J Korean Neurosurg Soc.
2020 Sep;63(5):649-656. 10.3340/jkns.2020.0171.
Missed Skeletal Trauma Detected by Whole Body Bone Scan in Patients with Traumatic Brain Injury
- Affiliations
-
- 1Department of Neurosurgery, 1 Yonsei University Wonju College of Medicine, Wouju, Korea
- 2Department of Neurosurgery, 2 Yonsei University College of Medicine, Seoul, Korea
- KMID: 2506029
- DOI: http://doi.org/10.3340/jkns.2020.0171
Abstract
Objective
: Unclear mental state is one of the major factors contributing to diagnostic failure of occult skeletal trauma in patients with traumatic brain injury (TBI). The aim of this study was to evaluate the overlooked co-occurring skeletal trauma through whole body bone scan (WBBS) in TBI.
Methods
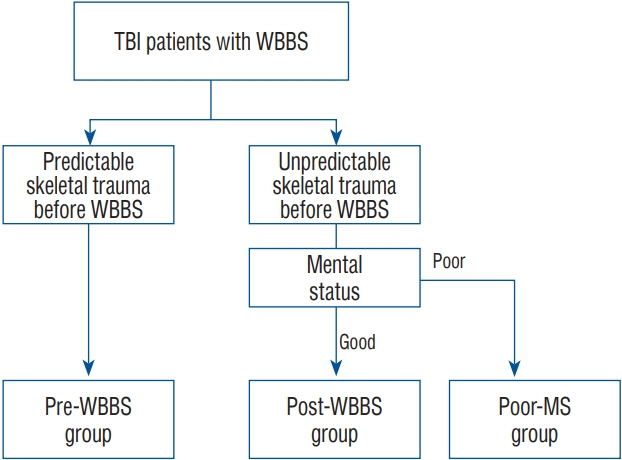
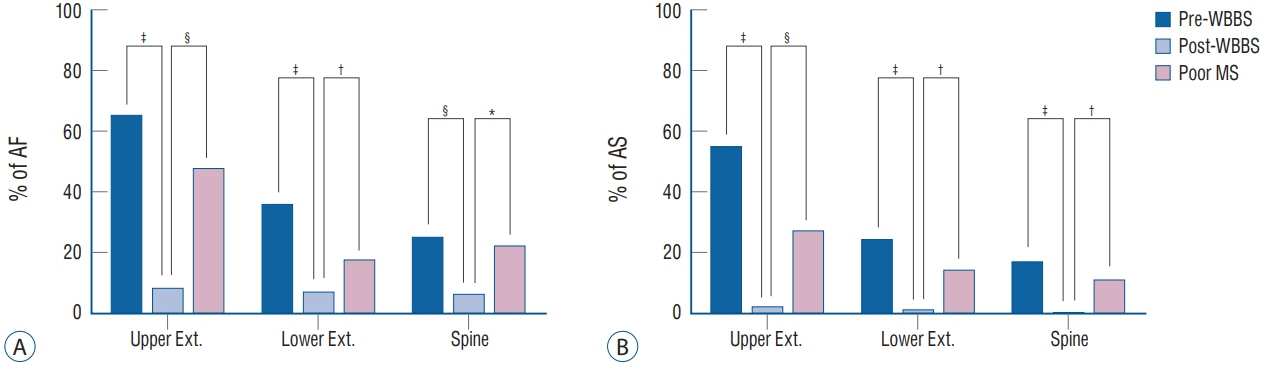
: A retrospective study of 547 TBI patients admitted between 2015 and 2017 was performed to investigate their cooccurring skeletal injuries detected by WBBS. The patients were divided into three groups based on the timing of suspecting skeletal trauma confirmed : 1) before WBBS (pre-WBBS); 2) after the routine WBBS (post-WBBS) with good mental state and no initial musculoskeletal complaints; and 3) after the routine WBBS with poor mental state (poor MS). The skeletal trauma detected by WBBS was classified into six skeletal categories : spine, upper and lower extremities, pelvis, chest wall, and clavicles. The skeletal injuries identified by WBBS were confirmed to be simple contusion or fractures by other imaging modalities such as X-ray or computed tomography (CT) scans. Of the six categorizations of skeletal trauma detected as hot uptake lesions in WBBS, the lesions of spine, upper and lower extremities were further statistically analyzed to calculate the incidence rates of actual fractures (AF) and actual surgery (AS) cases over the total number of hot uptake lesions in WBBS.
Results
: Of 547 patients with TBI, 112 patients (20.4 %) were presented with TBI alone. Four hundred and thirty-five patients with TBI had co-occurring skeletal injuries confirmed by WBBS. The incidences were as follows : chest wall (27.4%), spine (22.9%), lower extremities (20.2%), upper extremities (13.5%), pelvis (9.4%), and clavicles (6.3%). It is notable that relatively larger number of positive hot uptakes were observed in the groups of post-WBBS and poor MS. The percentage of post-WBBS group over the total hot uptake lesions in upper and lower extremities, and spines were 51.0%, 43.8%, and 41.7%, respectively, while their percentages of AS were 2.73%, 1.1%, and 0%, respectively. The percentages of poor MS group in the upper and lower extremities, and spines were 10.4%, 17.4%, and 7.8%, respectively, while their percentages of AS were 26.7%, 14.2%, and 11.1%, respectively. There was a statistical difference in the percentage of AS between the groups of post-WBBS and poor MS (p=0.000).
Conclusion
: WBBS is a potential diagnostic tool in understanding the skeletal conditions of patients with head injuries which may be undetected during the initial assessment.
Figure
Reference
-
References
1. Bauer GC. The use of radionuclides in orthopaedics. Radionuclide scintimetry of the skeleton. 1968. Clin Orthop Relat Res. 287:3–12. 1993.2. Brooks A, Holroyd B, Riley B. Missed injury in major trauma patients. Injury. 35:407–410. 2004.
Article3. Deininger HK. Skeletal scintigraphy as an addition to the roentgenological examination in traumatology (author's transl). Radiologe. 21:35–45. 1981.4. Enderson BL, Maull KI. Missed injuries. The trauma surgeon's nemesis. Surg Clin North Am. 71:399–418. 1991.
Article5. Frawley PA, Mills JA, Murton F, Ware R. Bone scanning in the multiply injured patient. Aust N Z J Surg. 65:390–393. 1995.
Article6. Garland DE, Bailey S. Undetected injuries in head-injured adults. Clin Orthop Relat Res. 155:162–165. 1981.
Article7. George MP, Bixby S. Frequently missed fractures in pediatric trauma: a pictorial review of plain film radiography. Radiol Clin North Am. 57:843–855. 2019.8. Heinrich SD, Gallagher D, Harris M, Nadell JM. Undiagnosed fractures in severely injured children and young adults. Identification with technetium imaging. J Bone Joint Surg Am. 76:561–572. 1994.
Article9. Hirshberg A, Wall MJ Jr, Allen MK, Mattox KL. Causes and patterns of missed injuries in trauma. Am J Surg. 168:299–303. 1994.
Article10. Huang HC, Fu CY, Hsieh CH, Wang YC, Wu SC, Chen RJ, et al. Lodox/Statscan facilitates the early detection of commonly overlooked extracranial injuries in patients with traumatic brain injury. Eur J Trauma Emerg Surg. 38:319–326. 2012.
Article11. Janjua KJ, Sugrue M, Deane SA. Prospective evaluation of early missed injuries and the role of tertiary trauma survey. J Trauma. 44:1000–1007. 1998.
Article12. Kremli MK. Missed musculoskeletal injuries in a university hospital in Riyadh: types of missed injuries and responsible factors. Injury. 27:503–506. 1996.
Article13. Lee KJ, Jung K, Kim J, Kwon J. Bone scan as a screening test for missed fractures in severely injured patients. Orthop Traumatol Surg Res. 100:953–957. 2014.
Article14. Lee WC, Chen CW, Lin YK, Lin TY, Kuo LC, Cheng YC, et al. Association of head, thoracic and abdominal trauma with delayed diagnosis of coexisting injuries in critical trauma patients. Injury. 45:1429–1434. 2014.
Article15. Mackersie RC, Shackford SR, Garfin SR, Hoyt DB. Major skeletal injuries in the obtunded blunt trauma patient: a case for routine radiologic survey. J Trauma. 28:1450–1454. 1988.16. Mrozek S, Gaussiat F, Geeraerts T. The management of femur shaft fracture associated with severe traumatic brain injury. Ann Fr Anesth Reanim. 32:510–515. 2013.
Article17. Probst C, Pape HC, Hildebrand F, Regel G, Mahlke L, Giannoudis P, et al. 30 years of polytrauma care: an analysis of the change in strategies and results of 4849 cases treated at a single institution. Injury. 40:77–83. 2009.
Article18. Schmidt C, Deininger HK. The occult fracture in the roentgen picture and its detection using bone scintigraphy. Radiologe. 25:104–107. 1985.19. Sobus KM, Alexander MA, Harcke HT. Undetected musculoskeletal trauma in children with traumatic brain injury or spinal cord injury. Arch Phys Med Rehabil. 74:902–904. 1993.20. Soundappan SV, Holland AJ, Cass DT. Role of an extended tertiary survey in detecting missed injuries in children. J Trauma. 57:114–118. 2004.
Article21. Ward WG, Nunley JA. Occult orthopaedic trauma in the multiply injured patient. J Orthop Trauma. 5:308–312. 1991.
Article22. Wei CJ, Tsai WC, Tiu CM, Wu HT, Chiou HJ, Chang CY. Systematic analysis of missed extremity fractures in emergency radiology. Acta Radiol. 47:710–717. 2006.
Article23. Yang DC, Ratani RS, Mittal PK, Chua RS, Pate SM. Radionuclide threephase whole-body bone imaging. Clin Nucl Med. 27:419–426. 2002.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Analysis of Missed Fractures in Polytrauma Patients
- Whole Body Bone Scan for Detecting Missed Bone Injuries in Multiple Trauma Patients
- Incidental traumatic right diaphragmatic rupture: a missed case after trauma
- The Relationship of the Facial Injury Location and the Traumatic Brain Hemorrhage
- Missed Traumatic Cervical Spine Injury