468/ogs.20061.
Management of isolated oligohydramnios in Korea: a questionnaire-based study of clinical practice patterns among the members of the Korean Society of Maternal Fetal Medicine
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Research Institute of Medical Science, Konkuk University School of Medicine, Seoul, Korea
- 2Department of Obstetrics and Gynecology, Ilsan Paik Hospital, Inje University College of Medicine, Goyang, Korea
- KMID: 2506501
- DOI: http://doi.org/10.5468/ogs.20061
Abstract
Objective
The aim of this survey was to investigate the recommendations and clinical practice patterns of the Korean Society of Maternal and Fetal Medicine (KSMFM) members, regarding management of isolated oligohydramnios (IO).
Methods
From December 2018 to February 2019, questionnaires were e-mailed to the KSMFM members at 257 institutes that are listed by the Korean Statistical Information Services (KOSIS) as suitable labor premises. Responses to the seven questions on the management of IO, from diagnosis to treatment, were evaluated.
Results
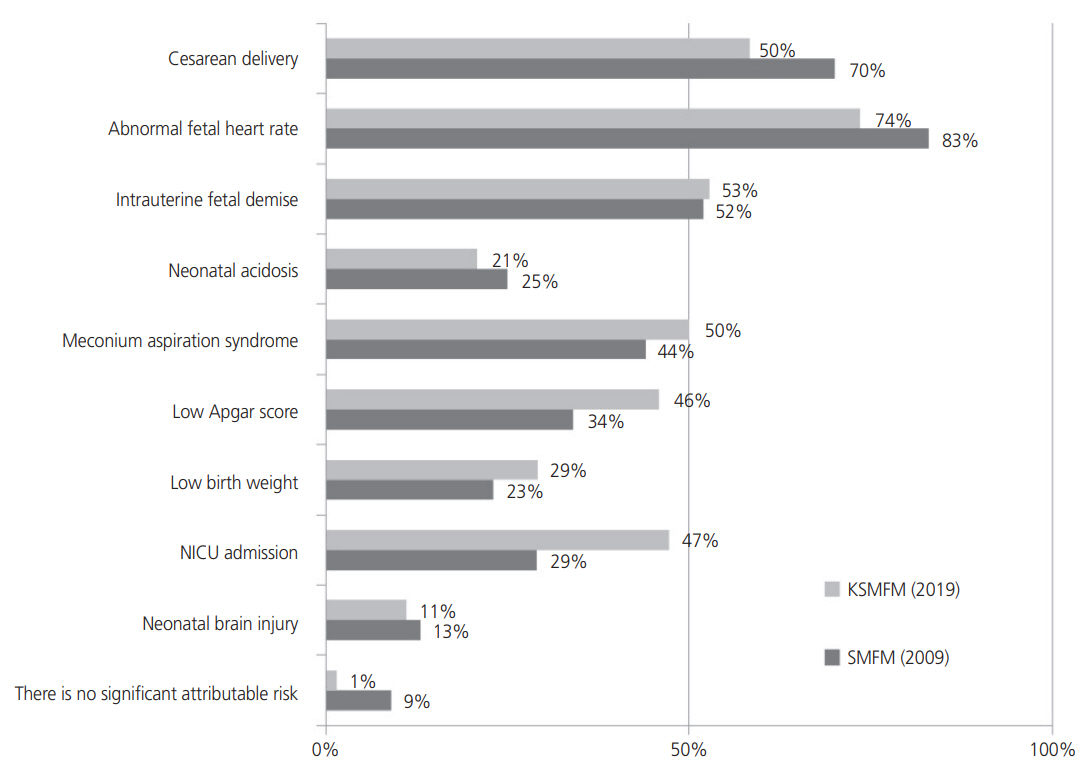
A total of 72 KSMFM members responded to this survey. Nearly all participants (90.1%) used the amniotic fluid index (AFI) as the primary method for estimating amniotic fluid volume. The majority of the participants (73.6%) believed that IO was a risk factor for adverse pregnancy outcomes, including abnormal fetal heart rate (73.6%), need for cesarean delivery (58.3%), intrauterine fetal demise (52.8%), and meconium aspiration syndrome (50%). Almost 70% of the participants believed that induction of labor might decrease perinatal morbidities, and that late-preterm to early-term period (36–38 gestational weeks) was a suitable timeframe for delivery, if the fetus was sufficiently grown and antenatal testing revealed reassuring results. Less than half of the participants (47.2%) believed that maternal oral or intravenous hydration was a useful intervention for IO management.
Conclusions
KSMFM members preferred labor induction at late-preterm to early-term, to decrease perinatal morbidity in cases of IO, although it was still uncertain whether labor induction improved the outcomes. Further prospective studies are needed regarding IO management.
Figure
Reference
-
References
1. Dubil EA, Magann EF. Amniotic fluid as a vital sign for fetal wellbeing. Australas J Ultrasound Med. 2013; 16:62–70.
Article2. Timor-Tritsch IE, Farine D, Rosen MG. A close look at early embryonic development with the high-frequency transvaginal transducer. Am J Obstet Gynecol. 1988; 159:676–81.
Article3. Chauhan SP, Cowan BD, Magann EF, Roberts WE, Morrison JC, Martin JN Jr. Intrapartum amniotic fluid index. A poor diagnostic test for adverse perinatal outcome. J Reprod Med. 1996; 41:860–6.4. Chauhan SP, Sanderson M, Hendrix NW, Magann EF, Devoe LD. Perinatal outcome and amniotic fluid index in the antepartum and intrapartum periods: a metaanalysis. Am J Obstet Gynecol. 1999; 181:1473–8.
Article5. Rossi AC, Prefumo F. Perinatal outcomes of isolated oligohydramnios at term and post-term pregnancy: a systematic review of literature with meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2013; 169:149–54.
Article6. Zhang J, Troendle J, Meikle S, Klebanoff MA, Rayburn WF. Isolated oligohydramnios is not associated with adverse perinatal outcomes. BJOG. 2004; 111:220–5.
Article7. Rabie N, Magann E, Steelman S, Ounpraseuth S. Oligohydramnios in complicated and uncomplicated pregnancy: a systematic review and meta-analysis. Ultrasound Obstet Gynecol. 2017; 49:442–9.
Article8. Gizzo S, Noventa M, Vitagliano A, Dall’Asta A, D’Antona D, Aldrich CJ, et al. An update on maternal hydration strategies for amniotic fluid improvement in isolated oligohydramnios and normohydramnios: evidence from a systematic review of literature and meta-analysis. PLoS One. 2015; 10:e0144334.
Article9. Schwartz N, Sweeting R, Young BK, Schwartz N, Sweeting R, Young BK. Practice patterns in the management of isolated oligohydramnios: a survey of perinatologists. J Matern Fetal Neonatal Med. 2009; 22:357–61.
Article10. Shrem G, Nagawkar SS, Hallak M, Walfisch A. Isolated oligohydramnios at term as an indication for labor induction: a systematic review and meta-analysis. Fetal Diagn Ther. 2016; 40:161–73.
Article11. Peipert JF, Donnenfeld AE. Oligohydramnios: a review. Obstet Gynecol Surv. 1991; 46:325–39.12. Munn MB. Management of oligohydramnios in pregnancy. Obstet Gynecol Clin North Am. 2011; 38:387–95.
Article13. Mayer A, Erez O, Novack L, Bashiri A, Wiznitzer A, Mazor M. Chronic hypertension is an independent risk factor for preeclampsia and preterm delivery in women with rheumatologic diseases: a population-based study. Eur J Obstet Gynecol Reprod Biol. 2007; 133:157–63.
Article14. Brzezinski-Sinai NA, Stavsky M, Rafaeli-Yehudai T, Yitshak-Sade M, Brzezinski-Sinai I, Imterat M, et al. Induction of labor in cases of late preterm isolated oligohydramnios: is it justified? J Matern Fetal Neonatal Med. 2019; 32:2271–9.
Article15. Charles D, Jacoby HE. Preliminary data on the use of sodium aminohippurate to determine amniotic fluid volumes. Am J Obstet Gynecol. 1966; 95:266–9.
Article16. Rosati P, Guariglia L, Cavaliere AF, Ciliberti P, Buongiorno S, Ciardulli A, et al. A comparison between amniotic fluid index and the single deepest vertical pocket technique in predicting adverse outcome in prolonged pregnancy. J Prenat Med. 2015; 9:12–5.
Article17. Magann EF, Nolan TE, Hess LW, Martin RW, Whitworth NS, Morrison JC. Measurement of amniotic fluid volume: accuracy of ultrasonography techniques. Am J Obstet Gynecol. 1992; 167:1533–7.
Article18. Rutherford SE, Smith CV, Phelan JP, Kawakami K, Ahn MO. Four-quadrant assessment of amniotic fluid volume. Interobserver and intraobserver variation. J Reprod Med. 1987; 32:587–9.19. Nabhan AF, Abdelmoula YA. Amniotic fluid index versus single deepest vertical pocket: a meta-analysis of randomized controlled trials. Int J Gynaecol Obstet. 2009; 104:184–8.
Article20. Ashwal E, Hiersch L, Melamed N, Aviram A, Wiznitzer A, Yogev Y. The association between isolated oligohydramnios at term and pregnancy outcome. Arch Gynecol Obstet. 2014; 290:875–81.
Article21. ACOG Committee opinion No. 764 summary: medically indicated late-preterm and early-term deliveries. Obstet Gynecol. 2019; 133:400–3.22. Moore TR. The role of amniotic fluid assessment in indicated preterm delivery. Semin Perinatol. 2011; 35:286–91.
Article23. Jo JH, Choi YH, Wie JH, Ko HS, Park IY, Shin JC. Fetal Doppler to predict cesarean delivery for non-reassuring fetal status in the severe small-for-gestational-age fetuses of late preterm and term. Obstet Gynecol Sci. 2018; 61:202–8.
Article24. Oh SY. Management of isolated oligohydramnios between 34+0 and 36+6 weeks of gestation. Korean J Perinatol. 2013; 24:229–36.25. Hofmeyr GJ, Gülmezoglu AM, Novikova N. Maternal hydration for increasing amniotic fluid volume in oligohydramnios and normal amniotic fluid volume. Cochrane Database Syst Rev. 2002; (1):CD000134.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Management of Isolated Oligohydramnios between 34(+0) and 36(+6) Weeks of Gestation
- The Isolated Oligohydramnios
- A Case of Multiple Placental Chorioangioma Combined with Oligohydramnios
- The practice patterns of second trimester fetal ultrasonography: A questionnaire survey and an analysis of checklists
- Autopsy Findings in Fetuses with Oligohydramnios