Clin Endosc.
2020 May;53(3):370-373. 10.5946/ce.2019.109.
Submucosal Tunneling Muscle Biopsy for Esophageal Motility Disorders: A Case Report
- Affiliations
-
- 1Department of Endoscopy, First Pavlov Saint-Petersburg Medical State University, Saint Petersburg, Russia
- KMID: 2502774
- DOI: http://doi.org/10.5946/ce.2019.109
Abstract
- Submucosal tunneling endoscopic technique can be useful in obtaining esophageal muscle specimens in patients with esophageal motility disorders. Here, we describe the case of a patient with systemic sclerosis. Histological verification of the esophageal involvement in the pathological process was required for the treatment. There were no intra- and post- operational complications.
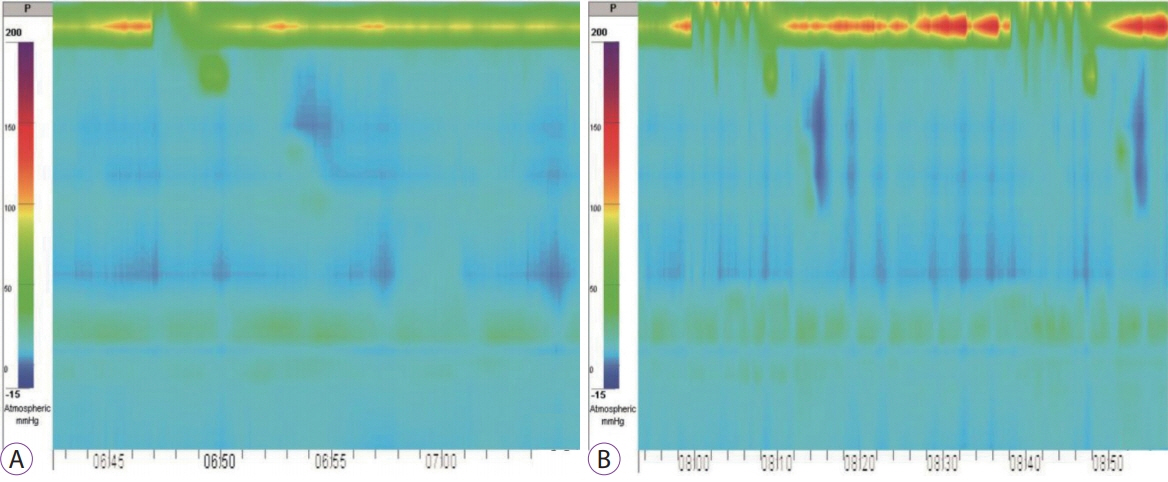
Figure
Reference
-
1. Kobara H, Mori H, Rafiq K, et al. Submucosal tunneling techniques: current perspectives. Clin Exp Gastroenterol. 2014; 7:67–74.
Article2. Knowles CH, De Giorgio R, Kapur RP, et al. Gastrointestinal neuromuscular pathology: guidelines for histological techniques and reporting on behalf of the Gastro 2009 International Working Group. Acta Neuropathol. 2009; 118:271–301.
Article3. Kahrilas PJ, Bredenoord AJ, Fox M, et al. The Chicago Classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil. 2015; 27:160–174.
Article4. Gyawali CP, Kahrilas PJ, Savarino E, et al. Modern diagnosis of GERD: the Lyon Consensus. Gut. 2018; 67:1351–1362.
Article5. Rajan E, Gostout CJ, Lurken MS, et al. Endoscopic “no hole” full-thickness biopsy of the stomach to detect myenteric ganglia. Gastrointest Endosc. 2008; 68:301–307.
Article6. Rajan E, Gostout CJ, Wong Kee Song LM, et al. Innovative gastric endoscopic muscle biopsy to identify all cell types, including myenteric neurons and interstitial cells of Cajal in patients with idiopathic gastroparesis: a feasibility study (with video). Gastrointest Endosc. 2016; 84:512–517.7. Othman MO, Davis B, Saroseik I, Torabi A, McCallum RW. EUS-guided FNA biopsy of the muscularis propria of the antrum in patients with gastroparesis is feasible and safe. Gastrointest Endosc. 2016; 83:327–333.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Esophageal Bezoar in a Patient with Achalasia: Case Report and Literature Review
- Esophageal Motility and Acid Clearance in Patients with Esophageal Varices
- Peroral Endoscopic Myotomy for Treating Achalasia and Esophageal Motility Disorders
- Three Cases of Epiphrenic Diverticula Associated With Esophageal Motility Disorders
- Assessment and Management of Primary Esophageal Motility Disorders: Achalasia and Distal Esophageal Spasm