Ann Surg Treat Res.
2020 Aug;99(2):65-71. 10.4174/astr.2020.99.2.65.
Hepatocellular carcinoma in old age: are there any benefits of liver resection in old age?
- Affiliations
-
- 1Department of Surgery, Wonju Severance Christian Hospital, Yonsei University Wonju College of Medicine, Wonju, Korea
- 2Department of Internal Medicine, Wonju Severance Christian Hospital, Yonsei University Wonju College of Medicine, Wonju, Korea
- KMID: 2504818
- DOI: http://doi.org/10.4174/astr.2020.99.2.65
Abstract
- Purpose
Elderly individuals have comorbidities that can adversely affect surgical outcomes. Some studies reported that elderly patients with hepatocellular carcinoma (HCC) have higher liver- and non-liver–related deaths. Therefore, palliative treatments are preferred in these patients. We compared surgical treatment outcomes between young and old age groups.
Methods
In total, 233 liver resections were performed in patients with HCC from March 2012 to December 2018. We retrospectively reviewed medical records. The old age group was defined as patients aged more than 70 years. We compared perioperative characteristics and surgical outcomes and analyzed the prognostic factors for disease-free survival (DFS) and overall survival (OS) rates.
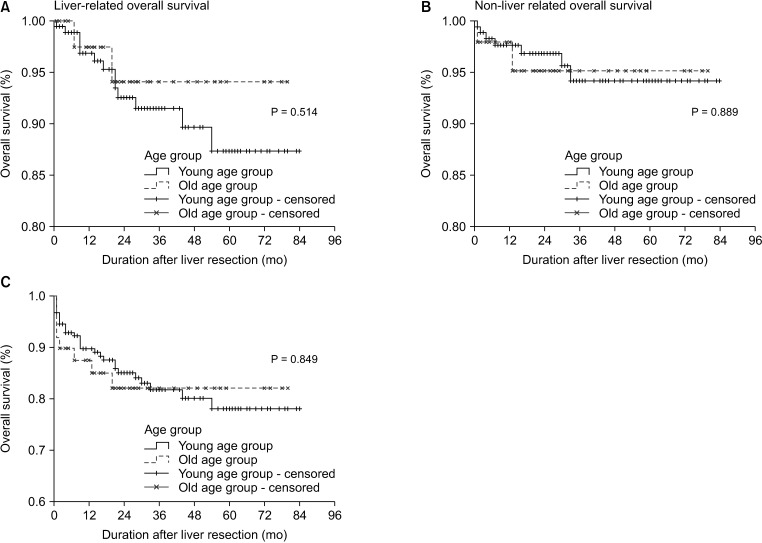
Results
The young and old age group included 184 and 49 patients, respectively. Preoperative characteristics were similar. Major liver resection rate was similar (young age group, 26.1% vs. old age group, 20.4%), but the operation time was a little bit shorter in old age group. Major postoperative complications were 23 (12.5%) and 9 (18.4%) in the young and old age group (P = 0.351). Median non-liver–related overall survival were 80 and 76 months (P = 0.889) and liver-related OS were 76 and 76 months (P = 0.514) in the young and old age groups, respectively. Age was not an independent risk factor for DFS and OS.
Conclusion
Elderly patients showed similar non-liver- and liver-related OS rates as young patients after liver resection. Postoperative complications were also similar. If elderly patients are well selected, they can receive curative treatment and show good surgical outcomes.
Figure
Cited by 1 articles
-
Realization of improved outcomes following liver resection in hepatocellular carcinoma patients aged 75 years and older
Jong Man Kim, Jinsoo Rhu, Sang Yun Ha, Gyu-Seong Choi, Choon Hyuck David Kwon, Gaabsoo Kim, Jae-Won Joh
Ann Surg Treat Res. 2021;101(5):257-265. doi: 10.4174/astr.2021.101.5.257.
Reference
-
1. Kaibori M, Yoshii K, Yokota I, Hasegawa K, Nagashima F, Kubo S, et al. Impact of advanced age on survival in patients undergoing resection of hepatocellular carcinoma: report of a Japanese nationwide survey. Ann Surg. 2019; 269:692–699. PMID: 28922205.2. National Cancer Information Center. Major cancer mortality [Internet]. Goyang: National Cancer Information Center;c2019. cited 2020 Jul 1. Available from: https://www.cancer.go.kr/lay1/S1T645C646/contents.do.3. Jung M. National Cancer Screening Programs and evidence-based healthcare policy in South Korea. Health Policy. 2015; 119:26–32. PMID: 25220569.4. Kim SH, Kang DR, Lee JG, Kim DY, Ahn SH, Han KH, et al. Early predictor of mortality due to irreversible posthepatectomy liver failure in patients with hepatocellular carcinoma. World J Surg. 2013; 37:1028–1033. PMID: 23423450.5. Turrentine FE, Wang H, Simpson VB, Jones RS. Surgical risk factors, morbidity, and mortality in elderly patients. J Am Coll Surg. 2006; 203:865–877. PMID: 17116555.6. Santambrogio R, Barabino M, Scifo G, Costa M, Giovenzana M, Opocher E. Effect of age (over 75 years) on postoperative complications and survival in patients undergoing hepatic resection for hepatocellular carcinoma. J Gastrointest Surg. 2017; 21:657–665. PMID: 28083840.7. Kutlu OC, Chan JA, Aloia TA, Chun YS, Kaseb AO, Passot G, et al. Comparative effectiveness of first-line radiofrequency ablation versus surgical resection and transplantation for patients with early hepatocellular carcinoma. Cancer. 2017; 123:1817–1827. PMID: 28085184.8. Ramesh H. Resection for hepatocellular carcinoma. J Clin Exp Hepatol. 2014; 4(Suppl 3):S90–S96. PMID: 25755617.9. Korean Liver Cancer Association. National Cancer Center. 2018 Korean Liver Cancer Association-National Cancer Center Korea practice guidelines for the management of hepatocellular carcinoma. Gut Liver. 2019; 13:227–299. PMID: 31060120.10. Hammad AY, Robbins JR, Turaga KK, Christians KK, Gamblin TC, Johnston FM. Palliative interventions for hepatocellular carcinoma patients: analysis of the National Cancer Database. Ann Palliat Med. 2017; 6:26–35. PMID: 28061532.11. Guo H, Wu T, Lu Q, Dong J, Ren YF, Nan KJ, et al. Hepatocellular carcinoma in elderly: clinical characteristics, treatments and outcomes compared with younger adults. PLoS One. 2017; 12:e0184160. PMID: 28886106.12. Dahiya D, Wu TJ, Lee CF, Chan KM, Lee WC, Chen MF. Minor versus major hepatic resection for small hepatocellular carcinoma (HCC) in cirrhotic patients: a 20-year experience. Surgery. 2010; 147:676–685. PMID: 20004441.13. Lim JH, Choi GH, Choi SH, Lee HS, Kim KS, Choi JS. Ventral segment-preserving right hepatectomy in patients with hepatocellular carcinoma. World J Surg. 2015; 39:1034–1043. PMID: 25446484.14. Bulathsinhala BKS, Tillekaratne MSB, Gunatilleke MB, Niriella MA, Wijegunawardena DGA, Siriwardana RC. Outcome of hepatic resection: First five-year experience in elderly and younger patients. Ceylon Med J. 2018; 63:43–45. PMID: 29764097.15. Inoue Y, Tanaka R, Fujii K, Kawaguchi N, Ishii M, Masubuchi S, et al. Surgical outcome and hepatic regeneration after hepatic resection for hepatocellular carcinoma in elderly patients. Dig Surg. 2019; 36:289–301. PMID: 29758561.16. Mastoraki A, Tsakali A, Papanikolaou IS, Danias N, Smyrniotis V, Arkadopoulos N. Outcome following major hepatic resection in the elderly patients. Clin Res Hepatol Gastroenterol. 2014; 38:462–466. PMID: 24582424.17. Zarour LR, Billingsley KG, Walker BS, Enestvedt CK, Orloff SL, Maynard E, et al. Hepatic resection of solitary HCC in the elderly: a unique disease in a growing population. Am J Surg. 2019; 217:899–905. PMID: 30819401.18. Zhao LY, Huo RR, Xiang X, Torzilli G, Zheng MH, Yang T, et al. Hepatic resection for elderly patients with hepatocellular carcinoma: a systematic review of more than 17,000 patients. Expert Rev Gastroenterol Hepatol. 2018; 12:1059–1068. PMID: 30145919.19. Hamaoka M, Kobayashi T, Ishiyama K, Ohira M, Tahara H, Kuroda S, et al. Evaluation of the risk factors and prognostic factors of hepatectomy for hepatocellular carcinoma in patients aged 80 years or more. J Hepatobiliary Pancreat Sci. 2017; 24:58–64. PMID: 27860361.20. Ide T, Miyoshi A, Kitahara K, Noshiro H. Prediction of postoperative complications in elderly patients with hepatocellular carcinoma. J Surg Res. 2013; 185:614–619. PMID: 23932657.21. Ruzzenente A, Conci S, Ciangherotti A, Campagnaro T, Valdegamberi A, Bertuzzo F, et al. Impact of age on short-term outcomes of liver surgery: lessons learned in 10-years' experience in a tertiary referral hepato-pancreato-biliary center. Medicine (Baltimore). 2017; 96:e6955. PMID: 28514317.22. de la Fuente SG, Bennett KM, Scarborough JE. Functional status determines postoperative outcomes in elderly patients undergoing hepatic resections. J Surg Oncol. 2013; 107:865–870. PMID: 23585324.23. Jang JS, Shin DG, Cho HM, Kwon Y, Cho DH, Lee KB, et al. Differences in the survival of gastric cancer patients after gastrectomy according to the medical insurance status. J Gastric Cancer. 2013; 13:247–254. PMID: 24511421.24. Ahn SH, Kim SH, Choi GH, Choi JS, Kim KS. The optimal follow-up period in patients with above 5-year disease-free survival after curative liver resection for hepatocellular carcinoma. J Korean Surg Soc. 2013; 85:269–274. PMID: 24368984.25. Tan JT, Zhao C, Peng NF, Yang Y, Zhong JH, Yang T, et al. Association between age and overall survival of patients with hepatocellular carcinoma after hepatic resection. J Surg Oncol. 2016; 114:966–970. PMID: 27633143.26. Wei F. Does an extreme age (≥80 years) affect outcomes in patients after liver cancer surgery? A meta-analysis. ANZ J Surg. 2019; 89:25–31. PMID: 29885205.27. Yamada S, Shimada M, Miyake H, Utsunomiya T, Morine Y, Imura S, et al. Outcome of hepatectomy in super-elderly patients with hepatocellular carcinoma. Hepatol Res. 2012; 42:454–458. PMID: 22295877.28. Cucchetti A, Sposito C, Pinna AD, Citterio D, Ercolani G, Flores M, et al. Effect of age on survival in patients undergoing resection of hepatocellular carcinoma. Br J Surg. 2016; 103:e93–e99. PMID: 26662121.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Surgical Perspectives of Hepatocellular Carcinoma beyond the Barcelona Clinical Liver Cancer Guideline; Focusing on Liver Resection
- Survival rate of hepatectomy according to liver cirrhosis in hepatoculluar carcinoma
- Surgical Management of Hepatocellular Carcinoma
- Fibrolamellar hepatocellular carcinoma that was successfully treated with surgical resection: a case report
- Histopathologic consideration of hepatocellular carcinoma