Ann Rehabil Med.
2020 Aug;44(4):311-319. 10.5535/arm.19181.
A Fully Immersive Virtual Reality Method for Upper Limb Rehabilitation in Spinal Cord Injury
- Affiliations
-
- 1Department of Rehabilitation Medicine, Chungnam National University College of Medicine, Daejeon, Korea
- 2Biomedical Institute, Chungnam National University, Daejeon, Korea
- KMID: 2505391
- DOI: http://doi.org/10.5535/arm.19181
Abstract
Objective
To determine whether a fully immersive virtual reality (VR) intervention combined with conventional rehabilitation (CR) can improve upper limb function more than CR alone in patients with spinal cord injury (SCI), we conducted a prospective, randomized, controlled clinical trial.
Methods
Participants were randomly assigned to either the control group (CG; n=10) or experimental group (EG; n=10). The participants in the CG received 60 minutes of conventional therapy per day, 4 days per week for 4 weeks, whereas those in the EG received 30 minutes of VR training and 30 minutes of conventional therapy per day, 4 days per week for 4 weeks. The clinical outcome measures included Medical Research Council grade, the American Spinal Injury Association upper extremity motor score (ASIA-UEMS), and scores in the Hand Strength Test, Box and Block Test, Nine-Hole Peg Test, Action Research Arm Test, and Korean version of the Spinal Cord Independence Measure (K-SCIM). The assessments were performed at the beginning (T0) and end of the intervention (T1).
Results
Grip power and K-SCIM score significantly improved in the EG after the intervention. When comparing differences between the groups, elbow extensor, wrist extensor, ASIA-UEMS, grip power, lateral pinch power, and palmar pinch power were all significantly improved.
Conclusion
VR training of upper limb function after SCI can provide an acceptable adjunctive rehabilitation method without significant adverse effects.
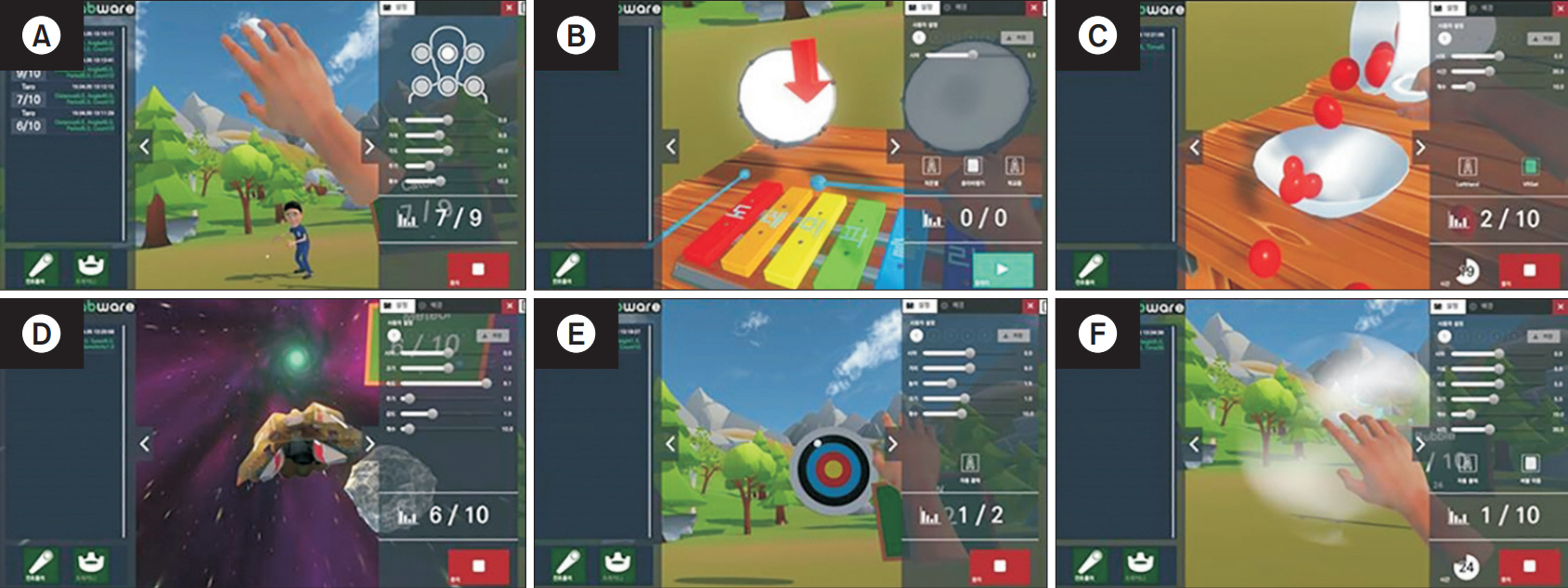
Figure
Reference
-
1. Almeida VM, Paiva AE, Sena IF, Mintz A, Magno LA, Birbrair A. Pericytes make spinal cord breathless after injury. Neuroscientist. 2018; 24:440–7.
Article2. Wyndaele M, Wyndaele JJ. Incidence, prevalence and epidemiology of spinal cord injury: what learns a worldwide literature survey? Spinal Cord. 2006; 44:523–9.
Article3. Jain NB, Ayers GD, Peterson EN, Harris MB, Morse L, O’Connor KC, et al. Traumatic spinal cord injury in the United States, 1993-2012. JAMA. 2015; 313:2236–43.
Article4. Snoek GJ, IJzerman MJ, Hermens HJ, Maxwell D, Biering-Sorensen F. Survey of the needs of patients with spinal cord injury: impact and priority for improvement in hand function in tetraplegics. Spinal Cord. 2004; 42:526–32.
Article5. Anderson KD. Targeting recovery: priorities of the spinal cord-injured population. J Neurotrauma. 2004; 21:1371–83.
Article6. Saposnik G, Cohen LG, Mamdani M, Pooyania S, Ploughman M, Cheung D, et al. Efficacy and safety of non-immersive virtual reality exercising in stroke rehabilitation (EVREST): a randomised, multicentre, single-blind, controlled trial. Lancet Neurol. 2016; 15:1019–27.
Article7. Kwon JS, Park MJ, Yoon IJ, Park SH. Effects of virtual reality on upper extremity function and activities of daily living performance in acute stroke: a double-blind randomized clinical trial. NeuroRehabilitation. 2012; 31:379–85.
Article8. Lohse KR, Hilderman CG, Cheung KL, Tatla S, Van der Loos HF. Virtual reality therapy for adults post-stroke: a systematic review and meta-analysis exploring virtual environments and commercial games in therapy. PLoS One. 2014; 9:e93318.
Article9. Sin H, Lee G. Additional virtual reality training using Xbox Kinect in stroke survivors with hemiplegia. Am J Phys Med Rehabil. 2013; 92:871–80.
Article10. Saposnik G, Levin M; Outcome Research Canada (SORCan) Working Group. Virtual reality in stroke rehabilitation: a meta-analysis and implications for clinicians. Stroke. 2011; 42:1380–6.11. Corbetta D, Imeri F, Gatti R. Rehabilitation that incorporates virtual reality is more effective than standard rehabilitation for improving walking speed, balance and mobility after stroke: a systematic review. J Physiother. 2015; 61:117–24.
Article12. AMP New Ventures. Virtual reality (VR) continuum [Internet]. Sydney, Australia: AMP New Ventures;2016. [cited 2020 Jul 14]. Available from: https://www.slideshare.net/ampnewventures/virtual-reality-vr-continuum-amp-new-ventures.13. Moreira MC, de Amorim Lima AM, Ferraz KM, Benedetti Rodrigues MA. Use of virtual reality in gait recovery among post stroke patients: a systematic literature review. Disabil Rehabil Assist Technol. 2013; 8:357–62.14. Dimbwadyo-Terrer I, Gil-Agudo A, Segura-Fragoso A, de los Reyes-Guzman A, Trincado-Alonso F, Piazza S, et al. Effectiveness of the virtual reality system Toyra on upper limb function in people with tetraplegia: a pilot randomized clinical trial. Biomed Res Int. 2016; 2016:6397828.
Article15. Prasad S, Aikat R, Labani S, Khanna N. Efficacy of virtual reality in upper limb rehabilitation in patients with spinal cord injury: a pilot randomized controlled trial. Asian Spine J. 2018; 12:927–34.
Article16. Poynton AR, O’Farrell DA, Shannon F, Murray P, McManus F, Walsh MG. An evaluation of the factors affecting neurological recovery following spinal cord injury. Injury. 1997; 28:545–8.
Article17. Waters RL, Adkins RH, Yakura JS, Sie I. Motor and sensory recovery following complete tetraplegia. Arch Phys Med Rehabil. 1993; 74:242–7.18. Waters RL, Adkins RH, Yakura JS, Sie I. Motor and sensory recovery following incomplete tetraplegia. Arch Phys Med Rehabil. 1994; 75:306–11.
Article19. Sumida M, Fujimoto M, Tokuhiro A, Tominaga T, Magara A, Uchida R. Early rehabilitation effect for traumatic spinal cord injury. Arch Phys Med Rehabil. 2001; 82:391–5.
Article20. Laver KE, Lange B, George S, Deutsch JE, Saposnik G, Crotty M. Virtual reality for stroke rehabilitation. Cochrane Database Syst Rev. 2017; 11:CD008349.
Article21. Lee HS, Park YJ, Park SW. The effects of virtual reality training on function in chronic stroke patients: a systematic review and meta-analysis. Biomed Res Int. 2019; 2019:7595639.
Article22. Faria AL, Andrade A, Soares L, I Badia SB. Benefits of virtual reality based cognitive rehabilitation through simulated activities of daily living: a randomized controlled trial with stroke patients. J Neuroeng Rehabil. 2016; 13:96.
Article23. Brunner I, Skouen JS, Hofstad H, Abmuss J, Becker F, Pallesen H, et al. Is upper limb virtual reality training more intensive than conventional training for patients in the subacute phase after stroke? An analysis of treatment intensity and content. BMC Neurol. 2016; 16:219.
Article24. Oh YB, Kim GW, Han KS, Won YH, Park SH, Seo JH, et al. Efficacy of virtual reality combined with real instrument training for patients with stroke: a randomized controlled trial. Arch Phys Med Rehabil. 2019; 100:1400–8.
Article25. Harvey LA, Dunlop SA, Churilov L, Hsueh YS, Galea MP. Early intensive hand rehabilitation after spinal cord injury (“Hands On”): a protocol for a randomised controlled trial. Trials. 2011; 12:14.
Article26. Devivo MJ. Epidemiology of traumatic spinal cord injury: trends and future implications. Spinal Cord. 2012; 50:365–72.
Article27. Bracken MB, Shepard MJ, Holford TR, Leo-Summers L, Aldrich EF, Fazl M, et al. Administration of methylprednisolone for 24 or 48 hours or tirilazad mesylate for 48 hours in the treatment of acute spinal cord injury. Results of the Third National Acute Spinal Cord Injury Randomized Controlled Trial. JAMA. 1997; 277:1597–604.28. Bracken MB, Holford TR. Effects of timing of methylprednisolone or naloxone administration on recovery of segmental and long-tract neurological function in NASCIS 2. J Neurosurg. 1993; 79:500–7.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Motor Learning by Novel Therapeutic Approaches: Virtual Reality and Robotics
- Efficacy of Virtual Reality in Upper Limb Rehabilitation in Patients with Spinal Cord Injury: A Pilot Randomized Controlled Trial
- Efficacy of Electrical Stimulation-Augmented Virtual Reality Training in Improving Balance in Individuals with Incomplete Spinal Cord Injury: Study Protocol of a Randomized Controlled Trial
- Spinal Cord Injury Rehabilitation (II): Management of Neurogenic Bladder
- Role of Virtual Reality in Balance Training in Patients with Spinal Cord Injury: A Prospective Comparative Pre-Post Study