J Surg Ultrasound.
2020 May;7(1):7-13. 10.46268/jsu.2020.7.1.7.
Comparative Accuracy of Preoperative Tumor Size Assessment on Breast Ultrasonography and Magnetic Resonance Imaging in Young Breast Cancer Patients
- Affiliations
-
- 1Division of BreastㆍThyroid Surgery, Department of Surgery, Jeonbuk National University Medical School, Korea
- 2Departmenet of Radiology, Jeonbuk National University Medical School, Jeonju, Korea
- KMID: 2502953
- DOI: http://doi.org/10.46268/jsu.2020.7.1.7
Abstract
- Purpose
Breast cancer in young women deserves special consideration, such as dense breast, more aggressive progression, and oncoplastic surgery. Magnetic resonance imaging (MRI) is a more recent modality than ultrasonography (US), but the role of MRI in patients with a dense breast is still controversial. This comparative study analyzed the relationship between the preoperative radiological and the postoperative pathological tumor size for young breast cancer patients.
Methods
All breast cancers diagnosed in patients 45 years or younger from January 2016 to December 2018 were reviewed. Tumor size measurements obtained on breast US and MRI were compared for accuracy with those obtained in the final pathology results. Patients with only microcalcification on imaging modalities and those who had undergone neoadjuvant chemotherapy were excluded.
Results
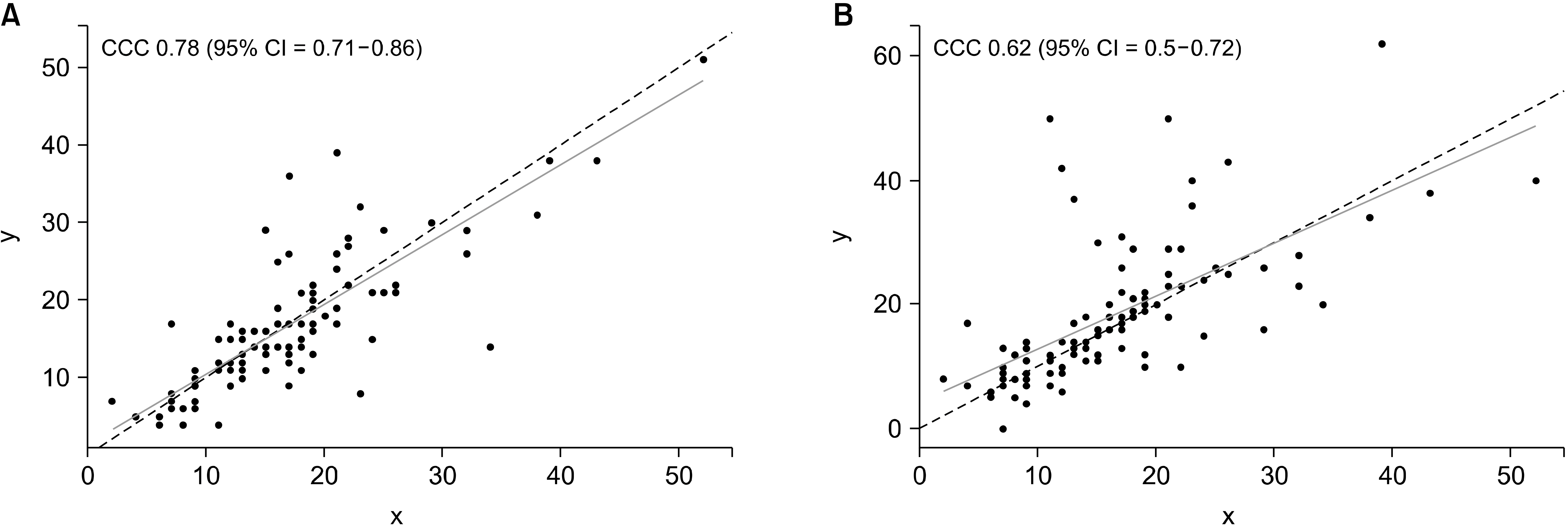
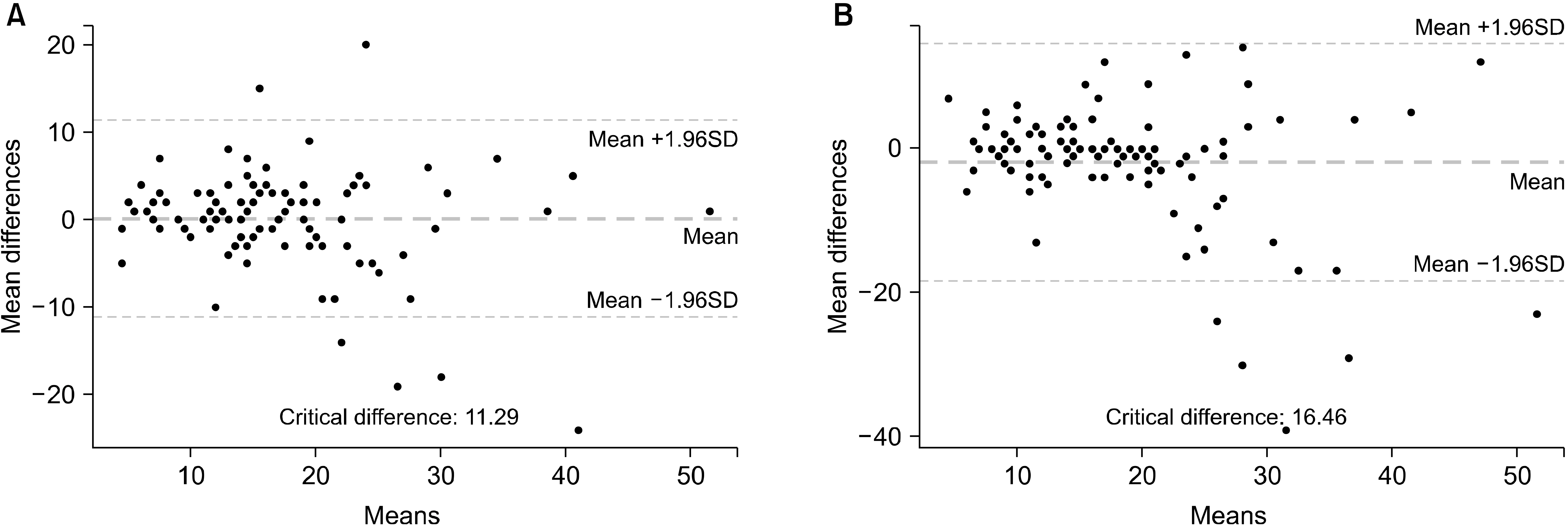
A total of 103 breast cancer patients were included in this study. Of the 103 breast cancers with both imaging modalities performed, 86 (83.5%) were infiltrating ductal carcinomas and 17 (16.5%) were ductal carcinoma in situ. The mean tumor size measured on MRI was significantly greater than that measured on pathology (18.5 ± 11.0 mm vs. 16.6 ± 8.5 mm), whereas the sizes measured on US was not significantly different from that measured on pathology (16.5 ± 9.5 mm vs. 16.6 ± 8.5 mm). The tumor size measured on MRI was greater than that measured on US.
Conclusion
Measurements taken by US were more accurate in measuring the tumor size in patients 45 years of age or younger than MRI.
Figure
Reference
-
Kang SY., Kim YS., Kim Z., Kim HY., Kim HJ., Park S, et al. 2020. Breast cancer statistics in Korea in 2017: data from a Breast Cancer Registry. J Breast Cancer. 23:115–28. DOI: 10.4048/jbc.2020.23.e24. PMID: 32395372. PMCID: PMC7192743.
ArticleHwang KT., Kim H., Chung JK., Jung IM., Heo SC., Ahn YJ, et al. 2010. A comparative study between the preoperative diagnostic tumor size and the postoperative pathologic tumor size in patients with breast tumors. J Breast Cancer. 13:187–97. DOI: 10.4048/jbc.2010.13.2.187.
ArticleLeddy R., Irshad A., Metcalfe A., Mabalam P., Abid A., Ackerman S, et al. 2016. Comparative accuracy of preoperative tumor size assessment on mammography, sonography, and MRI: is the accuracy affected by breast density or cancer subtype? J Clin Ultrasound. 44:17–25. DOI: 10.1002/jcu.22290. PMID: 26294391.
ArticleRamirez SI., Scholle M., Buckmaster J., Paley RH., Kowdley GC. 2012. Breast cancer tumor size assessment with mammography, ultrasonography, and magnetic resonance imaging at a community based multidisciplinary breast center. Am Surg. 78:440–6. PMID: 22472402.
ArticleKang SY., Choi EJ., Youn HJ., Jung SH. 2016. Accuracy of preoperative tumor size assessment on ultrasonography and magnetic resonance imaging in breast cancer. J Surg Ultrasound. 3:24–9.Lai HW., Chen DR., Wu YC., Chen CJ., Lee CW., Kuo SJ, et al. 2015. Comparison of the diagnostic accuracy of magnetic resonance imaging with sonography in the prediction of breast cancer tumor size: a concordance analysis with histopathologically determined tumor size. Ann Surg Oncol. 22:3816–23. DOI: 10.1245/s10434-015-4424-4. PMID: 25707494.
ArticleRudat V., Nour A., Almuraikhi N., Ghoniemy I., Brune-Erber I., Almasri N, et al. 2015. MRI and ultrasonography for assessing multifocal disease and tumor size in breast cancer: comparison with histopathological results. Gulf J Oncolog. 1:65–72. PMID: 25682455.Shin HJ., Ko ES., Yi A. 2015. Breast cancer screening in Korean woman with dense breast tissue. J Korean Soc Radiol. 73:279–86. DOI: 10.3348/jksr.2015.73.5.279.
ArticleLee CI., Lehman CD., Bassett LW. 2018. Breast imaging. Oxford University Press;New York: p. 29–47. DOI: 10.1093/med/9780190270261.001.0001.Edwards SD., Lipson JA., Ikeda DM., Lee JM. 2013. Updates and revisions to the BI-RADS magnetic resonance imaging lexicon. Magn Reson Imaging Clin N Am. 21:483–93. DOI: 10.1016/j.mric.2013.02.005. PMID: 23928239.
ArticleEdge SB. 2010. AJCC cancer staging manual. 7th ed. Springer;New York: p. 347–76.DeSantis CE., Ma J., Goding Sauer A., Newman LA., Jemal A. 2017. Breast cancer statistics, 2017, racial disparity in mortality by state. CA Cancer J Clin. 67:439–48. DOI: 10.3322/caac.21412. PMID: 28972651.
ArticleKing V., Gu Y., Kaplan JB., Brooks JD., Pike MC., Morris EA. 2012. Impact of menopausalstatus on background parenchymal enhancement and fibroglandular tissue on breast MRI. Eur Radiol. 22:2641–7. DOI: 10.1007/s00330-012-2553-8. PMID: 22752463.
ArticleGiess CS., Raza S., Birdwell RL. 2013. Patterns of nonmasslike enhancement at screening breast MR imaging of high-risk premenopausal women. Radiographics. 33:1343–60. DOI: 10.1148/rg.335125185. PMID: 24025928.
ArticleKim JY., Lee SH., Lee JW., Kim S., Choo KS. 2015. Magnetic resonance imaging characteristics of invasive breast cancer in women aged less than 35 years. Acta Radiol. 56:924–32. DOI: 10.1177/0284185114542365. PMID: 25024441.
ArticleUematsu T., Kasami M., Watanabe J. 2011. Does the degree of background enhancement in breast MRI affect the detection and staging of breast cancer? Eur Radiol. 21:2261–7. DOI: 10.1007/s00330-011-2175-6. PMID: 21688006.
ArticleKang SY., Kim YS., Kim Z., Kim HY., Lee SK., Jung KW, et al. 2018. Basic findings regarding breast cancer in Korea in 2015: data from a Breast Cancer Registry. J Breast Cancer. 21:1–10. DOI: 10.4048/jbc.2018.21.1.1. PMID: 29628978. PMCID: PMC5880959.
ArticleBehjatnia B., Sim J., Bassett LW., Moatamed NA., Apple SK. 2010. Does size matter? Comparison study between MRI, gross, and microscopic tumor sizes in breast cancer in lumpectomy specimens. Int J Clin Exp Pathol. 3:303–9. PMID: 20224728. PMCID: PMC2836507.Jethava A., Ali S., Wakefield D., Crowell R., Sporn J., Vrendenburgh J. 2015. Diagnostic accuracy of MRI in predicting breast tumor size: comparative analysis of MRI vs histopathological assessed breast tumor size. Conn Med. 79:261–7. PMID: 26245013.Leddy R., Irshad A., Metcalfe A., Mabalam P., Abid A., Ackerman S, et al. 2016. Comparative accuracy of preoperative tumor size assessment on mammography, sonography, and MRI: is the accuracy affected by breast density or cancer subtype? J Clin Ultrasound. 44:17–25. DOI: 10.1002/jcu.22290. PMID: 26294391.
ArticleGiess CS., Raza S., Birdwell RL. 2013. Patterns of nonmasslike enhancement at screening breast MR imaging of high-risk premenopausal women. Radiographics. 33:1343–60. DOI: 10.1148/rg.335125185. PMID: 24025928.
ArticleGiess CS., Yeh ED., Raza S., Birdwell RL. 2014. Background parenchymal enhancement at breast MR imaging: normal patterns, diagnostic challenges, and potential for false-positive and false-negative interpretation. Radiographics. 34:234–47. DOI: 10.1148/rg.341135034. PMID: 24428293.
ArticleTeifke A., Hlawatsch A., Beier T., Werner Vomweg T., Schadmand S., Schmidt M, et al. 2002. Undetected malignancies of the breast: dynamic contrast-enhanced MR imaging at 1.0 T. Radiology. 224:881–8. DOI: 10.1148/radiol.2243010547. PMID: 12202728.
ArticleIrshad A., Leddy R., Pisano E., Baker N., Lewis M., Ackerman S, et al. 2013. Assessing the role of ultrasound in predicting the biological behavior of breast cancer. AJR Am J Roentgenol. 200:284–90. DOI: 10.2214/AJR.12.8781. PMID: 23345347.
ArticleKuhl CK., Bieling HB., Gieseke J., Kreft BP., Sommer T., Lutterbey G, et al. 1997. Healthy premenopausal breast parenchyma in dynamic contrast-enhanced MR imaging of the breast: normal contrast medium enhancement and cyclical-phase dependency. Radiology. 203:137–44. DOI: 10.1148/radiology.203.1.9122382. PMID: 9122382.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Differences of Tumor Size Measured by Ultrasonography and Magnetic Resonance Imaging Compared to Pathological Tumor Size in Primary Breast Cancer
- Comparative Accuracy of Preoperative Tumor Size Assessment on Ultrasonography and Magnetic Resonance Imaging in Ductal Carcinoma In Situ
- Analysis of Tumor Size between Imaging of Preoperative Ultrasound, MRI and Pathologic Measurements in Early Breast Carcinoma
- The Role and Significance of Preoperative Breast MRI in the Setting of Breast Cancer
- Clinical Mammographic, and Ultrasonographic Assessment of Breast Cancer Sizes