J Korean Med Sci.
2020 Aug;35(34):e316. 10.3346/jkms.2020.35.e316.
Adverse Initial CT Findings Associated with Poor Prognosis of Coronavirus Disease
- Affiliations
-
- 1Department of Radiology, Keimyung University Dongsan Hospital, Keimyung University School of Medicine, Daegu, Korea
- 2Department of Radiology, Research Institute of Radiological Science, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- 3Department of Internal Medicine, Keimyung University Dongsan Hospital, Keimyung University School of Medicine, Daegu, Korea
- KMID: 2505728
- DOI: http://doi.org/10.3346/jkms.2020.35.e316
Abstract
- Background
The predictors of poor prognosis in patients with coronavirus disease 2019 (COVID-19) using computed tomography (CT) have not been investigated in a large cohort. Therefore, the purpose of this study was to investigate the adverse initial CT features to predict poor prognosis in COVID-19.
Methods
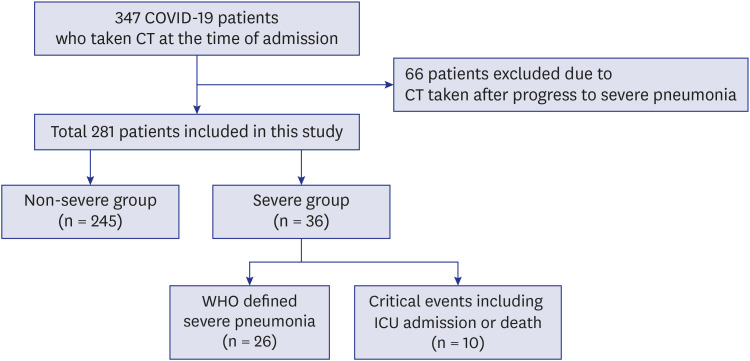
From February to April 2020, 281 COVID-19 patients who underwent CT at the time of admission were included. We divided the patients into the severe and non-severe disease groups. The severe group included patients with severe pneumonia or critical events. Intensive care unit admission or death were the critical events in this study. We compared the clinical and CT findings between the severe and non-severe groups and investigated the prognostic factors and critical events of the severe group using the regression analysis.
Results
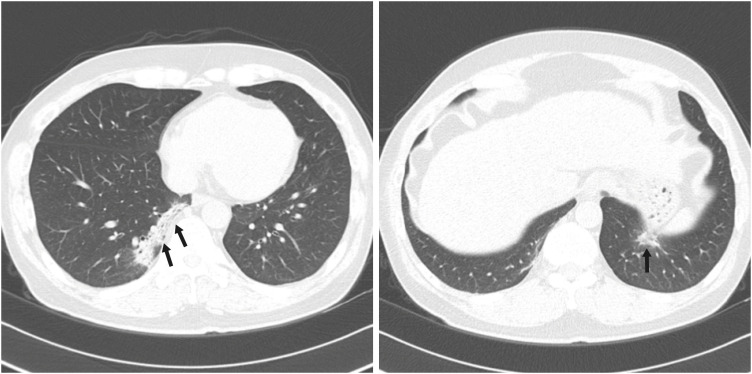
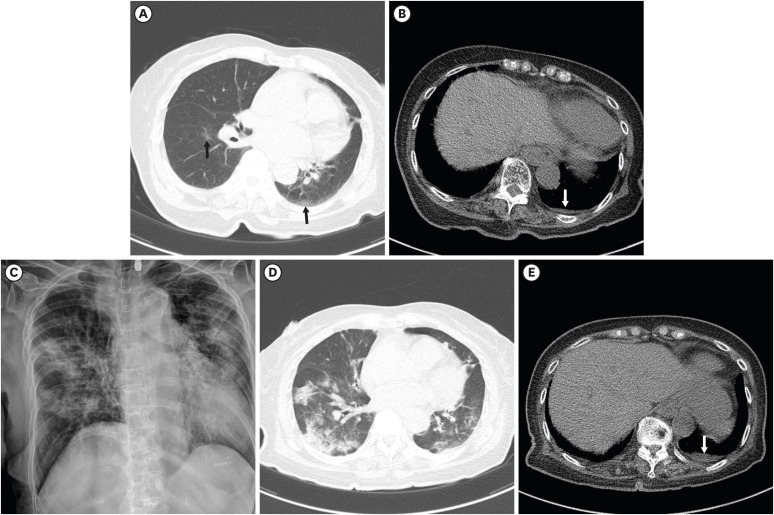
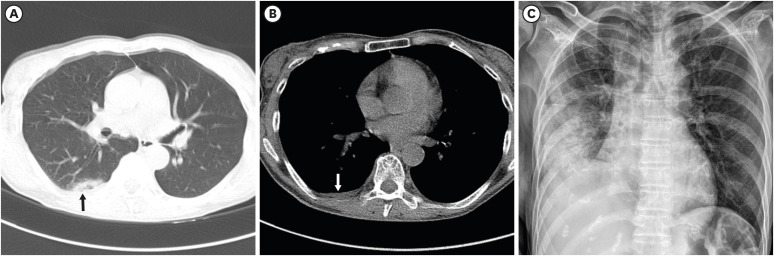
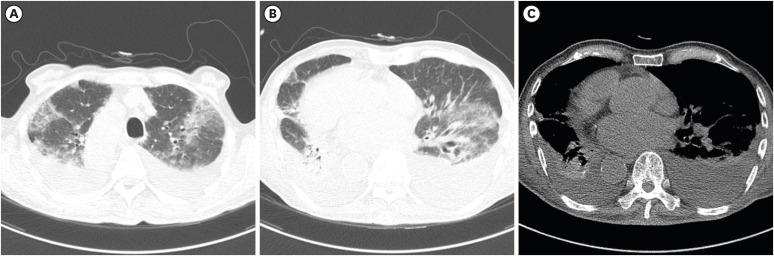
Among the 281 patients, 36 (12.8%) patients were in the severe group and 245 (87.2%) patients were in the non-severe group. Critical events occurred in 10 patients (3.6%). In the severe group, patients showed significantly more pneumonia with consolidation, crazy-paving appearance, pleural effusion, and higher CT scores than those in the non-severe group (all, p < 0.05). In the multivariate regression, pleural effusion (odds ratio [OR], 8.96; 95% confidence interval [CI], 1.81–44.42; p = 0.007), CT score > 5 (OR, 3.70; 95% CI, 1.44– 9.53; p = 0.007), old age (> 77 years, OR, 9.96; 95% CI, 3.78–26.28; p < 0.001), and elevated C-reactive protein (OR, 4.15; 95% CI, 1.62–10.6; p = 0.003) were significant prognostic factors of severe disease. CT score > 5 (OR, 7.29; 95% CI, 1.37–38.68; p = 0.020), pleural effusion (OR, 5.67; 95% CI, 1.04–30.8; p = 0.045) and old age (OR, 8.6; 95% CI, 1.80–41.0; p = 0.007) were also significant predictors of critical events.
Conclusion
Pleural effusion and the extent of pneumonia on initial CT scans are associated with poor prognosis in patients with COVID-19.
Keyword
Figure
Cited by 2 articles
-
Establishment of a Nationwide Korean Imaging Cohort of Coronavirus Disease 2019
Soon Ho Yoon, Soo-Youn Ham, Bo Da Nam, Kum Ju Chae, Dabee Lee, Jin Young Yoo, So Hyeon Bak, Jin Young Kim, Jin Hwan Kim, Ki Beom Kim, Jung Im Jung, Jae-Kwang Lim, Jong Eun Lee, Myung Jin Chung, Young Kyung Lee, Young Seon Kim, Ji Eun Jo, Sang Min Lee, Woocheol Kwon, Chang Min Park, Yun-Hyeon Kim, Yeon Joo Jeong
J Korean Med Sci. 2020;35(46):e413. doi: 10.3346/jkms.2020.35.e413.Prognostic Implications of CT Feature Analysis in Patients with COVID-19: a Nationwide Cohort Study
Yeon Joo Jeong, Bo Da Nam, Jin Young Yoo, Kun-Il Kim, Hee Kang, Jung Hwa Hwang, Yun-Hyeon Kim, Kyung Soo Lee
J Korean Med Sci. 2021;36(8):e51. doi: 10.3346/jkms.2021.36.e51.
Reference
-
1. World Health Organization. WHO Director-general's opening remarks at the media briefing on COVID-19. Updated 2020. Accessed April 13, 2020. https://www.who.int/docs/default-source/coronaviruse/clinical-management-of-novel-cov.pdf.2. Worldometer. COVID-19 coronavirus pandemic. Updated 2020. Accessed May 20, 2020. https://www.worldometers.info/coronavirus/.3. Chen T, Wu D, Chen H, Yan W, Yang D, Chen G, et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ. 2020; 368:m1091. PMID: 32217556.
Article4. Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020; 395(10229):1054–1062. PMID: 32171076.
Article5. Rubin GD, Ryerson CJ, Haramati LB, Sverzellati N, Kanne JP, Raoof S, et al. The role of chest imaging in patient management during the COVID-19 pandemic: a multinational consensus statement from the Fleischner Society. Chest. 2020; 158(1):106–116. PMID: 32275978.
Article6. Kim H, Hong H, Yoon SH. Diagnostic performance of CT and reverse transcriptase polymerase chain reaction for coronavirus disease 2019: a meta-analysis. Radiology. 2020; 296(3):E145–55. PMID: 32301646.7. Erturk SM. CT Is not a screening tool for coronavirus disease (COVID-19) pneumonia. AJR Am J Roentgenol. 2020; 215(1):W11. PMID: 32286875.
Article8. Tabatabaei SM, Talari H, Moghaddas F, Rajebi H. Computed tomographic features and short-term prognosis of coronavirus disease 2019 (COVID-19) pneumonia: a single-center study from Kashan, Iran. Radiol Cardiothorac Imaging. 2020; 2(2):e200130.9. Zhang R, Ouyang H, Fu L, Wang S, Han J, Huang K, et al. CT features of SARS-CoV-2 pneumonia according to clinical presentation: a retrospective analysis of 120 consecutive patients from Wuhan city. Eur Radiol. 2020; 30(8):4417–4426. PMID: 32279115.
Article10. Guan W, Liu J, Yu C. CT findings of coronavirus disease (COVID-19) severe pneumonia. AJR Am J Roentgenol. 2020; 214(5):W85–6. PMID: 32208010.
Article11. World Health Organization. Clinical management of severe acute respiratory infection (SARI) when COVID-19 disease is suspected: interim guidance. Updated 2020. Accessed April 13, 2020. https://www.who.int/docs/default-source/coronaviruse/clinical-management-of-novel-cov.pdf.12. Yoon SH, Lee KH, Kim JY, Lee YK, Ko H, Kim KH, et al. Chest radiographic and CT findings of the 2019 novel coronavirus disease (COVID-19): analysis of nine patients treated in Korea. Korean J Radiol. 2020; 21(4):494–500. PMID: 32100485.
Article13. Moy MP, Levsky JM, Berko NS, Godelman A, Jain VR, Haramati LB. A new, simple method for estimating pleural effusion size on CT scans. Chest. 2013; 143(4):1054–1059. PMID: 23632863.
Article14. Yang R, Li X, Liu H, Zhen Y, Zhang X, Xiong Q, et al. Chest CT severity score: an imaging tool for assessing severe COVID-19. Radiol Cardiothorac Imaging. 2020; 2(2):e200047.15. Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol. 1996; 49(12):1373–1379. PMID: 8970487.
Article16. Caruso D, Zerunian M, Polici M, Pucciarelli F, Polidori T, Rucci C, et al. Chest CT features of COVID-19 in Rome, Italy. Radiology. 2020; 296(2):E79–E85. PMID: 32243238.
Article17. Shi H, Han X, Jiang N, Cao Y, Alwalid O, Gu J, et al. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis. 2020; 20(4):425–434. PMID: 32105637.
Article18. Cheng Z, Lu Y, Cao Q, Qin L, Pan Z, Yan F, et al. Clinical features and chest CT manifestations of coronavirus disease 2019 (COVID-19) in a single-center study in Shanghai, China. AJR Am J Roentgenol. 2020; 215(1):121–126. PMID: 32174128.
Article19. Das KM, Lee EY, Al Jawder SE, Enani MA, Singh R, Skakni L, et al. Acute Middle East respiratory syndrome coronavirus: temporal lung changes observed on the chest radiographs of 55 patients. AJR Am J Roentgenol. 2015; 205(3):W267–W274. PMID: 26102309.
Article20. Das KM, Lee EY, Langer RD, Larsson SG. Middle East respiratory syndrome coronavirus: What does a radiologist need to know? AJR Am J Roentgenol. 2016; 206(6):1193–1201. PMID: 26998804.
Article21. Hsieh SC, Chan WP, Chien JC, Lee WS, Yao MS, Choi WM, et al. Radiographic appearance and clinical outcome correlates in 26 patients with severe acute respiratory syndrome. AJR Am J Roentgenol. 2004; 182(5):1119–1122. PMID: 15100105.
Article22. Hosseiny M, Kooraki S, Gholamrezanezhad A, Reddy S, Myers L. Radiology perspective of coronavirus disease 2019 (COVID-19): lessons from severe acute respiratory syndrome and Middle East respiratory syndrome. AJR Am J Roentgenol. 2020; 214(5):1078–1082. PMID: 32108495.
Article23. Falzarano D, de Wit E, Feldmann F, Rasmussen AL, Okumura A, Peng X, et al. Infection with MERS-CoV causes lethal pneumonia in the common marmoset. PLoS Pathog. 2014; 10(8):e1004250. PMID: 25144235.
Article24. Zou Z, Yang Y, Chen J, Xin S, Zhang W, Zhou X, et al. Prognostic factors for severe acute respiratory syndrome: a clinical analysis of 165 cases. Clin Infect Dis. 2004; 38(4):483–489. PMID: 14765339.
Article25. Colombi D, Bodini FC, Petrini M, Maffi G, Morelli N, Milanese G, et al. Well-aerated lung on admitting chest CT to predict adverse outcome in COVID-19 pneumonia. Radiology. 2020; 296(2):E86–96. PMID: 32301647.26. Wang Y, Dong C, Hu Y, Li C, Ren Q, Zhang X, et al. Temporal changes of CT findings in 90 patients with COVID-19 pneumonia: a longitudinal study. Radiology. 2020; 296(2):E55–64. PMID: 32191587.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pneumonia Associated with 2019 Novel Coronavirus: Can Computed Tomographic Findings Help Predict the Prognosis of the Disease?
- Bacterial meningitis in newborn and infant: Correlation between organism, CT findings and clinical outcome
- Clinical Features of Mild Head Injury in the Elderly
- Prediction of Adverse Outcomes among Women in the Third Trimester of Pregnancy with Coronavirus Disease 2019
- Traumatic Intraventricular Hemorrhage: Classifications and Prognosis According to CT Findings