Ann Hepatobiliary Pancreat Surg.
2020 Aug;24(3):333-338. 10.14701/ahbps.2020.24.3.333.
Management of hepatic artery aneurysm: A case series
- Affiliations
-
- 1Departments of Surgery, Virginia Commonwealth University Health System, Richmond, VA, USA
- 2Departments of Radiology, Virginia Commonwealth University Health System, Richmond, VA, USA
- KMID: 2505347
- DOI: http://doi.org/10.14701/ahbps.2020.24.3.333
Abstract
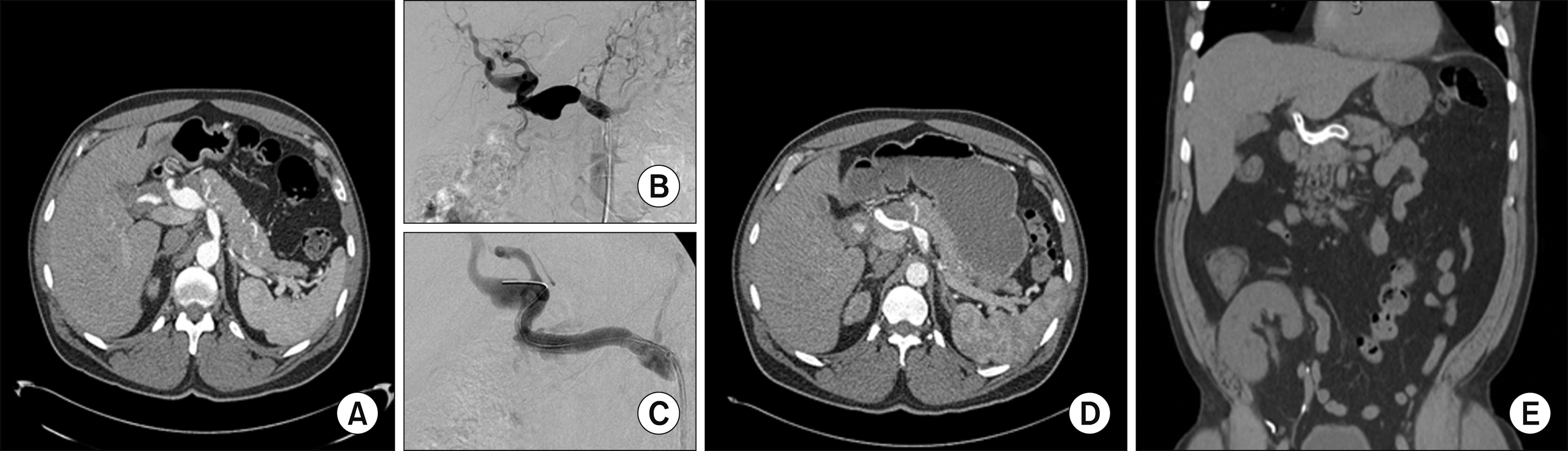
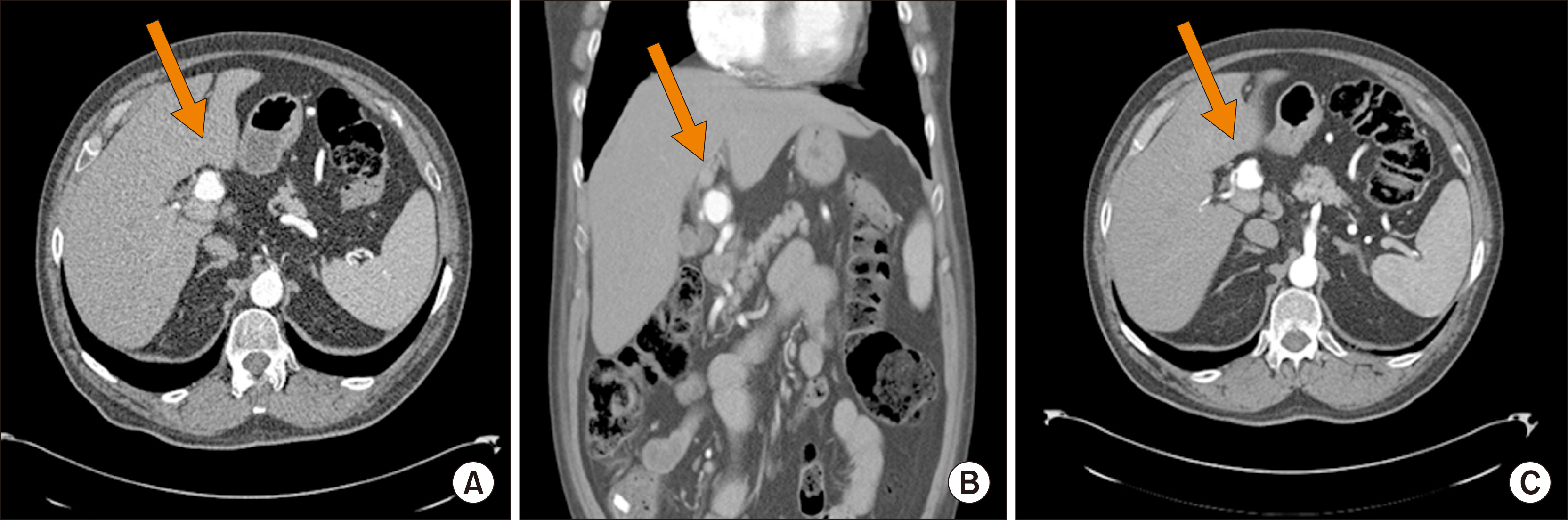
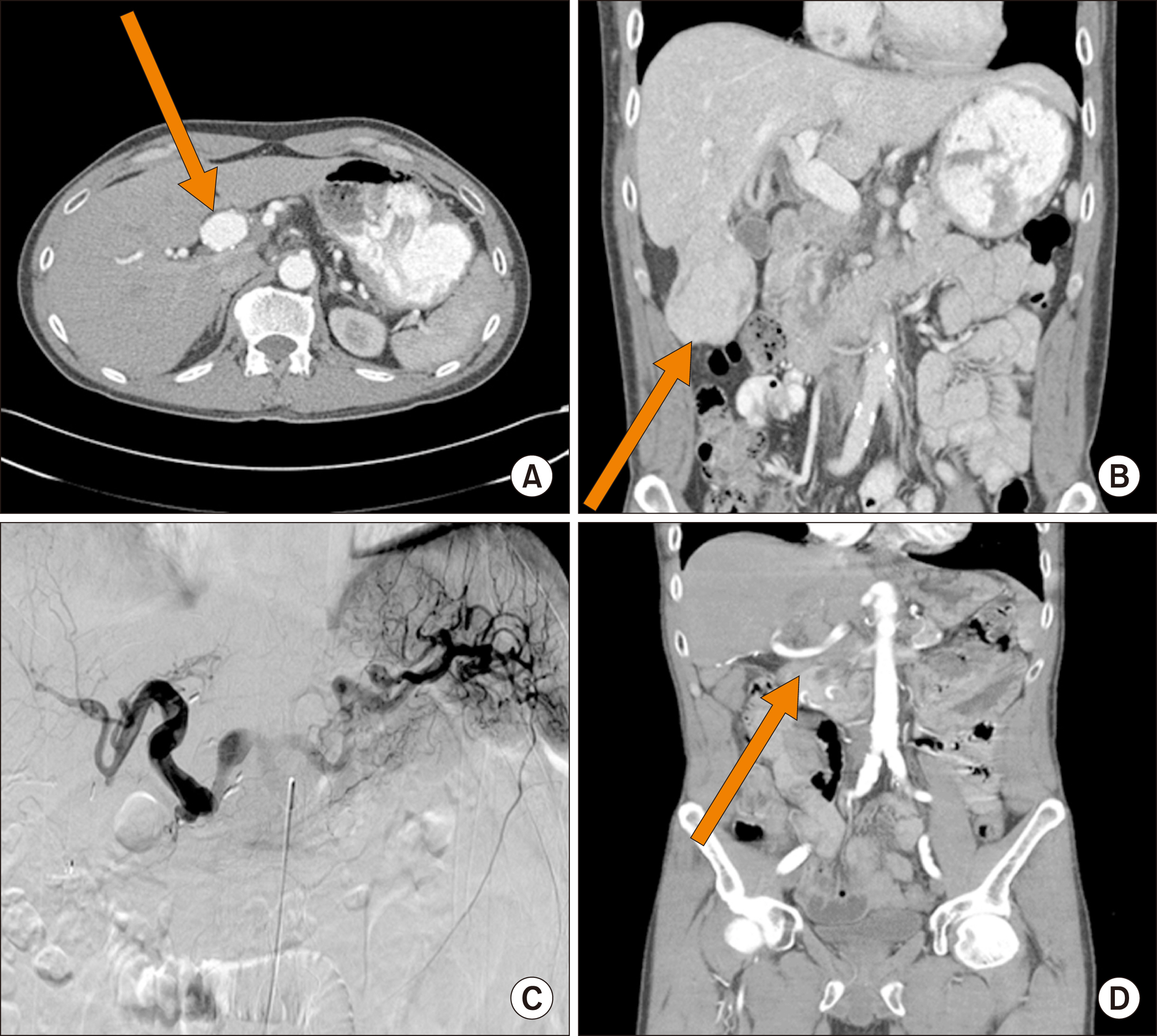
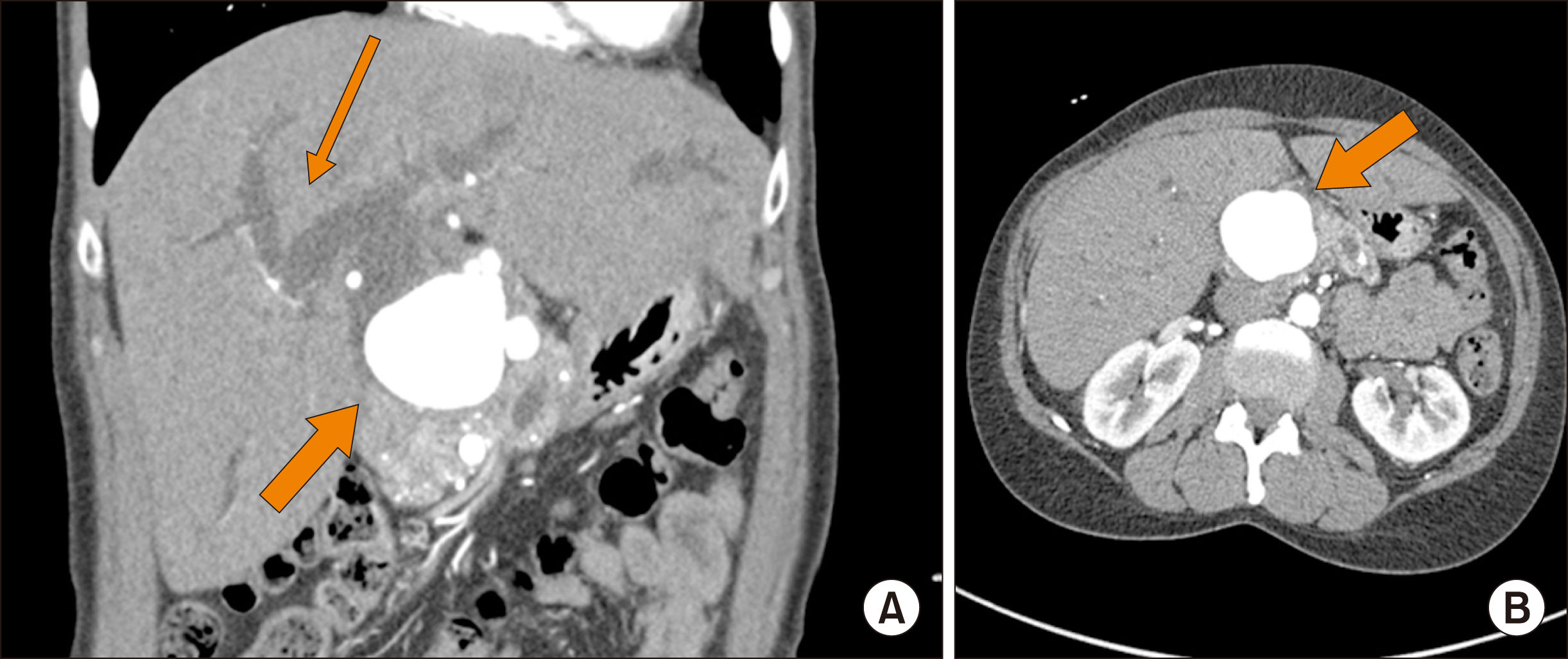
- Hepatic artery aneurysms are rare, but their diagnosis is important because of high mortality and complications.Common risk factors for developing these aneurysms include hypertension, vascular disease, pancreatitis, diabetes, tobacco use, autoimmune diseases, and previous transplantation. Frequent imaging for trauma and tumor surveillance has increased the incidence of naive hepatic aneurysms. These aneurysms can be difficult to manage, and it can be challenging to decide the correct treatment modality for the patient. Hereby, we present four cases of hepatic artery aneurysm and discuss various treatment options. Patient 1 suffered from a proper and right hepatic artery aneurysm discovered incidentally; repaired with an endovascular intervention later complicated by an endoleak which was further managed by another stenting. Patient 2 had a common hepatic artery aneurysm followed with serial imaging without any intervention. Patient 3 had a hepatic artery aneurysm and liver mass diagnosed concurrently. The patient underwent an open surgical repair of his aneurysm with graft and liver resection which was complicated later with rupture of aneurysm followed by surgical bypass repair. Patient 4 suffered from a large hepatic artery aneurysm causing bile duct compression. Her aneurysm was repaired open with splenic artery grafting. Patients were managed from careful observation to surgery with different outcomes.
Figure
Cited by 1 articles
-
Hepatic artery aneurysms: Endovascular therapeutic techniques
Umberto Geremia Rossi, Francesco Petrocelli
Ann Hepatobiliary Pancreat Surg. 2021;25(2):167-170. doi: 10.14701/ahbps.2021.25.2.167.
Reference
-
1. Chadha M, Ahuja C. 2009; Visceral artery aneurysms: diagnosis and percutaneous management. Semin Intervent Radiol. 26:196–206. DOI: 10.1055/s-0029-1225670. PMID: 21326564. PMCID: PMC3036493.
Article2. Bacalbasa N, Brezean I, Anghel C, Barbu I, Pautov M, Balescu I, et al. 2017; Successful resection and vascular ligation of a large hepatic artery aneurysm-a case report and literature review. In Vivo. 31:979–982. PMID: 28882969. PMCID: PMC5656876.3. Røkke O, Søndenaa K, Amundsen S, Bjerke-Larssen T, Jensen D. 1996; The diagnosis and management of splanchnic artery aneurysms. Scand J Gastroenterol. 31:737–743. DOI: 10.3109/00365529609010344. PMID: 8858739.
Article4. Madhusudhan KS, Venkatesh HA, Gamanagatti S, Garg P, Srivastava DN. 2016; Interventional radiology in the management of visceral artery pseudoaneurysms: a review of techniques and embolic materials. Korean J Radiol. 17:351–363. DOI: 10.3348/kjr.2016.17.3.351. PMID: 27134524. PMCID: PMC4842855.
Article5. Dolapci M, Ersoz S, Kama NA. 2003; Hepatic artery aneurysm. Ann Vasc Surg. 17:214–216. DOI: 10.1007/s10016-001-0296-0. PMID: 12616357.
Article6. Berceli SA. 2005; Hepatic and splenic artery aneurysms. Semin Vasc Surg. 18:196–201. DOI: 10.1053/j.semvascsurg.2005.09.005. PMID: 16360576.
Article7. Rapp JH, et al. 2010. Chapter 34: Arteries. CURRENT Diagnosis & Treatment: Surgery, 13e. McGraw-Hill;New York, NY: Doherty GM. eds.8. Abbas MA, Fowl RJ, Stone WM, Panneton JM, Oldenburg WA, Bower TC, et al. 2003; Hepatic artery aneurysm: factors that predict complications. J Vasc Surg. 38:41–45. DOI: 10.1016/S0741-5214(03)00090-9. PMID: 12844087.
Article9. Lu M, Weiss C, Fishman EK, Johnson PT, Verde F. 2015; Review of visceral aneurysms and pseudoaneurysms. J Comput Assist Tomogr. 39:1–6. DOI: 10.1097/RCT.0000000000000156. PMID: 25319606.
Article10. Ricotta JJ, Akbari CM. Zinner MJ, Ashley SW, editors. 2013. Abdominal vascular emergencies. Maingot's abdominal operations. 12th ed. McGraw Hill Professional;New York: p. 000–000.11. O'Driscoll D, Olliff SP, Olliff JF. 1999; Hepatic artery aneurysm. Br J Radiol. 72:1018–1025. DOI: 10.1259/bjr.72.862.10673957. PMID: 10673957.12. Jana M, Gamanagatti S, Mukund A, Paul S, Gupta P, Garg P, et al. 2011; Endovascular management in abdominal visceral arterial aneurysms: a pictorial essay. World J Radiol. 3:182–187. DOI: 10.4329/wjr.v3.i7.182. PMID: 21860714. PMCID: PMC3158896.
Article13. Yu YH, Sohn JH, Kim TY, Jeong JY, Han DS, Jeon YC, et al. 2012; Hepatic artery pseudoaneurysm caused by acute idiopathic pancreatitis. World J Gastroenterol. 18:2291–2294. DOI: 10.3748/wjg.v18.i18.2291. PMID: 22611325. PMCID: PMC3351782.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Right Gastroepiploic Artery Transposition for a Common Hepatic Artery and Proper Hepatic Artery Aneurysm Repair
- A Dissecting Aneurysm of the Common and Proper Hepatic Artery with Dissection of the Celiac Axis and the SMA
- Celiomesenteric Trunk with Concurrent Common Hepatic Artery Aneurysm: A Case Report
- A case of aneurysm of the proper hepatic artery as a rare cause of upper gastrointestinal bleeding
- Hepatic Artery Pseudoaneurysm Associated with Plastic Biliary Stent