Diabetes Metab J.
2020 Apr;44(2):316-325. 10.4093/dmj.2019.0029.
Body Fat Is Related to Sedentary Behavior and Light Physical Activity but Not to Moderate-Vigorous Physical Activity in Type 2 Diabetes Mellitus
- Affiliations
-
- 1Department of Sports Science, Daejin University, Pocheon, Korea
- 2Department of Internal Medicine, Eulji University School of Medicine, Daejeon, Korea
- 3Department of Internal Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 4Department of Endocrinology of Metabolism, Gachon University College of Medicine, Incheon, Korea
- 5Department of Endocrinology and Metabolism, Ajou University School of Medicine, Suwon, Korea
- 6Division of Endocrinology and Metabolism, Department of Internal Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea
- KMID: 2502413
- DOI: http://doi.org/10.4093/dmj.2019.0029
Abstract
- Background
Sedentary behavior (SB) has emerged as a new risk factor for cardiovascular accidents. We investigated whether physical activity levels or SB were related to percent body fat (%BF) in type 2 diabetes mellitus (T2DM).
Methods
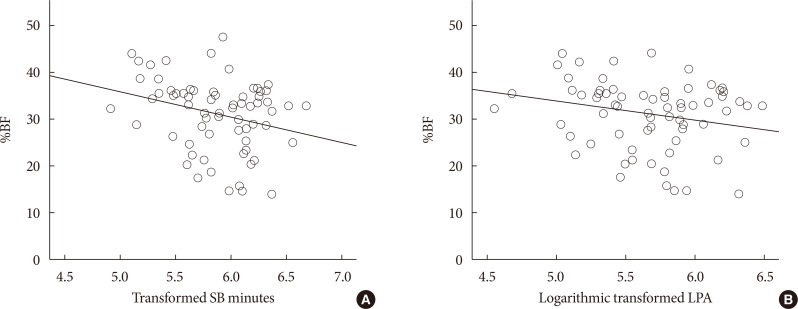
In this cross sectional study, we measured the duration of SB, light physical activity (LPA), moderate to vigorous physical activity (MVPA), total energy expenditure, and step counts using a wireless activity tracker (Fitbit HR; FB) for 7 days in freeliving conditions, along with %BF using a bio impedance analyzer (Inbody; Biospace) in 120 smartphone users with T2DM. Subjects were divided into exercise (Exe, n=68) and non-exercise (nonExe, n=52) groups based on self-reports of whether the recommended exercises (30 min/day, 3 days/week for 3 months) were performed. SBt, LPAt, MVPAt were transformed from SB, LPA, MVPA for normally distributed variables.
Results
Participants were: female, 59.2%; age, 59.3±8.4 years; body mass index, 25.5±3.4 kg/m2; glycosylated hemoglobin (HbA1c), 7.6%±1.2%; %BF, 30.4%±7.1%. They performed SB for 15.7±3.7 hr/day, LPA for 4.4±1.7 hr/day, and MVPA for 0.9±0.8 hr/day. The %BF was related to SBt and LPAt, but not to MVPA after adjustments for age, gender, and HbA1c. VPA was significantly higher in the Exe group than in the nonExe group, but SB, LPA, and moderate physical activity were not different. Predicted %BF was 89.494 to 0.105 (age), –13.047 (gender), –0.507 (HbA1c), –7.655 (LPAt) (F[4, 64]=62.929, P<0.001), with an R2 of 0.785 in multiple linear regression analysis.
Conclusion
Reduced body fat in elderly diabetic patients might be associated with reduced inactivity and increased LPA.
Figure
Reference
-
1. Stamatakis E, Hirani V, Rennie K. Moderate-to-vigorous physical activity and sedentary behaviours in relation to body mass index-defined and waist circumference-defined obesity. Br J Nutr. 2009; 101:765–773. PMID: 18680630.
Article2. Zurlo F, Lillioja S, Esposito-Del Puente A, Nyomba BL, Raz I, Saad MF, Swinburn BA, Knowler WC, Bogardus C, Ravussin E. Low ratio of fat to carbohydrate oxidation as predictor of weight gain: study of 24-h RQ. Am J Physiol. 1990; 259:E650–E657. PMID: 2240203.
Article3. Robinson SL, Hattersley J, Frost GS, Chambers ES, Wallis GA. Maximal fat oxidation during exercise is positively associated with 24-hour fat oxidation and insulin sensitivity in young, healthy men. J Appl Physiol (1985). 2015; 118:1415–1422. PMID: 25814634.
Article4. Irving BA, Davis CK, Brock DW, Weltman JY, Swift D, Barrett EJ, Gaesser GA, Weltman A. Effect of exercise training intensity on abdominal visceral fat and body composition. Med Sci Sports Exerc. 2008; 40:1863–1872. PMID: 18845966.
Article5. Colberg SR, Albright AL, Blissmer BJ, Braun B, Chasan-Taber L, Fernhall B, Regensteiner JG, Rubin RR, Sigal RJ. American College of Sports Medicine. American Diabetes Association. Exercise and type 2 diabetes: American College of Sports Medicine and the American Diabetes Association: joint position statement. Exercise and type 2 diabetes. Med Sci Sports Exerc. 2010; 42:2282–2303. PMID: 21084931.6. Romijn JA, Coyle EF, Sidossis LS, Gastaldelli A, Horowitz JF, Endert E, Wolfe RR. Regulation of endogenous fat and carbohydrate metabolism in relation to exercise intensity and duration. Am J Physiol. 1993; 265:E380–E391. PMID: 8214047.
Article7. Young DR, Hivert MF, Alhassan S, Camhi SM, Ferguson JF, Katzmarzyk PT, Lewis CE, Owen N, Perry CK, Siddique J, Yong CM. Physical Activity Committee of the Council on Lifestyle and Cardiometabolic Health. Council on Clinical Cardiology; Council on Epidemiology and Prevention. Council on Functional Genomics and Translational Biology. Stroke Council. Sedentary behavior and cardiovascular morbidity and mortality: a science advisory from the American Heart Association. Circulation. 2016; 134:e262–e279. PMID: 27528691.
Article8. Sedentary Behaviour Research Network. Letter to the editor: standardized use of the terms “sedentary” and “sedentary behaviours”. Appl Physiol Nutr Metab. 2012; 37:540–542. PMID: 22540258.9. American Diabetes Association. 4. Lifestyle management. Diabetes Care. 2017; 40:S33–S43. PMID: 27979891.10. Balducci S, D'Errico V, Haxhi J, Sacchetti M, Orlando G, Cardelli P, Di Biase N, Bollanti L, Conti F, Zanuso S, Nicolucci A, Pugliese G. Italian Diabetes and Exercise Study 2 (IDES_2) Investigators. Level and correlates of physical activity and sedentary behavior in patients with type 2 diabetes: a cross-sectional analysis of the Italian Diabetes and Exercise Study 2. PLoS One. 2017; 12:e0173337. PMID: 28291838.11. Brazeau AS, Hajna S, Joseph L, Dasgupta K. Correlates of sitting time in adults with type 2 diabetes. BMC Public Health. 2015; 15:793. PMID: 26285581.
Article12. Hamasaki H, Noda M, Moriyama S, Yoshikawa R, Katsuyama H, Sako A, Mishima S, Kakei M, Ezaki O, Yanai H. Daily physical activity assessed by a triaxial accelerometer is beneficially associated with waist circumference, serum triglycerides, and insulin resistance in Japanese patients with prediabetes or untreated early type 2 diabetes. J Diabetes Res. 2015; 2015:526201. PMID: 26064983.
Article13. Sardinha LB, Magalhaes JP, Santos DA, Judice PB. Sedentary patterns, physical activity, and cardiorespiratory fitness in association to glycemic control in type 2 diabetes patients. Front Physiol. 2017; 8:262. PMID: 28503154.
Article14. Healy GN, Winkler EA, Brakenridge CL, Reeves MM, Eakin EG. Accelerometer-derived sedentary and physical activity time in overweight/obese adults with type 2 diabetes: cross-sectional associations with cardiometabolic biomarkers. PLoS One. 2015; 10:e0119140. PMID: 25775249.
Article15. Cooper AR, Sebire S, Montgomery AA, Peters TJ, Sharp DJ, Jackson N, Fitzsimons K, Dayan CM, Andrews RC. Sedentary time, breaks in sedentary time and metabolic variables in people with newly diagnosed type 2 diabetes. Diabetologia. 2012; 55:589–599. PMID: 22167127.
Article16. Garcia-Pastor T, Salinero JJ, Sanz-Frias D, Pertusa G, Del Coso J. Body fat percentage is more associated with low physical fitness than with sedentarism and diet in male and female adolescents. Physiol Behav. 2016; 165:166–172. PMID: 27474415.
Article17. Shephard RJ. Limits to the measurement of habitual physical activity by questionnaires. Br J Sports Med. 2003; 37:197–206. PMID: 12782543.18. Bann D, Hire D, Manini T, Cooper R, Botoseneanu A, McDermott MM, Pahor M, Glynn NW, Fielding R, King AC, Church T, Ambrosius WT, Gill TM. LIFE Study Group. Light intensity physical activity and sedentary behavior in relation to body mass index and grip strength in older adults: cross-sectional findings from the Lifestyle Interventions and Independence for Elders (LIFE) study. PLoS One. 2015; 10:e0116058. PMID: 25647685.
Article19. Paul SS, Tiedemann A, Hassett LM, Ramsay E, Kirkham C, Chagpar S, Sherrington C. Validity of the Fitbit activity tracker for measuring steps in community-dwelling older adults. BMJ Open Sport Exerc Med. 2015; 1:e000013.20. Wang H, Hai S, Cao L, Zhou J, Liu P, Dong BR. Estimation of prevalence of sarcopenia by using a new bioelectrical impedance analysis in Chinese community-dwelling elderly people. BMC Geriatr. 2016; 16:216. PMID: 28031025.
Article21. Kim H, Kim CH, Kim DW, Park M, Park HS, Min SS, Han SH, Yee JY, Chung S, Kim C. External cross-validation of bioelectrical impedance analysis for the assessment of body composition in Korean adults. Nutr Res Pract. 2011; 5:246–252. PMID: 21779529.
Article22. Chowdhury EA, Western MJ, Nightingale TE, Peacock OJ, Thompson D. Assessment of laboratory and daily energy expenditure estimates from consumer multi-sensor physical activity monitors. PLoS One. 2017; 12:e0171720. PMID: 28234979.
Article23. Sasaki JE, Hickey A, Mavilia M, Tedesco J, John D, Kozey Keadle S, Freedson PS. Validation of the Fitbit wireless activity tracker for prediction of energy expenditure. J Phys Act Health. 2015; 12:149–154. PMID: 24770438.
Article24. Byun W, Lee JM, Kim Y, Brusseau TA. Classification accuracy of a wearable activity tracker for assessing sedentary behavior and physical activity in 3-5-year-old children. Int J Environ Res Public Health. 2018; 15.
Article25. Collings PJ, Westgate K, Vaisto J, Wijndaele K, Atkin AJ, Haapala EA, Lintu N, Laitinen T, Ekelund U, Brage S, Lakka TA. Cross-sectional associations of objectively-measured physical activity and sedentary time with body composition and cardiorespiratory fitness in mid-childhood: the PANIC Study. Sports Med. 2017; 47:769–780. PMID: 27558140.
Article26. Guo VY, Brage S, Ekelund U, Griffin SJ, Simmons RK. ADDITION-Plus study team. Objectively measured sedentary time, physical activity and kidney function in people with recently diagnosed type 2 diabetes: a prospective cohort analysis. Diabet Med. 2016; 33:1222–1229. PMID: 26282583.27. Bakrania K, Edwardson CL, Khunti K, Henson J, Stamatakis E, Hamer M, Davies MJ, Yates T. Associations of objectively measured moderate-to-vigorous-intensity physical activity and sedentary time with all-cause mortality in a population of adults at high risk of type 2 diabetes mellitus. Prev Med Rep. 2017; 5:285–288. PMID: 28149710.
Article28. van der Berg JD, Stehouwer CD, Bosma H, van der Velde JH, Willems PJ, Savelberg HH, Schram MT, Sep SJ, van der Kallen CJ, Henry RM, Dagnelie PC, Schaper NC, Koster A. Associations of total amount and patterns of sedentary behaviour with type 2 diabetes and the metabolic syndrome: The Maastricht Study. Diabetologia. 2016; 59:709–718. PMID: 26831300.
Article29. Matthews CE, Chen KY, Freedson PS, Buchowski MS, Beech BM, Pate RR, Troiano RP. Amount of time spent in sedentary behaviors in the United States, 2003–2004. Am J Epidemiol. 2008; 167:875–881. PMID: 18303006.
Article30. Hu FB, Li TY, Colditz GA, Willett WC, Manson JE. Television watching and other sedentary behaviors in relation to risk of obesity and type 2 diabetes mellitus in women. JAMA. 2003; 289:1785–1791. PMID: 12684356.
Article31. Agiovlasitis S, Riebe D, Ehrman JK, Liguori G, Magal M. American College of Sports Medicine, Wolters Kluwer Health. ACSM's guidelines for exercise testing and prescription. 10th ed. Philadelphia: Lippincott Williams & Wilkins;2018. p. 3.32. Hansen AL, Carstensen B, Helge JW, Johansen NB, Gram B, Christiansen JS, Brage S, Lauritzen T, Jorgensen ME, Aadahl M, Witte DR. ADDITION-Denmark Steering Committee. Combined heart rate- and accelerometer-assessed physical activity energy expenditure and associations with glucose homeostasis markers in a population at high risk of developing diabetes: the ADDITION-PRO study. Diabetes Care. 2013; 36:3062–3069. PMID: 23757430.
Article33. Hagstromer M, Oja P, Sjostrom M. Physical activity and inactivity in an adult population assessed by accelerometry. Med Sci Sports Exerc. 2007; 39:1502–1508. PMID: 17805081.34. Gusmer RJ, Bosch TA, Watkins AN, Ostrem JD, Dengel DR. Comparison of FitBit ultra to ActiGraph GT1M for assessment of physical activity in young adults during treadmill walking. Open Sports Med J. 2014; 8:11–15.
Article35. Harrington DM, Edwardson CL, Henson J, Khunti K, Yates T, Davies MJ. Moderate to vigorous physical activity, not sedentary time, is associated with total and regional adiposity in a sample of UK adults at risk of type 2 diabetes. Physiol Meas. 2016; 37:1862–1871. PMID: 27654326.
Article36. Dronkers JJ, Lamberts H, Reutelingsperger IM, Naber RH, Dronkers-Landman CM, Veldman A, van Meeteren NL. Preoperative therapeutic programme for elderly patients scheduled for elective abdominal oncological surgery: a randomized controlled pilot study. Clin Rehabil. 2010; 24:614–622. PMID: 20530651.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Physical Activity and Sedentary Behavior Patterns according to Body Composition Phenotypes of Sarcopenia and Obesity in Frail Older Women
- Association of Physical Activity and Sedentary Behavior With the Risk of Colorectal Cancer
- Amounts of physical activity and sedentary behavior patterns in older adults: using an accelerometer and a physical activity diary
- Current Status of Physical Activity in South Korea
- The Prevention of Type 2 Diabetes Mellitus