Korean J Sports Med.
2020 Mar;38(1):20-27. 10.5763/kjsm.2020.38.1.20.
Effect of Postoperative Intensive Rehabilitation on Ankle Function Recovery in Patients with Chronic Ankle Instability
- Affiliations
-
- 1Departments of Rehabilitation Medicine, Wonkwang University School of Medicine, Iksan, Korea
- 2Departments of Orthopedic Surgery, Wonkwang University School of Medicine, Iksan, Korea
- KMID: 2502513
- DOI: http://doi.org/10.5763/kjsm.2020.38.1.20
Abstract
- Purpose
This study aimed to investigate the effect of hospital-based intensive rehabilitation program after ankle ligament operation.
Methods
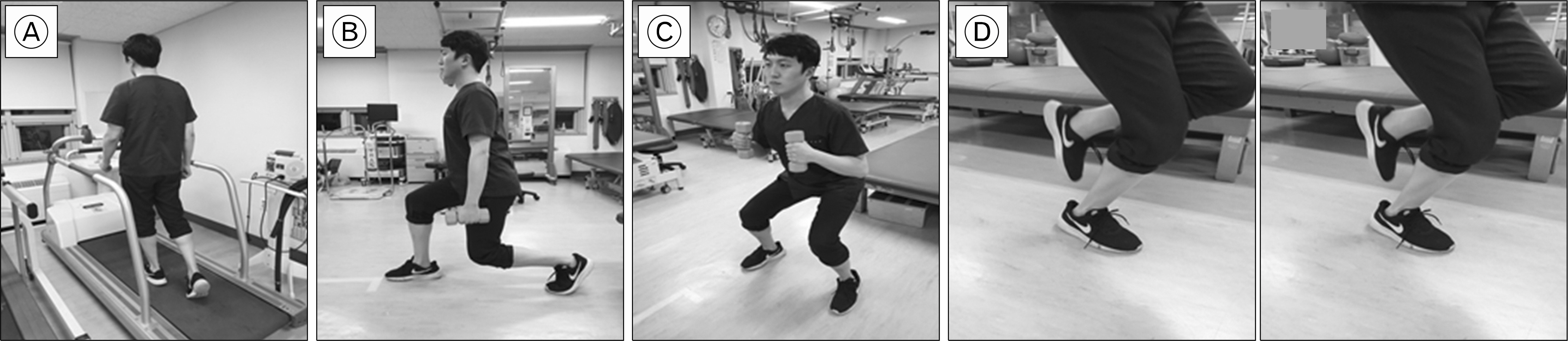
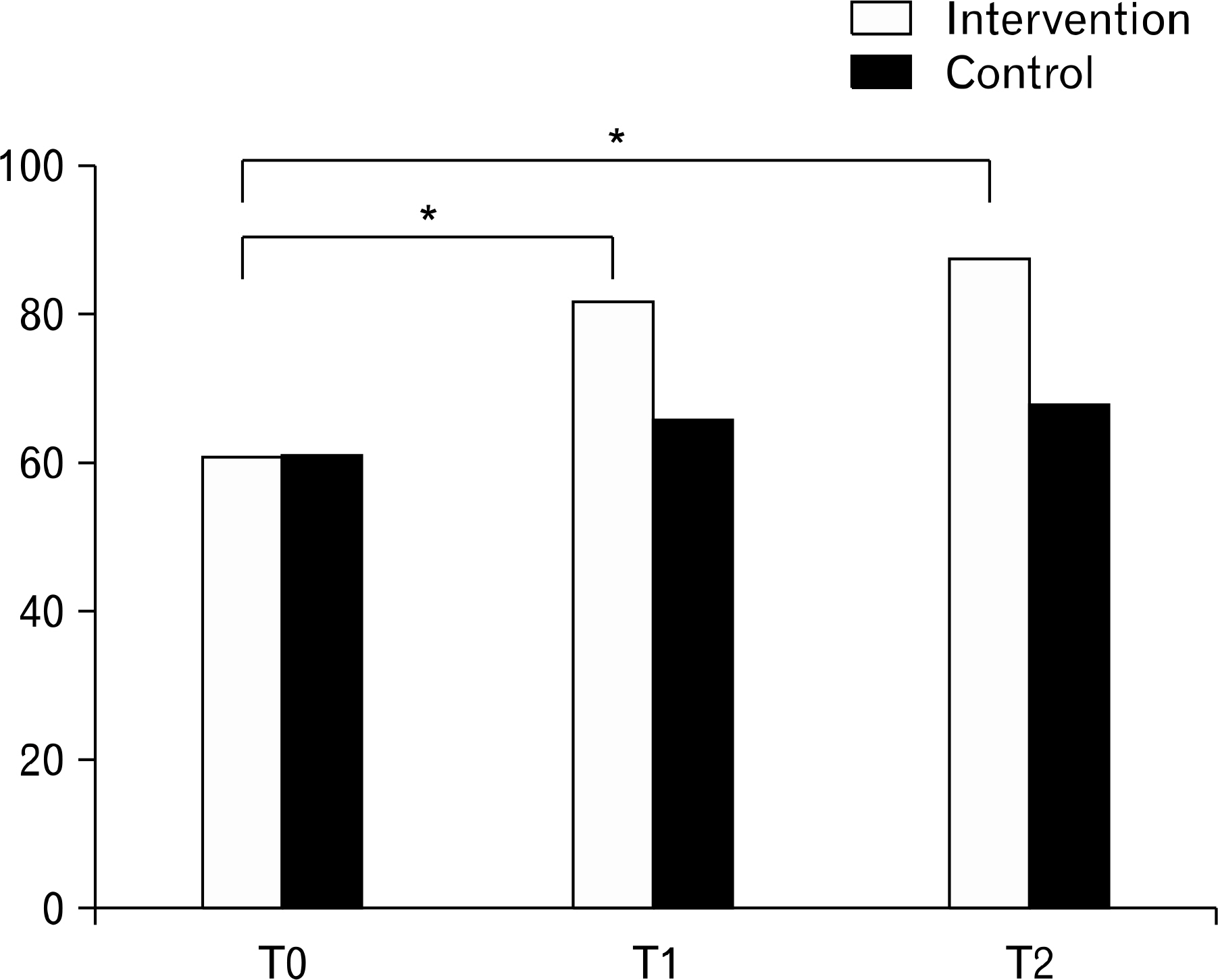
A total of 35 patients were included in this randomized controlled trial. Fifty-minute sessions of hospital-based rehabilitation were performed three times weekly for 12 weeks in the intervention group. Home-based exercise was conducted in the control group. Outcomes were evaluated at baseline, 12 weeks, and 16 weeks. The primary outcome was measured using the Foot and Ankle Outcome Score (FAOS). Secondary outcomes included the American Orthopedic Foot and Ankle Society (AOFAS) score, ankle strength measured using an isokinetic device, fall index measured using a Tetrax posturography device, and the Berg Balance Scale.
Results
Significant improvements in FAOS, AOFAS, ankle strength, and fall index were found in the intervention group after performing the hospital-based rehabilitation (all p<0.05) and these improvements were sustained at T2 (all p<0.05). Between-group comparisons demonstrated significantly greater improvements in FAOS, AOFAS, ankle strength, and fall index in the intervention group than those in the control group at both T1 (all p<0.05), and T2 (all p<0.05).
Conclusion
The rehabilitation program in this study improved postoperative pain, sports function, quality of life, and strength and balance of the ankle significantly better than home-based self-care. Therefore, we recommend hospital-based systematic rehabilitation programs after surgical treatment for chronic ankle instability.
Keyword
Figure
Reference
-
References
1. Fong DT, Hong Y, Chan LK, Yung PS, Chan KM. A systematic review on ankle injury and ankle sprain in sports. Sports Med. 2007; 37:73–94.
Article2. Anandacoomarasamy A, Barnsley L. Long term outcomes of inversion ankle injuries. Br J Sports Med. 2005; 39:e14.3. Hertel J. Functional anatomy, pathomechanics, and pathophysiology of lateral ankle instability. J Athl Train. 2002; 37:364–75.4. Kostuj T, Krummenauer F, Schaper K, et al. Analysis of agreement between the German translation of the American Foot and Ankle Society's Ankle and Hindfoot Scale (AOFAS-AHS) and the Foot Function Index in its validated German translation by Naal et al. (FFI-D). Arch Orthop Trauma Surg. 2014; 134:1205–10.
Article5. Lui TH. Modified arthroscopic Brostrom procedure. Foot Ankle Surg. 2015; 21:216–9.
Article6. Lee JH, Lee SH, Jung HW, Jang WY. Modified Brostrom procedure in patients with chronic ankle instability is superior to conservative treatment in terms of muscle endurance and postural stability. Knee Surg Sports Traumatol Arthrosc. 2020; 28:93–9.7. Guelfi M, Zamperetti M, Pantalone A, Usuelli FG, Salini V, Oliva XM. Open and arthroscopic lateral ligament repair for treatment of chronic ankle instability: a systematic review. Foot Ankle Surg. 2018; 24:11–8.
Article8. Yeo ED, Lee KT, Sung IH, Lee SG, Lee YK. Comparison of all-inside arthroscopic and open techniques for the modified broström procedure for ankle instability. Foot Ankle Int. 2016; 37:1037–45.
Article9. Sammarco VJ. Complications of lateral ankle ligament reconstruction. Clin Orthop Relat Res. 2001; 391:123–32.
Article10. Hennrikus WL, Mapes RC, Lyons PM, Lapoint JM. Outcomes of the Chrisman-Snook and modified-Broström procedures for chronic lateral ankle instability: a prospective, randomized comparison. Am J Sports Med. 1996; 24:400–4.11. Pearce CJ, Tourne Y, Zellers J, et al. Rehabilitation after anatomical ankle ligament repair or reconstruction. Knee Surg Sports Traumatol Arthrosc. 2016; 24:1130–9.
Article12. Karlsson J, Lundin O, Lind K, Styf J. Early mobilization versus immobilization after ankle ligament stabilization. Scand J Med Sci Sports. 1999; 9:299–303.
Article13. Hall EA, Docherty CL, Simon J, Kingma JJ, Klossner JC. Strength-training protocols to improve deficits in participants with chronic ankle instability: a randomized controlled trial. J Athl Train. 2015; 50:36–44.
Article14. Postle K, Pak D, Smith TO. Effectiveness of proprioceptive exercises for ankle ligament injury in adults: a systematic literature and metaanalysis. Man Ther. 2012; 17:285–91.
Article15. Mettler A, Chinn L, Saliba SA, McKeon PO, Hertel J. Balance training and center-of-pressure location in participants with chronic ankle instability. J Athl Train. 2015; 50:343–9.
Article16. Tourne Y, Mabit C. Lateral ligament reconstruction procedures for the ankle. Orthop Traumatol Surg Res. 2017; 103:S171–81.17. Cao Y, Xu Y, Hong Y, Xu X. A new minimally invasive method for anatomic reconstruction of the lateral ankle ligaments with a Tightrope system. Arch Orthop Trauma Surg. 2018; 138:1549–55.
Article18. Cordier G, Ovigue J, Dalmau-Pastor M, Michels F. Endoscopic anatomic ligament reconstruction is a reliable option to treat chronic lateral ankle instability. Knee Surg Sports Traumatol Arthrosc. 2020; 28:86–92.
Article19. van den Akker-Scheek I, Seldentuis A, Reininga IH, Stevens M. Reliability and validity of the Dutch version of the Foot and Ankle Outcome Score (FAOS). BMC Musculoskelet Disord. 2013; 14:183.
Article20. Mani SB, Brown HC, Nair P, et al. Validation of the Foot and Ankle Outcome Score in adult acquired flatfoot deformity. Foot Ankle Int. 2013; 34:1140–6.
Article21. Roos EM, Brandsson S, Karlsson J. Validation of the foot and ankle outcome score for ankle ligament reconstruction. Foot Ankle Int. 2001; 22:788–94.
Article22. Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994; 15:349–53.
Article23. Linens SW, Ross SE, Arnold BL. Wobble board rehabilitation for improving balance in ankles with chronic instability. Clin J Sport Med. 2016; 26:76–82.
Article24. Kaminski TW, Buckley BD, Powers ME, Hubbard TJ, Ortiz C. Effect of strength and proprioception training on eversion to inversion strength ratios in subjects with unilateral functional ankle instability. Br J Sports Med. 2003; 37:410–5.25. Park SJ, Hwang JH, Lee YT, Lim SG. The effect of hospital based rehabilitation exercise and home rehabilitation exercise in patients with chronic ankle sprain. Korean J Sports Med. 2006; 24:194–9.26. Konradsen L, Olesen S, Hansen HM. Ankle sensorimotor control and eversion strength after acute ankle inversion injuries. Am J Sports Med. 1998; 26:72–7.
Article27. Mattacola CG, Dwyer MK. Rehabilitation of the ankle after acute sprain or chronic instability. J Athl Train. 2002; 37:413–29.28. Bernier JN, Perrin DH. Effect of coordination training on proprioception of the functionally unstable ankle. J Orthop Sports Phys Ther. 1998; 27:264–75.
Article29. Thacker SB, Stroup DF, Branche CM, Gilchrist J, Goodman RA, Weitman EA. The prevention of ankle sprains in sports. A systematic review of the literature. Am J Sports Med. 1999; 27:753–60.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Conservative Management and Postoperative Rehabilitation of Chronic Lateral Ankle Instability
- Diagnosis and Comorbidity of Chronic Ankle Instability
- Chronic Lateral Ankle Instability
- Ligament Repair in Chronic Lateral Ankle Instability: Efficacy and Technique of Broström Procedures
- Diagnosis of Lateral Ankle Ligament Injury in the Evaluation of Chronic Lateral Ankle Instability