J Vet Sci.
2020 Mar;21(2):e27. 10.4142/jvs.2020.21.e27.
Clinical assessment of the efficacy of supraglottic airway devices compared with endotracheal tubes in cats during volume-controlled ventilation
- Affiliations
-
- 1Surgery Unit, Kasetsart University Veterinary Teaching Hospital, Bangkok 10900, Thailand
- 2Department of Companion Animal Clinical Sciences, Kasetsart University, Bangkok 10900, Thailand
- KMID: 2506188
- DOI: http://doi.org/10.4142/jvs.2020.21.e27
Abstract
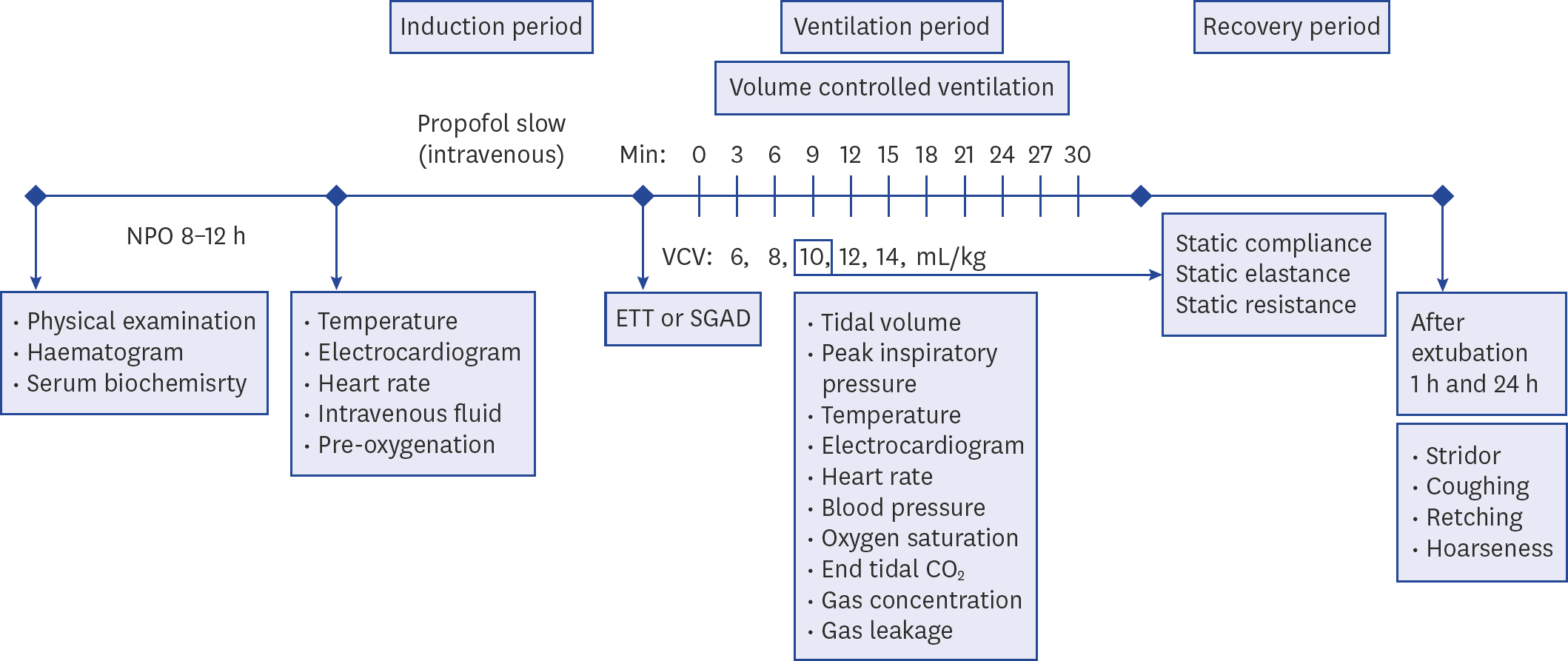
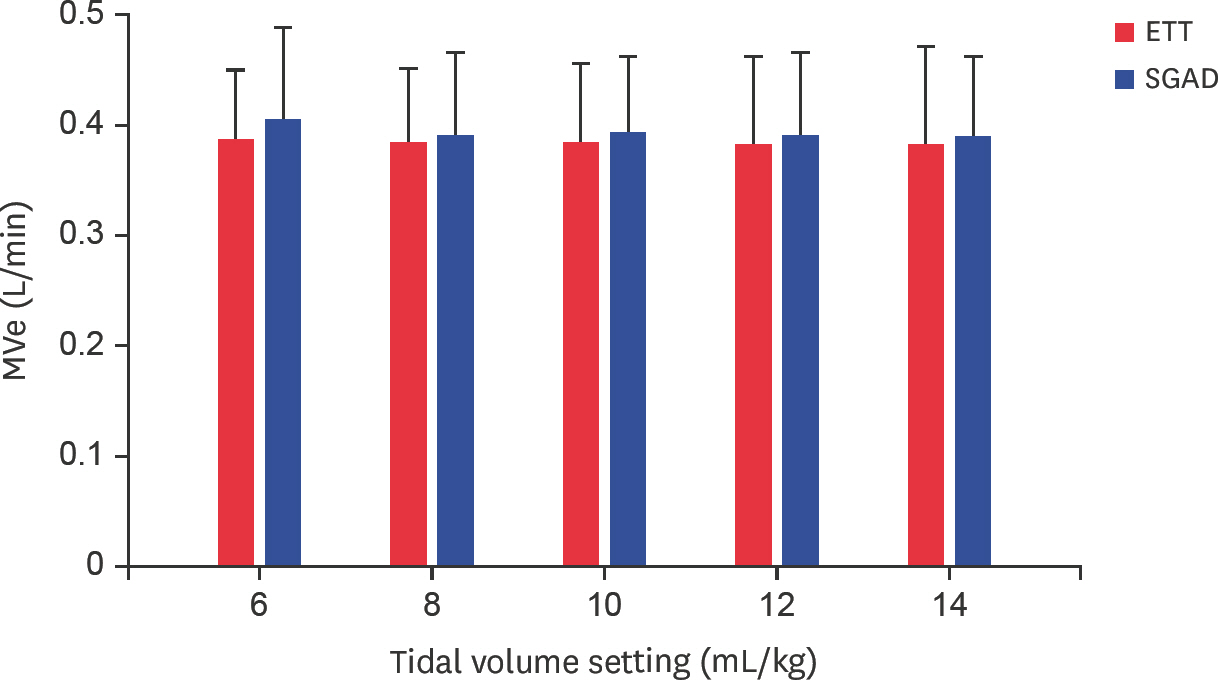
- The efficacies of a supraglottic airway device (SGAD) and an endotracheal tube (ETT) in cats under general anesthesia with volume-controlled ventilation (VCV) were compared. Thirty healthy cats were randomly allocated for airway control using either an SGAD or an ETT. Five tidal volumes (6, 8, 10, 12, and 14 mL/kg) were randomly tested, and respiratory rates were adjusted to achieve a minute ventilation of 100 mL/kg/min. The dose of propofol necessary to insert the SGAD or ETT, the static respiratory pressure, leakage during VCV, and end tidal CO2 (ETCO2 ) were recorded. Dosages of propofol and static respiratory measurements for the SGAD and ETT groups were compared using a t-test. The distribution of leakages and hypercapnia (ETCO2> 45 mmHg) were compared using Fisher's exact test. A significance level ofp < 0.05 was established. No significant difference in dose of propofol was observed between the SGAD and ETT groups (7.1 ± 1.0, 7.3 ± 1.7 mg/kg; p = 0.55). Static resistance pressure of the SGAD (22.0 ± 8.1 cmH 2 O/L/sec) was significantly lower than that of the ETT (36.6 ± 12.9 cmH 2 O/L/sec; p < 0.01). Of the 75 trials, leakage was more frequent when using an SGAD (8 events) than when using an ETT (1 event; p = 0.03). Hypercapnia occurred more frequently with SGAD (18 events) than with ETT (3 events;p< 0.01). Although intubation with an ETT is the gold standard in small animal anesthesia, the use of an SGAD can reduce airway resistance and the work of breathing. Nonetheless, SGAD had more dead space and the tidal volume for VCV needs adjustment.
Keyword
Figure
Reference
-
References
1. van Oostrom H, Krauss MW, Sap R. A comparison between the v-gel supraglottic airway device and the cuffed endotracheal tube for airway management in spontaneously breathing cats during isoflurane anaesthesia. Vet Anaesth Analg. 2013; 40:265–271.
Article2. Hofmeister EH, Trim CM, Kley S, Cornell K. Traumatic endotracheal intubation in the cat. Vet Anaesth Analg. 2007; 34:213–216.
Article3. Prasse SA, Schrack J, Wenger S, Mosing M. Clinical evaluation of the v-gel supraglottic airway device in comparison with a classical laryngeal mask and endotracheal intubation in cats during spontaneous and controlled mechanical ventilation. Vet Anaesth Analg. 2016; 43:55–62.
Article4. Brodbelt D. Feline anesthetic deaths in veterinary practice. Top Companion Anim Med. 2010; 25:189–194.
Article5. Brodbelt DC, Pfeiffer DU, Young LE, Wood JL. Risk factors for anaesthetic-related death in cats: results from the confidential enquiry into perioperative small animal fatalities (CEPSAF). Br J Anaesth. 2007; 99:617–623.6. Mitchell SL, McCarthy R, Rudloff E, Pernell RT. Tracheal rupture associated with intubation in cats: 20 cases (1996–1998). J Am Vet Med Assoc. 2000; 216:1592–1595.
Article7. Hardie EM, Spodnick GJ, Gilson SD, Benson JA, Hawkins EC. Tracheal rupture in cats: 16 cases (1983–1998). J Am Vet Med Assoc. 1999; 214:508–512.8. Costanzo LS. Physiology. 1st ed.Williams & Wilkins;Philadelphia: 1995.9. Crotaz IR. Initial feasibility investigation of the v-gel airway: an anatomically designed supraglottic airway device for use in companion animal veterinary anaesthesia. Vet Anaesth Analg. 2010; 37:579–580.
Article10. Toman H, Erbas M, Kiraz HA, Sahin H, Ovali MA, Uzun M. Comparison of effects of classic LMA, cobraPLA and V-gel rabbit on QTc interval. Bratisl Lek Listy. 2015; 116:632–636.
Article11. Muir WW, Hubbell JA, Bednarski RM, Skarda RT. Handbook of Veterinary Anesthesia. 4th ed.Elsevier Inc.;St. Louis: 2007.12. Mosley CA. Lumb & Jones'Veterinary Anesthesia and Analgesia. 5th ed.John Wiley & Sons;Inc., Pondicherry: 2015.13. West JB, Luks AM. West's Respiratory Physiology: The Essentials. 10th ed.Wolters Kluwer;Philadelphia: 2016.14. Thengchaisri N, Steiner JM, Suchodolski JS, Sattasathuchana P. Association of gingivitis with dental calculus thickness or dental calculus coverage and subgingival bacteria in feline leukemia virus- and feline immunodeficiency virus-negative cats. Can J Vet Res. 2017; 81:46–52.15. Gurney M, Cripps P, Mosing M. Subcutaneous pre-anaesthetic medication with acepromazine-buprenorphine is effective as and less painful than the intramuscular route. J Small Anim Pract. 2009; 50:474–477.
Article16. Ko J. Small Animal Anesthesia and Pain Management: a Color Handbook. 1st ed.Manson Publishing Ltd.;London: 2013.17. Ramsey I. BSAVA Small Animal Formulary. 6th ed.British Small Animal Veterinary Association;Wales: 2008.18. Cassu RN, Luna SP, Teixeira Neto FJ, Braz JR, Gasparini SS, Crocci AJ. Evaluation of laryngeal mask as an alternative to endotracheal intubation in cats anesthetized under spontaneous or controlled ventilation. Vet Anaesth Analg. 2004; 31:213–221.
Article19. Nseir S, Brisson H, Marquette CH, Chaud P, Di Pompeo C, Diarra M, Durocher A. Variations in endotracheal cuff pressure in intubated critically ill patients: prevalence and risk factors. Eur J Anaesthesiol. 2009; 26:229–234.
Article20. White DM, Redondo JI, Mair AR, Martinez-Taboada F. The effect of user experience and inflation technique on endotracheal tube cuff pressure using a feline airway simulator. Vet Anaesth Analg. 2017; 44:1076–1084.
Article21. Pennant JH, White PF. The laryngeal mask airway. Its uses in anesthesiology. Anesthesiology. 1993; 79:144–163.22. Bansal SC, Caoci S, Dempsey E, Trevisanuto D, Roehr CC. The laryngeal mask airway and its use in neonatal resuscitation: a critical review of where we are in 2017/2018. Neonatology. 2018; 113:152–161.
Article23. Thomas JA, Lerche P. Anesthesia and Analgesia for Veterinary Technicians. 5th ed.Elsevier Health Sciences;Philadelphia: 2016.24. Barletta M, Kleine SA, Quandt JE. Assessment of v-gel supraglottic airway device placement in cats performed by inexperienced veterinary students. Vet Rec. 2015; 177:523.
Article25. Keidan I, Berkenstadt H, Segal E, Perel A. Pressure versus volume-controlled ventilation with a laryngeal mask airway in paediatric patients. Paediatr Anaesth. 2001; 11:691–694.26. Dassios T, Dixon P, Hickey A, Fouzas S, Greenough A. Physiological and anatomical dead space in mechanically ventilated newborn infants. Pediatr Pulmonol. 2018; 53:57–63.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Safety and clinical usefulness of supraglottic airway device
- Comparison of the Clinical Effectiveness of the CobraTM Perilaryngeal Airway and the ProSealTM Laryngeal Mask Airway during Anesthesia with Controlled Ventilation
- Use of the i-gel(TM) supraglottic airway device in a patient with subglottic stenosis: a case report
- Comparison of the CobraPLA and the LMA Classic airway devices during volume-controlled ventilation in children
- Airway Management