Korean J Gastroenterol.
2020 Jun;75(6):351-355. 10.4166/kjg.2020.75.6.351.
Gallbladder Perforation after Transarterial Chemoembolization in a Patient with a Huge Hepatocellular Carcinoma
- Affiliations
-
- 1Departments of Internal Medicine, Kosin University College of Medicine, Busan, Korea
- 2Departments of Radiology, Kosin University College of Medicine, Busan, Korea
- KMID: 2504378
- DOI: http://doi.org/10.4166/kjg.2020.75.6.351
Abstract
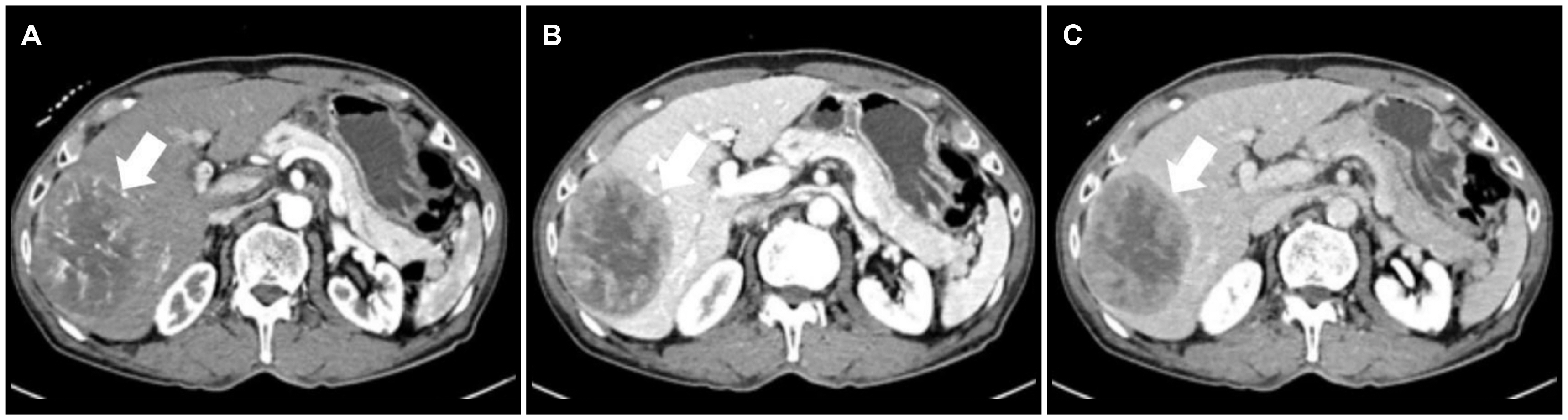
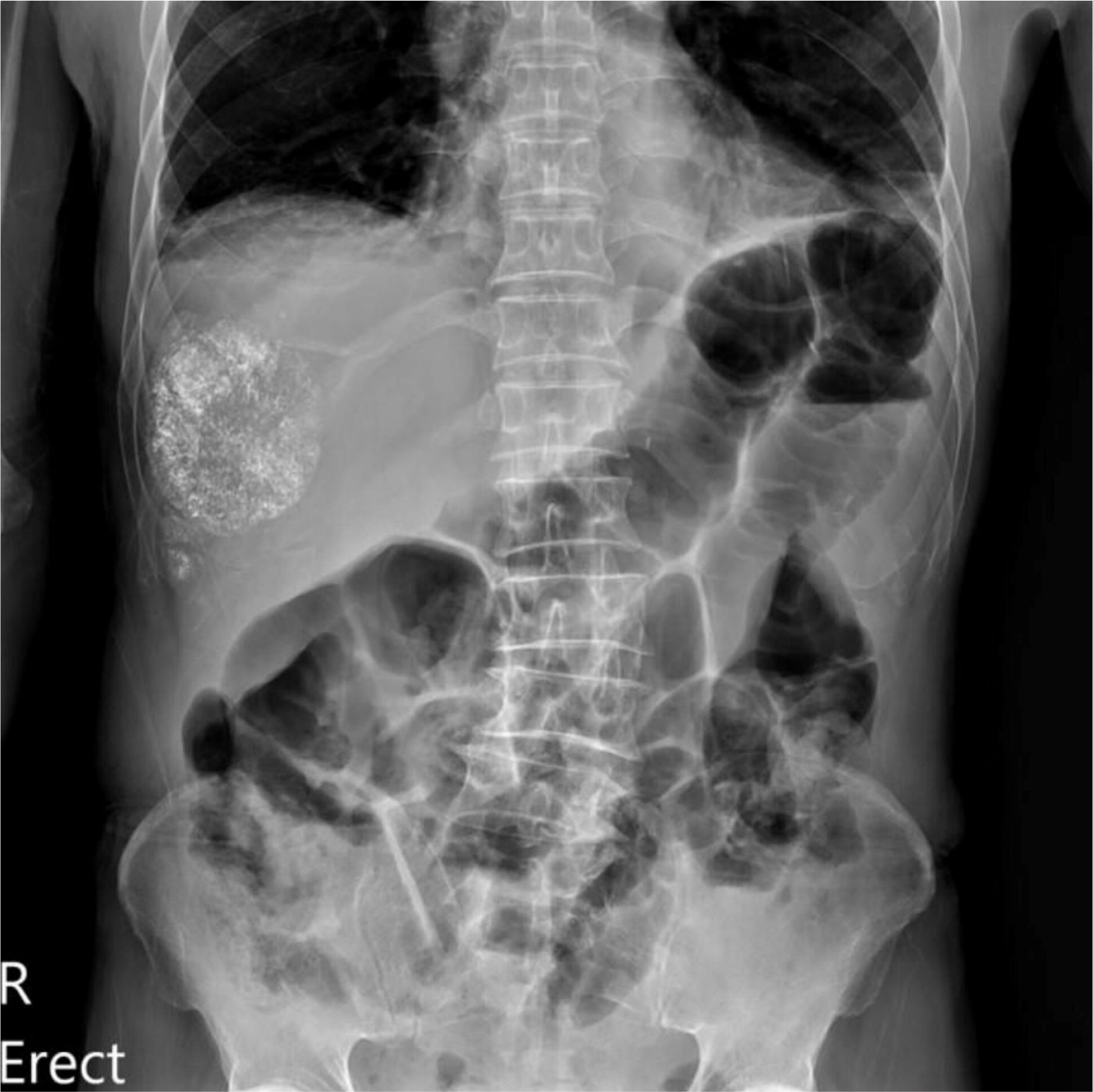
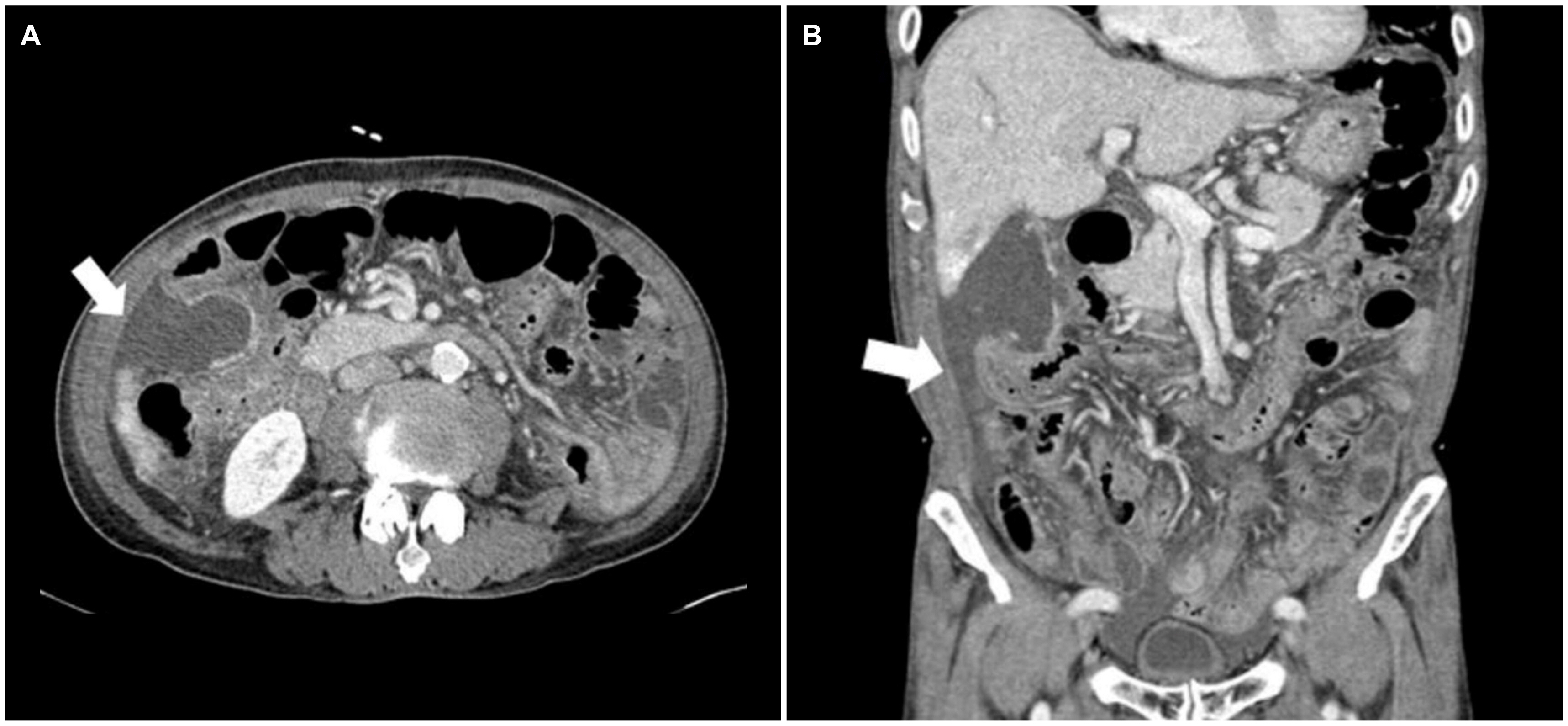
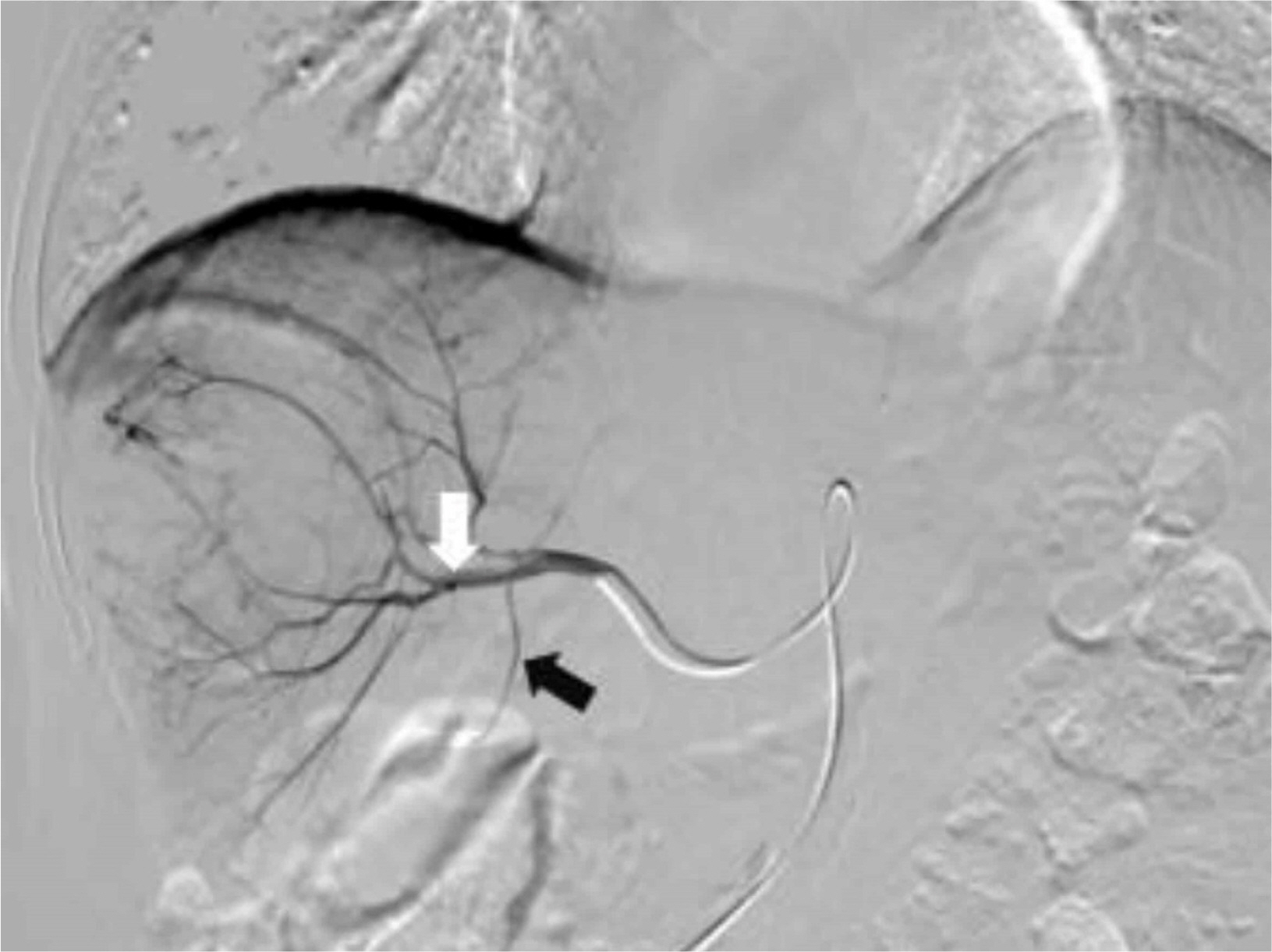
- Transarterial chemoembolization (TACE) is a common treatment for unresectable hepatocellular carcinoma (HCC). The most common complications after TACE are non-specific symptoms called post-embolization syndrome, such as abdominal pain or fever. Rare complications, such as liver failure, liver abscess, sepsis, pulmonary embolism, cholecystitis, can also occur. On the other hand, gallbladder perforation is quite rare. This paper reports a case of gallbladder perforation following TACE. A 76-year-old male with a single 9-cm-sized HCC underwent TACE. Five days after TACE, he developed persistent right upper quadrant pain and ileus. An abdomen CT scan confirmed gallbladder perforation with bile in the right paracolic gutter and pelvic cavity. Percutaneous transhepatic gallbladder drainage was performed with the intravenous administration of antibiotics. After 1 month, the patient underwent right hemihepatectomy and cholecystectomy. Physicians should consider the possibility of gallbladder perforation, which is a rare complication after TACE, when unexplained abdominal pain persists.
Figure
Reference
-
1. Korean Liver Cancer Association (KLCA) and National Cancer Center (NCC). 2019; 2018 Korean Liver Cancer Association-National Cancer Center Korea practice guidelines for the management of hepatocellular carcinoma. Korean J Radiol. 20:1042–1113. DOI: 10.3348/kjr.2019.0140. PMID: 31270974. PMCID: PMC6609431.2. Llovet JM, Bruix J. 2003; Systematic review of randomized trials for unresectable hepatocellular carcinoma: chemoembolization improves survival. Hepatology. 37:429–442. DOI: 10.1053/jhep.2003.50047. PMID: 12540794.
Article3. Paik YH, Chon CY, Cho JY, et al. 2005; Risk factors of acute hepatic failure associated with transcatheter arterial chemoembolization for hepatocellular carcinoma. Korean J Med. 69:622–630.4. Wagnetz U, Jaskolka J, Yang P, Jhaveri KS. 2010; Acute ischemic cholecystitis after transarterial chemoembolization of hepatocellular carcinoma: incidence and clinical outcome. J Comput Assist Tomogr. 34:348–353. DOI: 10.1097/RCT.0b013e3181caaea3. PMID: 20498534.5. Tu J, Jia Z, Ying X, et al. 2016; The incidence and outcome of major complication following conventional TAE/TACE for hepatocellular carcinoma. Medicine (Baltimore). 95:e5606. DOI: 10.1097/MD.0000000000005606. PMID: 27930585. PMCID: PMC5266057.
Article6. Lim EJ, Spanger M, Lubel JS. 2013; Gallbladder perforation following transarterial chemoembolisation; a rare but serious complication. Frontline Gastroenterol. 4:135–137. DOI: 10.1136/flgastro-2012-100216. PMID: 28839714. PMCID: PMC5369796.
Article7. Clark TW. 2006; Complications of hepatic chemoembolization. Semin Intervent Radiol. 23:119–125. DOI: 10.1055/s-2006-941442. PMID: 21326755. PMCID: PMC3036366.
Article8. Leung DA, Goin JE, Sickles C, Raskay BJ, Soulen MC. 2001; Determinants of postembolization syndrome after hepatic chemoembolization. J Vasc Interv Radiol. 12:321–326. DOI: 10.1016/S1051-0443(07)61911-3. PMID: 11287509.
Article9. Chan AO, Yuen MF, Hui CK, Tso WK, Lai CL. 2002; A prospective study regarding the complications of transcatheter intraarterial lipiodol chemoembolization in patients with hepatocellular carcinoma. Cancer. 94:1747–1752. DOI: 10.1002/cncr.10407. PMID: 11920537.
Article10. Yamaguchi T, Seki T, Komemushi A, et al. 2018; Acute necrotizing pancreatitis as a fatal complication following DC bead transcatheter arterial chemoembolization for hepatocellular carcinoma: a case report and review of the literature. Mol Clin Oncol. 9:403–407. DOI: 10.3892/mco.2018.1690. PMID: 30214729. PMCID: PMC6125694.11. McWilliams JP, Kee ST, Loh CT, Lee EW, Liu DM. 2011; Prophylactic embolization of the cystic artery before radioembolization: feasibility, safety, and outcomes. Cardiovasc Intervent Radiol. 34:786–792. DOI: 10.1007/s00270-010-0021-x. PMID: 21063871. PMCID: PMC3132419.
Article12. Powerski M, Busse A, Seidensticker M, et al. 2015; Prophylactic embolization of the cystic artery prior to radioembolization of liver malignancies-an evaluation of necessity. Cardiovasc Intervent Radiol. 38:678–684. DOI: 10.1007/s00270-015-1088-1. PMID: 25823575.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Combined Transarterial Chemoembolization and External Beam Radiotherapy in a Patient with Recurrent Huge Hepatocellular Carcinoma after Hepatic Resection
- Complications Related to Transarterial Treatment of Hepatocellular Carcinoma: A Comprehensive Review
- Efficacy of Hepatic Arterial Infusion Chemotherapy and Radiofrequency Ablation against Hepatocellular Carcinoma Refractory to Transarterial Chemoembolization and Vascular Variation: A Case Study
- A Case of Emphysematous Cholecystitis and Pneumobilia after Transarterial Chemoembolization for Hepatocellular Carcinoma
- Transarterial Chemoembolization in Patients with Hepatocellular Carcinoma and Extrahepatic Metastasis