Clin Exp Otorhinolaryngol.
2020 Aug;13(3):225-233. 10.21053/ceo.2020.00360.
Maxillomandibular Advancement and Upper Airway Stimulation: Extrapharyngeal Surgery for Obstructive Sleep Apnea
- Affiliations
-
- 1Division of Sleep Surgery, Department of Otolaryngology-Head and Neck Surgery, Stanford Hospital and Clinics, Stanford, CA, USA
- 2Department of Otorhinolaryngology-Head and Neck Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2504916
- DOI: http://doi.org/10.21053/ceo.2020.00360
Abstract
- There are many ways to categorize surgery for obstructive sleep apnea (OSA), one of which is to distinguish between intrapharyngeal and extrapharyngeal procedures. While the general otolaryngologist treating OSA is familiar with intrapharyngeal procedures, such as uvulopalatopharyngoplasty and tongue base reduction, extrapharyngeal sleep operations such as maxillomandibular advancement (MMA) and upper airway stimulation (UAS) have evolved rapidly in the recent decade and deserve a dedicated review. MMA and UAS have both shown predictable high success rates with low morbidity. Each approach has unique strengths and limitations, and for the most complex of OSA patients, the two in combination complement each other. Extrapharyngeal airway operations are critical for achieving favorable outcomes for sleep surgeons.
Keyword
Figure
Cited by 1 articles
-
Effect of Obstructive Sleep Apnea on Immunity in Cases of Chronic Rhinosinusitis With Nasal Polyps
Dong-Kyu Kim, Byeong Chan Lee, Ki Joon Park, Gil Myeong Son
Clin Exp Otorhinolaryngol. 2021;14(4):390-398. doi: 10.21053/ceo.2020.02250.
Reference
-
1. Benjafield A, Valentine K, Ayas N, Eastwood PR, Heinzer RC, Ip MS. Global prevalence of obstructive sleep apnea in adults: estimation using currently available data [abstract]. In : American Thoracic Society 2018 International Conference; 2018; San Diego, CA, USA. San Diego, CA: American Thoracic Society;2018. p. A3962.
Article2. Soose RJ, Gillespie MB. Upper airway stimulation therapy: a novel approach to managing obstructive sleep apnea. Laryngoscope. 2016; Sep. 126 Suppl 7:S5–8.
Article3. Lam B, Lam DC, Ip MS. Obstructive sleep apnoea in Asia. Int J Tuberc Lung Dis. 2007; Jan. 11(1):2–11.4. Salman LA, Shulman R, Cohen JB. Obstructive sleep apnea, hypertension, and cardiovascular risk: epidemiology, pathophysiology, and management. Curr Cardiol Rep. 2020; Jan. 22(2):6.
Article5. Young T, Palta M, Dempsey J, Peppard PE, Nieto FJ, Hla KM. Burden of sleep apnea: rationale, design, and major findings of the Wisconsin Sleep Cohort study. WMJ. 2009; Aug. 108(5):246–9.6. Garrigue S, Pepin JL, Defaye P, Murgatroyd F, Poezevara Y, Clementy J, et al. High prevalence of sleep apnea syndrome in patients with long-term pacing: the European Multicenter Polysomnographic Study. Circulation. 2007; Apr. 115(13):1703–9.7. Kim JH, Kwon MS, Song HM, Lee BJ, Jang YJ, Chung YS. Compliance with positive airway pressure treatment for obstructive sleep apnea. Clin Exp Otorhinolaryngol. 2009; Jun. 2(2):90–6.
Article8. Powell NB. Contemporary surgery for obstructive sleep apnea syndrome. Clin Exp Otorhinolaryngol. 2009; Sep. 2(3):107–14.
Article9. Li KK, Powell NB, Riley RW, Troell RJ, Guilleminault C. Long-term results of maxillomandibular advancement surgery. Sleep Breath. 2000; 4(3):137–40.
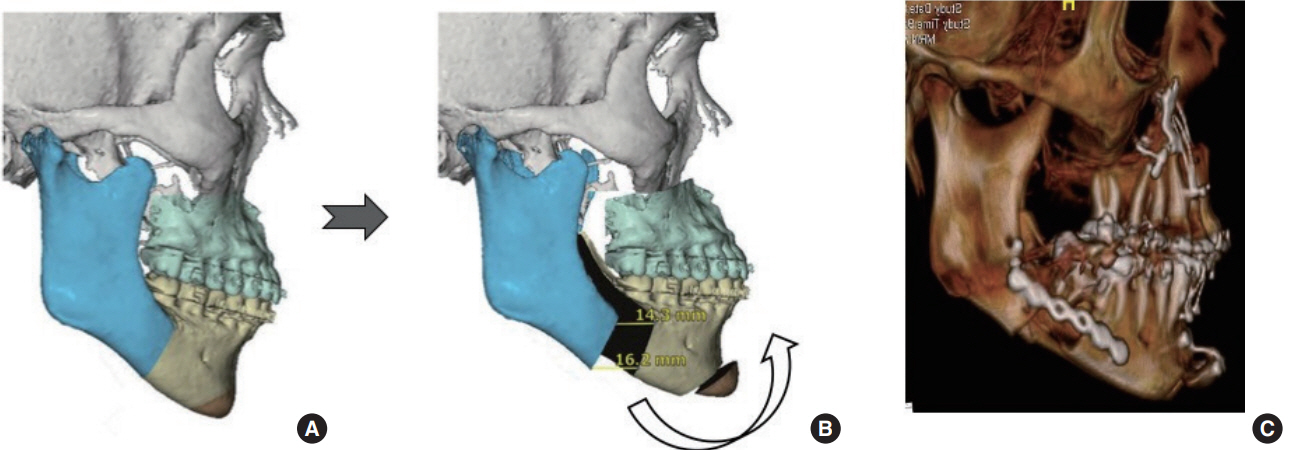
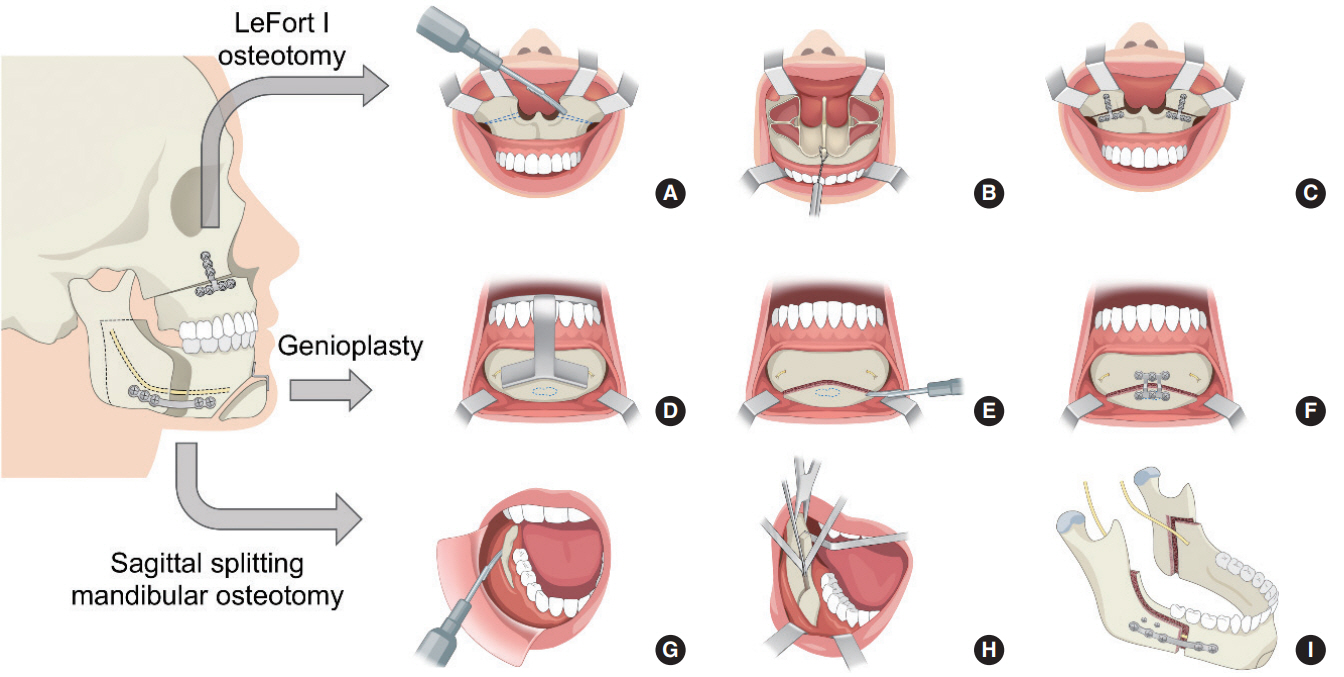
Article10. Camacho M, Liu SY, Certal V, Capasso R, Powell NB, Riley RW. Large maxillomandibular advancements for obstructive sleep apnea: an operative technique evolved over 30 years. J Craniomaxillofac Surg. 2015; Sep. 43(7):1113–8.11. Liu SY, Awad M, Riley R, Capasso R. The role of the revised Stanford protocol in today’s precision medicine. Sleep Med Clin. 2019; Mar. 14(1):99–107.
Article12. Awad M, Okland TS, Nekhendzy V. Drug-induced sleep endoscopy. Atlas Oral Maxillofac Surg Clin North Am. 2019; Mar. 27(1):7–10.
Article13. Kastoer C, Op de Beeck S, Dom M, Neirinckx T, Verbraecken J, Braem MJ, et al. Drug-induced sleep endoscopy upper airway collapse patterns and maxillomandibular advancement. Laryngoscope. 2020; Apr. 130(4):E268–74.
Article14. Liu SY, Huon LK, Iwasaki T, Yoon A, Riley R, Powell N, et al. Efficacy of maxillomandibular advancement examined with drug-induced sleep endoscopy and computational fluid dynamics airflow modeling. Otolaryngol Head Neck Surg. 2016; Jan. 154(1):189–95.
Article15. Liu SY, Huon LK, Powell NB, Riley R, Cho HG, Torre C, et al. Lateral pharyngeal wall tension after maxillomandibular advancement for obstructive sleep apnea is a marker for surgical success: observations from drug-induced sleep endoscopy. J Oral Maxillofac Surg. 2015; Aug. 73(8):1575–82.
Article16. Green KK, Kent DT, D’Agostino MA, Hoff PT, Lin HS, Soose RJ, et al. Drug-induced sleep endoscopy and surgical outcomes: a multicenter cohort study. Laryngoscope. 2019; Mar. 129(3):761–70.
Article17. Soares D, Sinawe H, Folbe AJ, Yoo G, Badr S, Rowley JA, et al. Lateral oropharyngeal wall and supraglottic airway collapse associated with failure in sleep apnea surgery. Laryngoscope. 2012; Feb. 122(2):473–9.
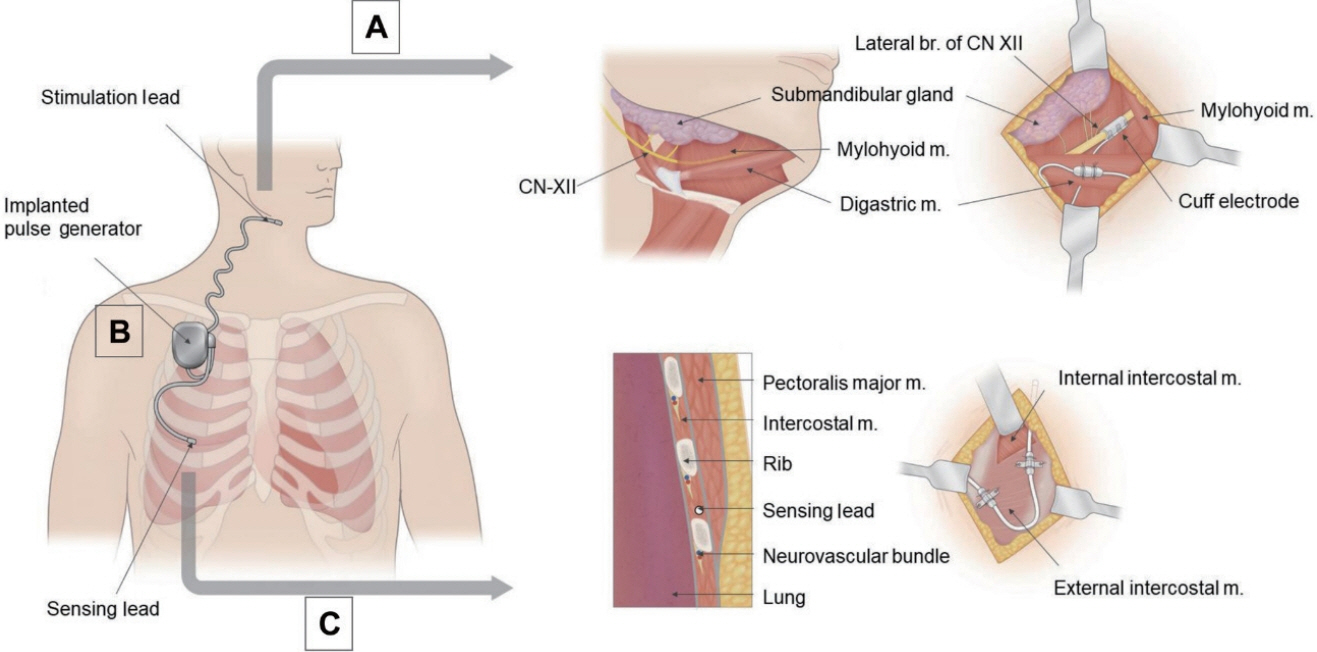
Article18. Vanderveken OM, Beyers J, Op de Beeck S, Dieltjens M, Willemen M, Verbraecken JA, et al. Development of a clinical pathway and technical aspects of upper airway stimulation therapy for obstructive sleep apnea. Front Neurosci. 2017; Sep. 11:523.
Article19. Liu SY, Wayne Riley R, Pogrel A, Guilleminault C. Sleep surgery in the era of precision medicine. Atlas Oral Maxillofac Surg Clin North Am. 2019; Mar. 27(1):1–5.
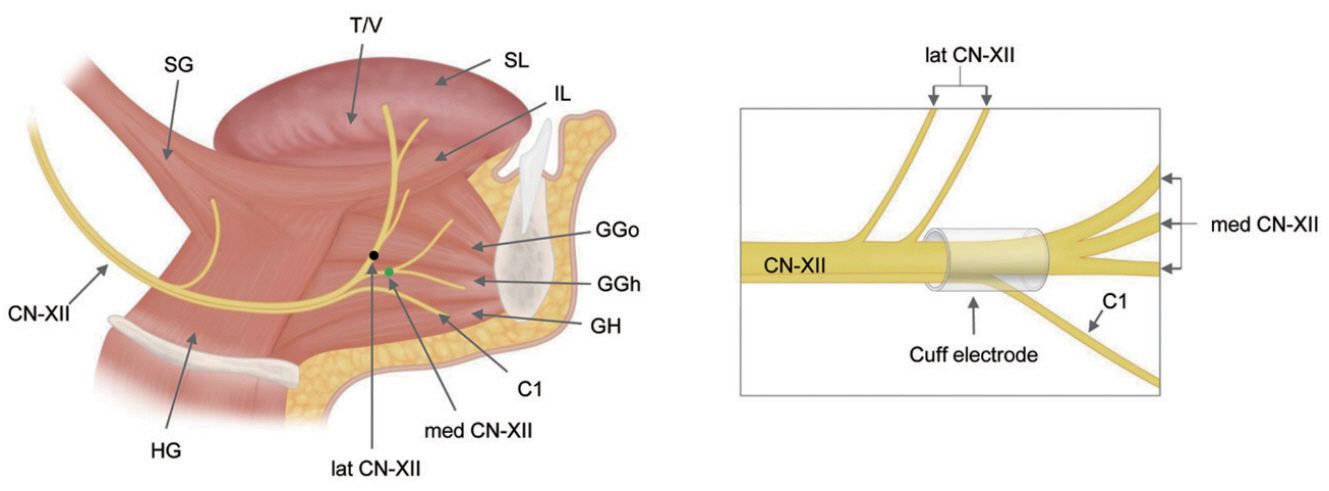
Article20. Liu SY, Awad M, Riley RW. Maxillomandibular advancement: contemporary approach at Stanford. Atlas Oral Maxillofac Surg Clin North Am. 2019; Mar. 27(1):29–36.21. Liu SY, Powell NB, Riley RW. Algorithm for multilevel treatment: the Riley, Powell, and Liu Stanford experience. In : Friedman M, Jacobowitz O, editors. Sleep and apnea snoring. Amsterdam: Elsevier;2020. p. 104–9.22. Gupta RJ, Kademani D, Liu SY. Upper airway (hypoglossal nerve) stimulation for treatment of obstructive sleep apnea. Atlas Oral Maxillofac Surg Clin North Am. 2019; Mar. 27(1):53–8.
Article23. Hasselbacher K, Seitz A, Abrams N, Wollenberg B, Steffen A. Complete concentric collapse at the soft palate in sleep endoscopy: what change is possible after UPPP in patients with CPAP failure? Sleep Breath. 2018; Dec. 22(4):933–8.
Article24. Steffen A. What makes the responder to upper airway stimulation in obstructive sleep apnea patients with positive airway pressure failure? J Thorac Dis. 2018; Sep. 10(Suppl 26):S3131–S4.
Article25. Liu SY, Hutz MJ, Poomkonsarn S, Chang CP, Awad M, Capasso R. Palatopharyngoplasty resolves concentric collapse in patients ineligible for upper airway stimulation. Laryngoscope. 2020; Feb. 28. [Epub]. https://doi.org/10.1002/lary.28595.
Article26. Boyd SB. Management of obstructive sleep apnea by maxillomandibular advancement. Oral Maxillofac Surg Clin North Am. 2009; 21(4):447–57.
Article27. Garg RK, Afifi AM, Sanchez R, King TW. Obstructive sleep apnea in adults: the role of upper airway and facial skeletal surgery. Plast Reconstr Surg. 2016; Oct. 138(4):889–98.28. Barrera JE. Skeletal surgery for obstructive sleep apnea. Otolaryngol Clin North Am. 2016; Dec. 49(6):1433–47.
Article29. Zaghi S, Holty JE, Certal V, Abdullatif J, Guilleminault C, Powell NB, et al. Maxillomandibular advancement for treatment of obstructive sleep apnea: a meta-analysis. JAMA Otolaryngol Head Neck Surg. 2016; Jan. 142(1):58–66.30. Prinsell JR. Maxillomandibular advancement surgery in a site-specific treatment approach for obstructive sleep apnea in 50 consecutive patients. Chest. 1999; Dec. 116(6):1519–29.
Article31. Riley RW, Powell NB, Guilleminault C. Maxillary, mandibular, and hyoid advancement for treatment of obstructive sleep apnea: a review of 40 patients. J Oral Maxillofac Surg. 1990; Jan. 48(1):20–6.
Article32. Dahy K, Takahashi K, Saito K, Kiso H, Rezk I, Oga T, et al. Gender differences in morphological and functional outcomes after mandibular setback surgery. J Craniomaxillofac Surg. 2018; Jun. 46(6):887–92.
Article33. Shah DH, Kim KB, McQuilling MW, Movahed R, Shah AH, Kim YI. Computational fluid dynamics for the assessment of upper airway changes in skeletal Class III patients treated with mandibular setback surgery. Angle Orthod. 2016; Nov. 86(6):976–82.
Article34. Tan SK, Leung WK, Tang AT, Zwahlen RA. Effects of mandibular setback with or without maxillary advancement osteotomies on pharyngeal airways: an overview of systematic reviews. PLoS One. 2017; Oct. 12(10):e0185951.
Article35. Yang HJ, Jung YE, Kwon IJ, Lee JY, Hwang SJ. Airway changes and prevalence of obstructive sleep apnoea after bimaxillary orthognathic surgery with large mandibular setback. Int J Oral Maxillofac Surg. 2020; Mar. 49(3):342–9.
Article36. Liu SY, Lee PJ, Awad M, Riley RW, Zaghi S. Corrective nasal surgery after maxillomandibular advancement for obstructive sleep apnea: experience from 379 cases. Otolaryngol Head Neck Surg. 2017; Jul. 157(1):156–9.
Article37. Chen YF, Ko EC, Zaghi S, Yoon A, Williams R, Riley R, et al. Optimizing mandibular sagittal split of large maxillomandibular advancements for obstructive sleep apnea: patient and surgical factors. Clin Oral Investig. 2020; Mar. 24(3):1359–67.
Article38. Liu SY, Huon LK, Zaghi S, Riley R, Torre C. An accurate method of designing and performing individual-specific genioglossus advancement. Otolaryngol Head Neck Surg. 2017; 156(1):194–7.
Article39. Holty JE, Guilleminault C. Maxillomandibular advancement for the treatment of obstructive sleep apnea: a systematic review and meta-analysis. Sleep Med Rev. 2010; Oct. 14(5):287–97.
Article40. John CR, Gandhi S, Sakharia AR, James TT. Maxillomandibular advancement is a successful treatment for obstructive sleep apnoea: a systematic review and meta-analysis. Int J Oral Maxillofac Surg. 2018; Dec. 47(12):1561–71.
Article41. Liu SY, Huon LK, Ruoff C, Riley RW, Strohl KP, Peng Z. Restoration of sleep architecture after maxillomandibular advancement: success beyond the apnea-hypopnea index. Int J Oral Maxillofac Surg. 2017; Dec. 46(12):1533–8.
Article42. Riley RW, Powell NB, Li KK, Troell RJ, Guilleminault C. Surgery and obstructive sleep apnea: long-term clinical outcomes. Otolaryngol Head Neck Surg. 2000; Mar. 122(3):415–21.
Article43. Vigneron A, Tamisier R, Orset E, Pepin JL, Bettega G. Maxillomandibular advancement for obstructive sleep apnea syndrome treatment: long-term results. J Craniomaxillofac Surg. 2017; Feb. 45(2):183–91.
Article44. Mahmoud AF, Thaler ER. Outcomes of hypoglossal nerve upper airway stimulation among patients with isolated retropalatal collapse. Otolaryngol Head Neck Surg. 2019; Jun. 160(6):1124–9.
Article45. Safiruddin F, Vanderveken OM, de Vries N, Maurer JT, Lee K, Ni Q, et al. Effect of upper-airway stimulation for obstructive sleep apnoea on airway dimensions. Eur Respir J. 2015; Jan. 45(1):129–38.
Article46. Doghramji K, Boon M. The role of upper airway stimulation therapy in the multidisciplinary management approach of obstructive sleep apnea in the adult patient. Laryngoscope. 2016; Sep. 126 Suppl 7:S9–11.
Article47. Oliven A, Odeh M, Geitini L, Oliven R, Steinfeld U, Schwartz AR, et al. Effect of coactivation of tongue protrusor and retractor muscles on pharyngeal lumen and airflow in sleep apnea patients. J Appl Physiol (1985). 2007; Nov. 103(5):1662–8.
Article48. Dedhia RC, Strollo PJ, Soose RJ. Upper airway stimulation for obstructive sleep apnea: past, present, and future. Sleep. 2015; Jun. 38(6):899–906.
Article49. Kumar AT, Vasconcellos A, Boon M, Huntley C. Inclusion of the first cervical nerve does not influence outcomes in upper airway stimulation for treatment of obstructive sleep apnea. Laryngoscope. 2020; May. 130(5):E382–85.
Article50. Schwab RJ, Wang SH, Verbraecken J, Vanderveken OM, Van de Heyning P, Vos WG, et al. Anatomic predictors of response and mechanism of action of upper airway stimulation therapy in patients with obstructive sleep apnea. Sleep. 2018; Apr. 41(4):
Article51. Heiser C, Knopf A, Hofauer B. Surgical anatomy of the hypoglossal nerve: a new classification system for selective upper airway stimulation. Head Neck. 2017; Dec. 39(12):2371–80.
Article52. Strollo PJ Jr, Soose RJ, Maurer JT, de Vries N, Cornelius J, Froymovich O, et al. Upper-airway stimulation for obstructive sleep apnea. N Engl J Med. 2014; Jan. 370(2):139–49.
Article53. Kompelli AR, Ni JS, Nguyen SA, Lentsch EJ, Neskey DM, Meyer TA. The outcomes of hypoglossal nerve stimulation in the management of OSA: a systematic review and meta-analysis. World J Otorhinolaryngol Head Neck Surg. 2018; Sep. 5(1):41–8.54. Costantino A, Rinaldi V, Moffa A, Luccarelli V, Bressi F, Cassano M, et al. Hypoglossal nerve stimulation long-term clinical outcomes: a systematic review and meta-analysis. Sleep Breath. 2020; Jun. 24(2):399–411.
Article55. Hofauer B, Steffen A, Knopf A, Hasselbacher K, Heiser C. Adherence to upper-airway stimulation in the treatment of OSA. Chest. 2018; Feb. 153(2):574–5.
Article56. Bohorquez D, Mahmoud AF, Yu JL, Thaler ER. Upper airway stimulation therapy and sleep architecture in patients with obstructive sleep apnea. Laryngoscope. 2020; Apr. 130(4):1085–9.
Article57. Walia HK, Thompson NR, Strohl KP, Faulx MD, Waters T, Kominsky A, et al. Upper airway stimulation vs positive airway pressure impact on BP and sleepiness symptoms in OSA. Chest. 2020; Jan. 157(1):173–83.58. Withrow K, Evans S, Harwick J, Kezirian E, Strollo P. Upper airway stimulation response in older adults with moderate to severe obstructive sleep apnea. Otolaryngol Head Neck Surg. 2019; Oct. 161(4):714–9.
Article59. Huntley C, Steffen A, Doghramji K, Hofauer B, Heiser C, Boon M. Upper airway stimulation in patients with obstructive sleep apnea and an elevated body mass index: a multi-institutional review. Laryngoscope. 2018; Oct. 128(10):2425–8.
Article60. Caples SM, Rowley JA, Prinsell JR, Pallanch JF, Elamin MB, Katz SG, et al. Surgical modifications of the upper airway for obstructive sleep apnea in adults: a systematic review and meta-analysis. Sleep. 2010; Oct. 33(10):1396–407.
Article61. Abramson Z, Susarla SM, Lawler M, Bouchard C, Troulis M, Kaban LB. Three-dimensional computed tomographic airway analysis of patients with obstructive sleep apnea treated by maxillomandibular advancement. J Oral Maxillofac Surg. 2011; Mar. 69(3):677–86.
Article62. Hong SO, Poomkonsarn S, Millesi G, Liu SY. Upper airway stimulation as an alternative to maxillomandibular advancement for obstructive sleep apnoea in a patient with dentofacial deformity: case report with literature review. Int J Oral Maxillofac Surg. 2019; Dec. 21. S0901-5027(19):31275–5.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Skeletal Surgery in Obstructive Sleep Apnea
- Surgical Algorithm for Obstructive Sleep Apnea: An Update
- Awake cephalometric analysis of posterior airway space and calculated resistance related to respiratory disturbance index before and after maxillomandibular advancement for obstructive sleep apnea
- Three-dimensional analysis of changes in airway space after bimaxillary orthognathic surgery with maxillomandibular setback and their association with obstructive sleep apnea
- Two Cases of Pediatric Obstructive Hypoventilation Managed with Upper Airway Surgery