J Korean Foot Ankle Soc.
2020 Jun;24(2):48-54. 10.14193/jkfas.2020.24.2.48.
Operative Treatment of Osteochondral Lesion of the Talus: Arthroscopic Bone Marrow Stimulation (Multiple Drilling or Microfracture)
- Affiliations
-
- 1Department of Orthopedic Surgery, Inje University Busan Paik Hospital, Korea
- 2Department of Orthopedic Surgery, Good Samsun Hospital, Busan, Korea
- KMID: 2502909
- DOI: http://doi.org/10.14193/jkfas.2020.24.2.48
Abstract
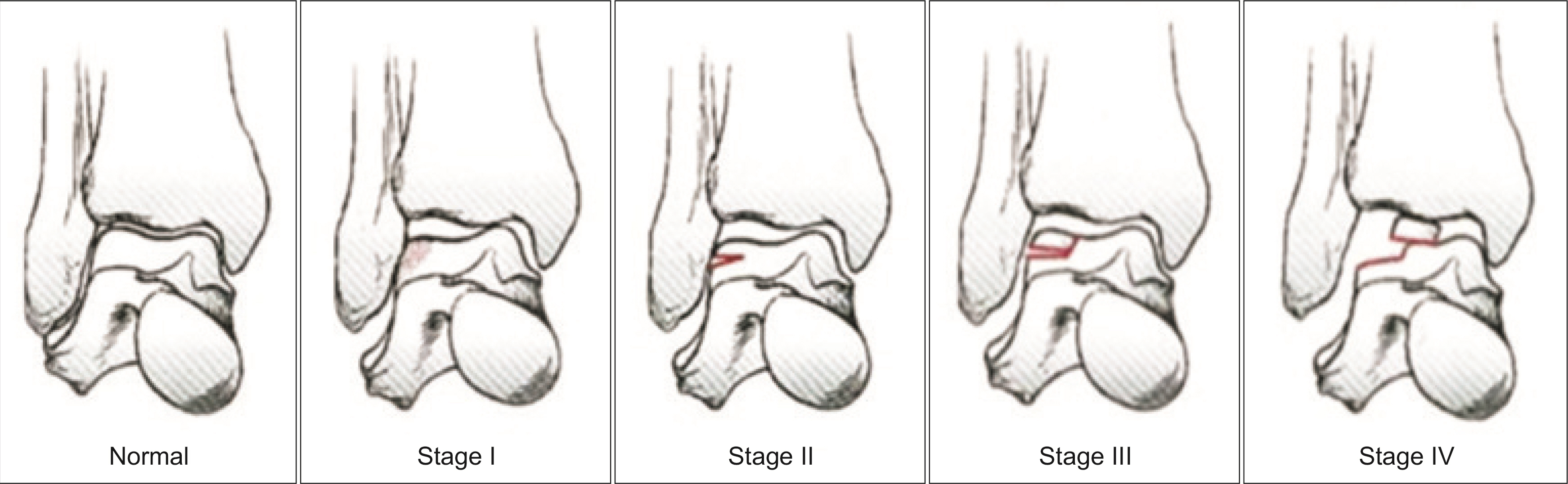
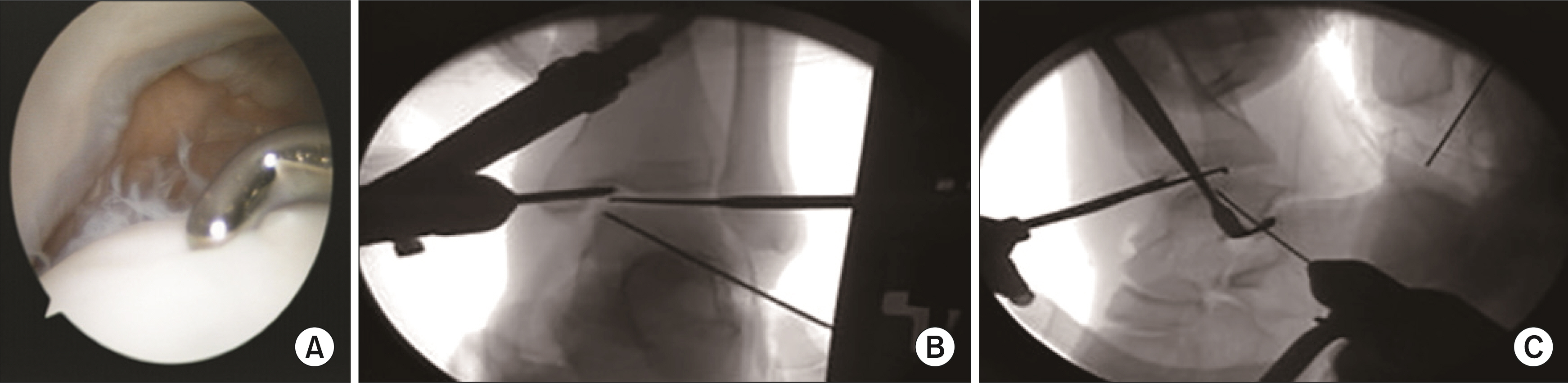
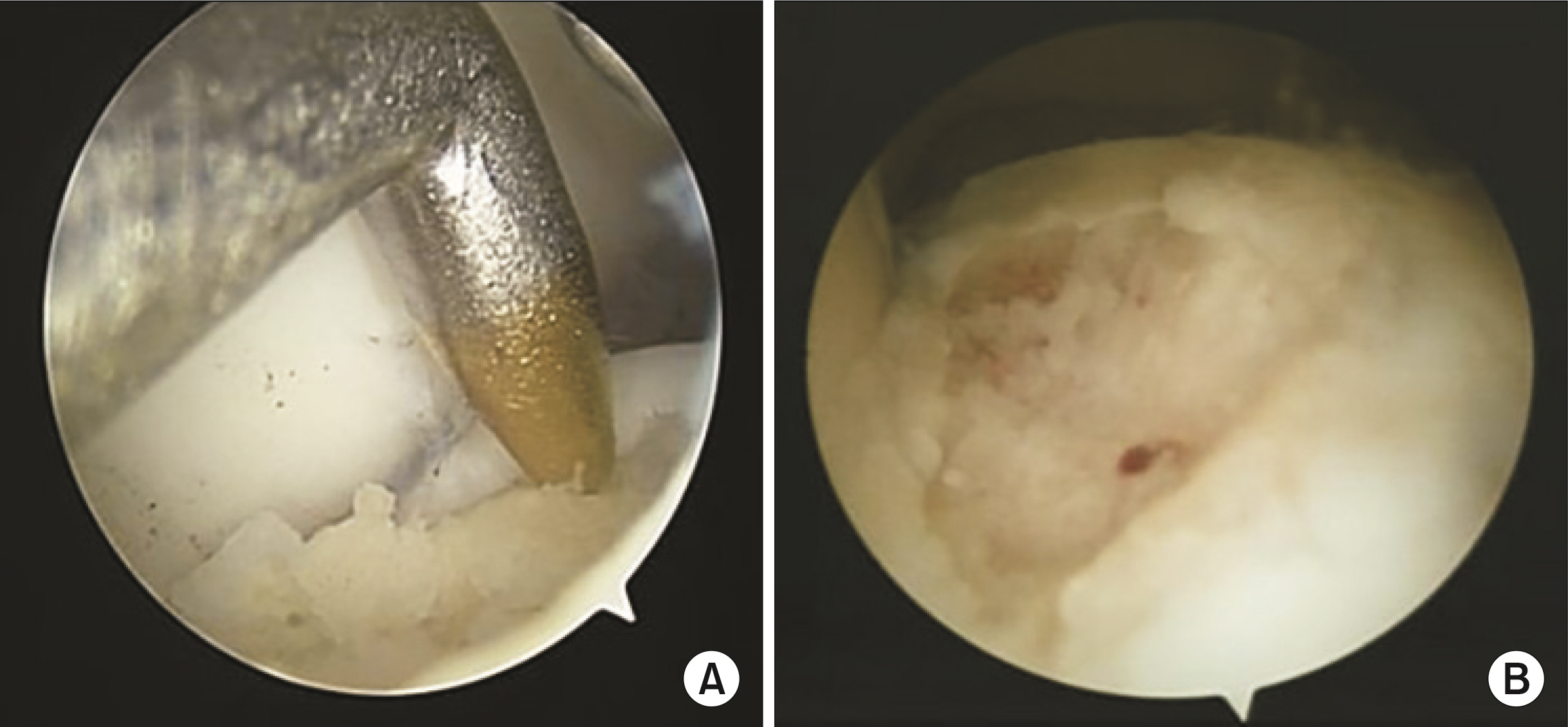
- Osteochondral lesion of the talus (OLT) is a broad term used to describe an injury or abnormality of the talar articular cartilage and adjacent bone. Various terms are used to describe this clinical entity, including osteochondritis dissecans, osteochondral fractures, and osteochondral defects. Several treatment options are available; the choice of treatment is based on the type and size of the defect and the treating clinician’s preference. Arthroscopic microfracture (a bone marrow stimulation technique) is a common and effective surgical strategy in patients with small lesions or in those in whom non-operative treatment has failed. This study had the following aims: 1) to review the historical background, etiology, and classification systems of OLT; 2) to describe a systematic approach to arthroscopic bone marrow stimulation for OLT; and 3) to determine the characteristics that are useful for assessing osteochondral lesions, including age, size, type (chondral, subchondral, cystic), stability, displacement, location, and containment of the lesion.
Figure
Reference
-
1. Monro A. 1783. Part of the cartilage of the joint, separated and ossified. Ruddimans;Edinburgh: p. 19.2. Steadman JR, Rodkey WG, Rodrigo JJ. 2001; Microfracture: surgical technique and rehabilitation to treat chondral defects. Clin Orthop Relat Res. (391 Suppl):S362–9. doi: 10.1097/00003086-200110001-00033. DOI: 10.1097/00003086-200110001-00033. PMID: 11603719.
Article3. Steele JR, Dekker TJ, Federer AE, Liles JL, Adams SB, Easley ME. Osteochondral lesions of the talus: current concepts in diagnosis and treatment. Foot Ankle Orthop. Published online July 27, 2018; doi: 10.1177/2473011418779559. DOI: 10.1177/2473011418779559.4. Baums MH, Schultz W, Kostuj T, Klinger HM. 2014; Cartilage repair techniques of the talus: an update. World J Orthop. 5:171–9. doi: 10.5312/wjo.v5.i3.171. DOI: 10.5312/wjo.v5.i3.171. PMID: 25035819. PMCID: PMC4095009.
Article5. Berndt AL, Harty M. 1959; Transchondral fractures (osteochondritis dissecans) of the talus. J Bone Joint Surg Am. 41:988–1020. DOI: 10.2106/00004623-195941060-00002. PMID: 13849029.
Article6. Schachter AK, Chen AL, Reddy PD, Tejwani NC. 2005; Osteochondral lesions of the talus. J Am Acad Orthop Surg. 13:152–8. doi: 10.5435/00124635-200505000-00002. DOI: 10.5435/00124635-200505000-00002. PMID: 15938604.
Article7. Dekker TJ, Dekker PK, Tainter DM, Easley ME, Adams SB. 2017; Treatment of osteochondral lesions of the talus: a critical analysis review. JBJS Rev. 5:01874474-201703000-00001. DOI: 10.2106/JBJS.RVW.16.00065. PMID: 28359070.8. Bosien WR, Staples OS, Russell SW. 1955; Residual disability following acute ankle sprains. J Bone Joint Surg Am. 37:1237–43. DOI: 10.2106/00004623-195537060-00011. PMID: 13271470.
Article9. Schenck RC Jr, Goodnight JM. 1996; Osteochondritis dissecans. J Bone Joint Surg Am. 78:439–56. DOI: 10.2106/00004623-199603000-00018. PMID: 8613454.10. Tol JL, Struijs PA, Bossuyt PM, Verhagen RA, van Dijk CN. 2000; Treatment strategies in osteochondral defects of the talar dome: a systematic review. Foot Ankle Int. 21:119–26. doi: 10.1177/107110070002100205. DOI: 10.1177/107110070002100205. PMID: 10694023.
Article11. Taranow WS, Bisignani GA, Towers JD, Conti SF. 1999; Retrograde drilling of osteochondral lesions of the medial talar dome. Foot Ankle Int. 20:474–80. doi: 10.1177/107110079902000802. DOI: 10.1177/107110079902000802. PMID: 10473056.
Article12. Kono M, Takao M, Naito K, Uchio Y, Ochi M. 2006; Retrograde drilling for osteochondral lesions of the talar dome. Am J Sports Med. 34:1450–6. doi: 10.1177/0363546506287300. DOI: 10.1177/0363546506287300. PMID: 16636347.
Article13. Zengerink M, Struijs PA, Tol JL, van Dijk CN. 2010; Treatment of osteochondral lesions of the talus: a systematic review. Knee Surg Sports Traumatol Arthrosc. 18:238–46. doi: 10.1007/s00167-009-0942-6. DOI: 10.1007/s00167-009-0942-6. PMID: 19859695. PMCID: PMC2809940.
Article14. Anders S, Lechler P, Rackl W, Grifka J, Schaumburger J. 2012; Fluoroscopy-guided retrograde core drilling and cancellous bone grafting in osteochondral defects of the talus. Int Orthop. 36:1635–40. doi: 10.1007/s00264-012-1530-9. DOI: 10.1007/s00264-012-1530-9. PMID: 22491802. PMCID: PMC3535023.
Article15. Ferkel RD, Zanotti RM, Komenda GA, Sgaglione NA, Cheng MS, Applegate GR, et al. 2008; Arthroscopic treatment of chronic osteochondral lesions of the talus: long-term results. Am J Sports Med. 36:1750–62. doi: 10.1177/0363546508316773. DOI: 10.1177/0363546508316773. PMID: 18753679.16. Lee KB, Bai LB, Chung JY, Seon JK. 2010; Arthroscopic microfracture for osteochondral lesions of the talus. Knee Surg Sports Traumatol Arthrosc. 18:247–53. doi: 10.1007/s00167-009-0914-x. DOI: 10.1007/s00167-009-0914-x. PMID: 19779893.
Article17. van Bergen CJ, Kox LS, Maas M, Sierevelt IN, Kerkhoffs GM, van Dijk CN. 2013; Arthroscopic treatment of osteochondral defects of the talus: outcomes at eight to twenty years of follow-up. J Bone Joint Surg Am. 95:519–25. doi: 10.2106/JBJS.L.00675. DOI: 10.2106/JBJS.L.00675. PMID: 23515986.18. Polat G, Erşen A, Erdil ME, Kızılkurt T, Kılıçoğlu Ö, Aşık M. 2016; Long-term results of microfracture in the treatment of talus osteochondral lesions. Knee Surg Sports Traumatol Arthrosc. 24:1299–303. doi: 10.1007/s00167-016-3990-8. DOI: 10.1007/s00167-016-3990-8. PMID: 26831855.
Article19. Cuttica DJ, Smith WB, Hyer CF, Philbin TM, Berlet GC. 2011; Osteochondral lesions of the talus: predictors of clinical outcome. Foot Ankle Int. 32:1045–51. doi: 10.3113/FAI.2011.1045. DOI: 10.3113/FAI.2011.1045. PMID: 22338953.
Article20. Deol PB, Berlet GC, Hyer CF. Age stratification of outcomes for osteochondral lesions of the talus. In : American Orthopedic Foot and Ankle Society Summer Meeting; 2009 Jul 15-18; Vancouver, Canada.21. Knutsen G, Engebretsen L, Ludvigsen TC, Drogset JO, Grøntvedt T, Solheim E, et al. 2004; Autologous chondrocyte implantation compared with microfracture in the knee. A randomized trial. J Bone Joint Surg Am. 86:455–64. doi: 10.2106/00004623-200403000-00001. DOI: 10.2106/00004623-200403000-00001. PMID: 14996869.22. Robinson DE, Winson IG, Harries WJ, Kelly AJ. 2003; Arthroscopic treatment of osteochondral lesions of the talus. J Bone Joint Surg Br. 85:989–93. doi: 10.1302/0301-620x.85b7.13959. DOI: 10.1302/0301-620X.85B7.13959. PMID: 14516033.
Article23. Choi WJ, Kim BS, Lee JW. 2012; Osteochondral lesion of the talus: could age be an indication for arthroscopic treatment? Am J Sports Med. 40:419–24. doi: 10.1177/0363546511423739. DOI: 10.1177/0363546511423739. PMID: 21984689.24. Chuckpaiwong B, Berkson EM, Theodore GH. 2008; Microfracture for osteochondral lesions of the ankle: outcome analysis and outcome predictors of 105 cases. Arthroscopy. 24:106–12. doi: 10.1016/j.arthro.2007.07.022. DOI: 10.1016/j.arthro.2007.07.022. PMID: 18182210.
Article25. Christensen JC, Driscoll HL, Tencer AF. 1994; 1994 William J. Stickel Gold Award. Contact characteristics of the ankle joint. Part 2. The effects of talar dome cartilage defects. J Am Podiatr Med Assoc. 84:537–47. doi: 10.7547/87507315-84-11-537. DOI: 10.7547/87507315-84-11-537. PMID: 7807383.
Article26. Choi WJ, Park KK, Kim BS, Lee JW. 2009; Osteochondral lesion of the talus: is there a critical defect size for poor outcome? Am J Sports Med. 37:1974–80. doi: 10.1177/0363546509335765. DOI: 10.1177/0363546509335765. PMID: 19654429.27. Giannini S, Ceccarelli F, Girolami M, Coppola G, Ferrari A. 1989; Biological osteosynthesis in osteochondral lesions of the talus. Ital J Orthop Traumatol. 15:425–32. PMID: 2517501.28. Anderson IF, Crichton KJ, Grattan-Smith T, Cooper RA, Brazier D. 1989; Osteochondral fractures of the dome of the talus. J Bone Joint Surg Am. 71:1143–52. DOI: 10.2106/00004623-198971080-00004. PMID: 2777840.
Article29. Hepple S, Winson IG, Glew D. 1999; Osteochondral lesions of the talus: a revised classification. Foot Ankle Int. 20:789–93. doi: 10.1177/107110079902001206. DOI: 10.1177/107110079902001206. PMID: 10609707.
Article30. Ogilvie-Harris DJ, Sarrosa EA. 2000; Arthroscopic treatment of post-traumatic cysts of the talus. Arthroscopy. 16:197–201. doi: 10.1016/s0749-8063(00)90036-7. DOI: 10.1016/S0749-8063(00)90036-7. PMID: 10705333.
Article31. Lee KB, Park HW, Cho HJ, Seon JK. 2015; Comparison of arthroscopic microfracture for osteochondral lesions of the talus with and without subchondral cyst. Am J Sports Med. 43:1951–6. doi: 10.1177/0363546515584755. DOI: 10.1177/0363546515584755. PMID: 25989800.
Article32. Saxena A, Eakin C. 2007; Articular talar injuries in athletes: results of microfracture and autogenous bone graft. Am J Sports Med. 35:1680–7. doi: 10.1177/0363546507303561. DOI: 10.1177/0363546507303561. PMID: 17656737.33. Hu Y, Guo Q, Jiao C, Mei Y, Jiang D, Wang J, et al. 2013; Treatment of large cystic medial osteochondral lesions of the talus with autologous osteoperiosteal cylinder grafts. Arthroscopy. 29:1372–9. doi: 10.1016/j.arthro.2013.05.014. DOI: 10.1016/j.arthro.2013.05.014. PMID: 23906276.
Article34. Schimmer RC, Dick W, Hintermann B. 2001; The role of ankle arthroscopy in the treatment strategies of osteochondritis dissecans lesions of the talus. Foot Ankle Int. 22:895–900. doi: 10.1177/107110070102201107. DOI: 10.1177/107110070102201107. PMID: 11722142.
Article35. Lee M, Kwon JW, Choi WJ, Lee JW. 2015; Comparison of outcomes for osteochondral lesions of the talus with and without chronic lateral ankle instability. Foot Ankle Int. 36:1050–7. doi: 10.1177/1071100715581477. DOI: 10.1177/1071100715581477. PMID: 25869235.
Article36. Becher C, Driessen A, Hess T, Longo UG, Maffulli N, Thermann H. 2010; Microfracture for chondral defects of the talus: maintenance of early results at midterm follow-up. Knee Surg Sports Traumatol Arthrosc. 18:656–63. doi: 10.1007/s00167-009-1036-1. DOI: 10.1007/s00167-009-1036-1. PMID: 20130840.
Article37. Park HW, Lee KB. 2015; Comparison of chondral versus osteochondral lesions of the talus after arthroscopic microfracture. Knee Surg Sports Traumatol Arthrosc. 23:860–7. doi: 10.1007/s00167-014-3061-y. DOI: 10.1007/s00167-014-3061-y. PMID: 24841942.
Article38. van Dijk CN, Reilingh ML, Zengerink M, van Bergen CJ. 2010; Osteochondral defects in the ankle: why painful? Knee Surg Sports Traumatol Arthrosc. 18:570–80. doi: 10.1007/s00167-010-1064-x. DOI: 10.1007/s00167-010-1064-x. PMID: 20151110. PMCID: PMC2855020.
Article39. Mankin HJ. 1982; The response of articular cartilage to mechanical injury. J Bone Joint Surg Am. 64:460–6. DOI: 10.2106/00004623-198264030-00022. PMID: 6174527.
Article40. Radin EL, Rose RM. 1986; Role of subchondral bone in the initiation and progression of cartilage damage. Clin Orthop Relat Res. (213):34–40. DOI: 10.1097/00003086-198612000-00005. PMID: 3780104.
Article41. Shimozono Y, Coale M, Yasui Y, O'Halloran A, Deyer TW, Kennedy JG. 2018; Subchondral bone degradation after microfracture for osteochondral lesions of the talus: an MRI analysis. Am J Sports Med. 46:642–8. doi: 10.1177/0363546517739606. DOI: 10.1177/0363546517739606. PMID: 29144772.
Article42. Reilingh ML, van Bergen CJ, Blankevoort L, Gerards RM, van Eekeren IC, Kerkhoffs GM, et al. 2016; Computed tomography analysis of osteochondral defects of the talus after arthroscopic debridement and microfracture. Knee Surg Sports Traumatol Arthrosc. 24:1286–92. doi: 10.1007/s00167-015-3928-6. DOI: 10.1007/s00167-015-3928-6. PMID: 26713327. PMCID: PMC4823333.
Article43. Lee KB, Bai LB, Yoon TR, Jung ST, Seon JK. 2009; Second-look arthroscopic findings and clinical outcomes after microfracture for osteochondral lesions of the talus. Am J Sports Med. 37(Suppl 1):63S–70S. doi: 10.1177/0363546509348471. DOI: 10.1177/0363546509348471. PMID: 19843658.
Article44. Murawski CD, Duke GL, Deyer TW, Kennedy JG. 2011; Bone marrow aspirate concentrate (BMAC) as a biological adjunct to the surgical treatment of osteochondral lesions of the talus. Tech Foot Ankle Surg. 10:18–27. doi: 10.1097/BTF.0b013e31820b4c2f. DOI: 10.1097/BTF.0b013e31820b4c2f.
Article45. Fortier LA, Potter HG, Rickey EJ, Schnabel LV, Foo LF, Chong LR, et al. 2010; Concentrated bone marrow aspirate improves full-thickness cartilage repair compared with microfracture in the equine model. J Bone Joint Surg Am. 92:1927–37. doi: 10.2106/JBJS.I.01284. DOI: 10.2106/JBJS.I.01284. PMID: 20720135.
Article46. Savva N, Jabur M, Davies M, Saxby T. 2007; Osteochondral lesions of the talus: results of repeat arthroscopic debridement. Foot Ankle Int. 28:669–73. doi: 10.3113/FAI.2007.0669. DOI: 10.3113/FAI.2007.0669. PMID: 17592696.
Article47. Ogilvie-Harris DJ, Sarrosa EA. 1999; Arthroscopic treatment after previous failed open surgery for osteochondritis dissecans of the talus. Arthroscopy. 15:809–12. doi: 10.1053/ar.1999.v15.0150802. DOI: 10.1053/ar.1999.v15.0150802. PMID: 10564857.
Article48. Yoon HS, Park YJ, Lee M, Choi WJ, Lee JW. 2014; Osteochondral autologous transplantation is superior to repeat arthroscopy for the treatment of osteochondral lesions of the talus after failed primary arthroscopic treatment. Am J Sports Med. 42:1896–903. doi: 10.1177/0363546514535186. DOI: 10.1177/0363546514535186. PMID: 24907287.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Redomicrofracture as a Treatment for Osteochondral Lesion of Talus after the Failure of Arthroscopic Microfracture
- If the Patient Complains Persistent Pain after the Operation, What Should We Do?
- Autologous Osteochondral Transplantation as a Secondary Procedure after Failed Microfracture for Osteochondral Lesion of Talus
- Autologous Chondrocyte Implantation as a Secondary Procedure after Failed Microfracture for Osteochondral Lesion of Talus
- Osteochondral Lesions of the Talus