Ann Surg Treat Res.
2020 Jun;98(6):283-290. 10.4174/astr.2020.98.6.283.
Omission of axillary lymph node dissection in patients who underwent total mastectomy with 1 or 2 metastatic lymph nodes
- Affiliations
-
- 1Department of Surgery, Daejeon St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 2Department of Surgery, Yonsei University College of Medicine, Seoul, Korea
- 3Department of Surgery, Inha University Hospital, Inha University School of Medicine, Incheon, Korea
- 4Department of Surgery, Seoul National University College of Medicine, Seoul, Korea
- 5Department of Surgery, Chonnam National University Hwasun Hospital, Hwasun, Korea
- 6Department of Surgery, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- 7Breast-Thyroid Center, Saegyaero Hospital, Busan, Korea
- KMID: 2502113
- DOI: http://doi.org/10.4174/astr.2020.98.6.283
Abstract
- Purpose
Sentinel lymph node biopsy (SLNB) is the standard axillary procedure in early breast cancer patients. In a randomized trial, the survival rates were not different when axillary lymph node dissection (ALND) was omitted in patients with 1 or 2 lymph node metastases who underwent breast conserving surgery. This study aimed to compare the outcomes in patients who underwent total mastectomy (TM) with 1 or 2 metastatic nodes according to the types of axillary surgery.
Methods
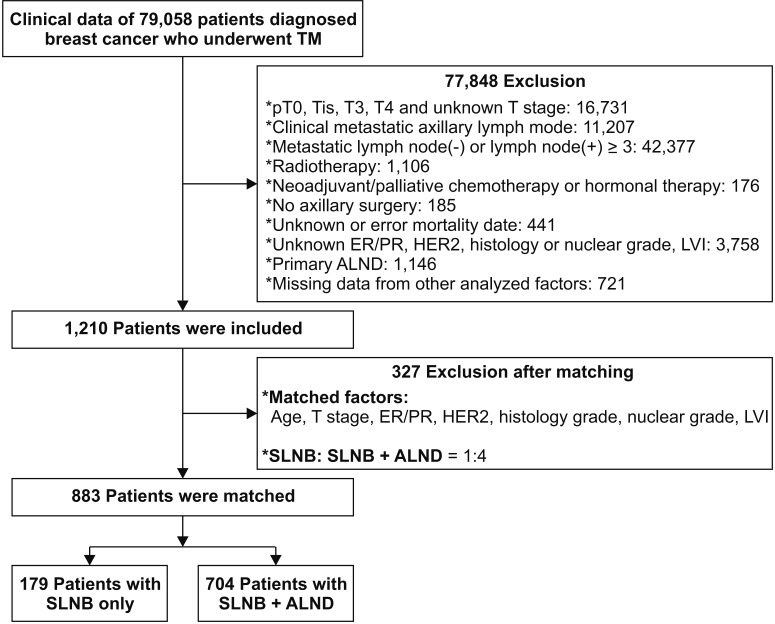
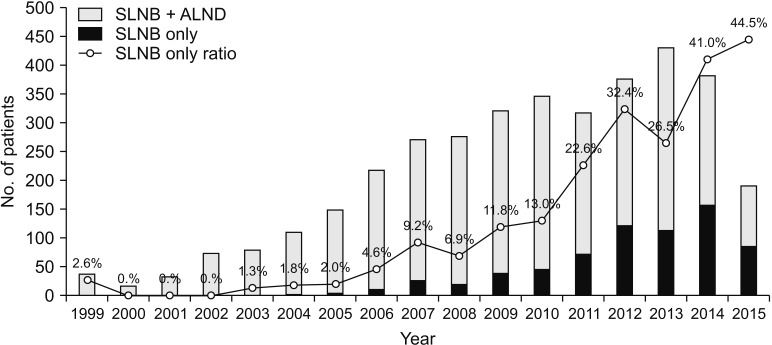
In total, 79,058 patients registered in the Korean Breast Cancer Society database who underwent TM were included in the analysis. The inclusion criteria were history of TM and SLNB, pathologic T stage 1 or 2, clinically negative axillary lymph nodes, 1 or 2 metastatic axillary lymph nodes, no radiation therapy, and no neoadjuvant therapy. We divided the patients into the SLNB only and SLNB + ALND groups. The groups were matched by propensity scores. We retrospectively analyzed the differences in the overall survival (OS) between the 2 groups.
Results
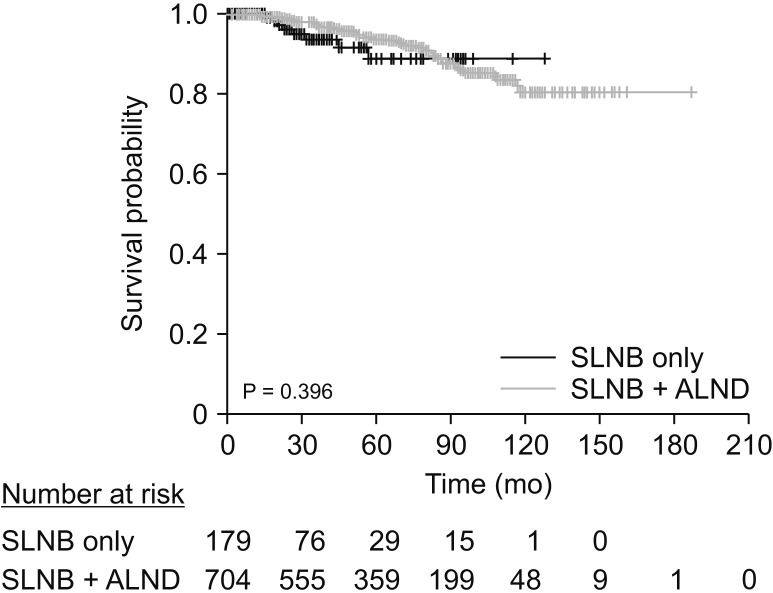
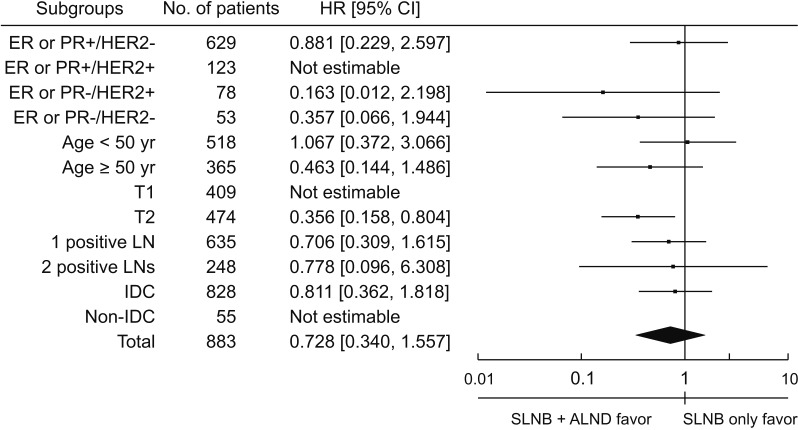
A total of 883 patients were matched in a 1:4 ratio for the SLNB only and SLNB + ALND groups in the cohort from 1999 to 2014. There were no significant differences in OS between the 2 groups (P = 0.413). Subgroup analysis revealed a significant survival benefit in the SLNB + ALND group in the T2 subgroup (P = 0.013).
Conclusion
OS did not differ between the 2 groups in early breast cancer patients with 1 or 2 metastatic axillary lymph nodes who underwent TM. Omission of ALND may be considered in selected patients.
Figure
Reference
-
1. Halsted WS. I. A clinical and histological study of certain adenocarcinomata of the breast: and a brief consideration of the supraclavicular operation and of the results of operations for cancer of the breast from 1889 to 1898 at the Johns Hopkins Hospital. Ann Surg. 1898; 28:557–576.2. Halsted WS. I. The results of radical operations for the cure of carcinoma of the breast. Ann Surg. 1907; 46:1–19.3. Khan F, Amatya B, Pallant JF, Rajapaksa I. Factors associated with long-term functional outcomes and psychological sequelae in women after breast cancer. Breast. 2012; 21:314–320. PMID: 22342676.4. Armer JM. The problem of post-breast cancer lymphedema: impact and measurement issues. Cancer Invest. 2005; 23:76–83. PMID: 15779870.5. Bulley C, Coutts F, Blyth C, Jack W, Chetty U, Barber M, et al. A Morbidity Screening Tool for identifying fatigue, pain, upper limb dysfunction and lymphedema after breast cancer treatment: a validity study. Eur J Oncol Nurs. 2014; 18:218–227. PMID: 24246445.6. Krag DN, Anderson SJ, Julian TB, Brown AM, Harlow SP, Costantino JP, et al. Sentinel-lymph-node resection compared with conventional axillary-lymph-node dissection in clinically node-negative patients with breast cancer: overall survival findings from the NSABP B-32 randomised phase 3 trial. Lancet Oncol. 2010; 11:927–933. PMID: 20863759.7. Galimberti V, Cole BF, Zurrida S, Viale G, Luini A, Veronesi P, et al. Axillary dissection versus no axillary dissection in patients with sentinel-node micrometastases (IBCSG 23-01): a phase 3 randomised controlled trial. Lancet Oncol. 2013; 14:297–305. PMID: 23491275.8. Sola M, Alberro JA, Fraile M, Santesteban P, Ramos M, Fabregas R, et al. Complete axillary lymph node dissection versus clinical follow-up in breast cancer patients with sentinel node micrometastasis: final results from the multicenter clinical trial AATRM 048/13/2000. Ann Surg Oncol. 2013; 20:120–127. PMID: 22956062.9. Giuliano AE, Hunt KK, Ballman KV, Beitsch PD, Whitworth PW, Blumencranz PW, et al. Axillary dissection vs no axillary dissection in women with invasive breast cancer and sentinel node metastasis: a randomized clinical trial. JAMA. 2011; 305:569–575. PMID: 21304082.10. Bleyer A, Welch HG. Effect of three decades of screening mammography on breast-cancer incidence. N Engl J Med. 2012; 367:1998–2005. PMID: 23171096.11. Iqbal J, Ginsburg O, Rochon PA, Sun P, Narod SA. Differences in breast cancer stage at diagnosis and cancer-specific survival by race and ethnicity in the United States. JAMA. 2015; 313:165–173. PMID: 25585328.12. Kang SY, Kim YS, Kim Z, Kim HY, Lee SK, Jung KW, et al. Basic findings regarding breast cancer in Korea in 2015: data from a Breast Cancer Registry. J Breast Cancer. 2018; 21:1–10. PMID: 29628978.13. Miller BT, Abbott AM, Tuttle TM. The influence of preoperative MRI on breast cancer treatment. Ann Surg Oncol. 2012; 19:536–540. PMID: 21751044.14. Hong KY, Son Y, Chang H, Jin US. Trends in breast reconstruction: implications for the National Health Insurance Service. Arch Plast Surg. 2018; 45:239–245. PMID: 29788687.15. Belkacemi Y, Allab-Pan Q, Bigorie V, Khodari W, Beaussart P, Totobenazara JL, et al. The standard tangential fields used for breast irradiation do not allow optimal coverage and dose distribution in axillary levels I-II and the sentinel node area. Ann Oncol. 2013; 24:2023–2028. PMID: 23616280.16. Giuliano AE, Ballman K, McCall L, Beitsch P, Whitworth PW, Blumencranz P, et al. Locoregional recurrence after sentinel lymph node dissection with or without axillary dissection in patients with sentinel lymph node metastases: long-term follow-up from the American College of Surgeons Oncology Group (Alliance) ACOSOG Z0011 Randomized Trial. Ann Surg. 2016; 264:413–420. PMID: 27513155.17. Lee J, Choi JE, Kim SJ, Lee SB, Seong MK, Jeong J, et al. Comparative study between sentinel lymph node biopsy and axillary dissection in patients with one or two lymph node metastases. J Breast Cancer. 2018; 21:306–314. PMID: 30275859.18. FitzSullivan E, Bassett RL, Kuerer HM, Mittendorf EA, Yi M, Hunt KK, et al. Outcomes of sentinel lymph node-positive breast cancer patients treated with mastectomy without axillary therapy. Ann Surg Oncol. 2017; 24:652–659.19. Van Zee KJ, Manasseh DM, Bevilacqua JL, Boolbol SK, Fey JV, Tan LK, et al. A nomogram for predicting the likelihood of additional nodal metastases in breast cancer patients with a positive sentinel node biopsy. Ann Surg Oncol. 2003; 10:1140–1151. PMID: 14654469.20. Park J, Fey JV, Naik AM, Borgen PI, Van Zee KJ, Cody HS 3rd. A declining rate of completion axillary dissection in sentinel lymph node-positive breast cancer patients is associated with the use of a multivariate nomogram. Ann Surg. 2007; 245:462–468. PMID: 17435554.21. Giuliano AE, Ballman KV, McCall L, Beitsch PD, Brennan MB, Kelemen PR, et al. Effect of axillary dissection vs no axillary dissection on 10-year overall survival among women with invasive breast cancer and sentinel node metastasis: the ACOSOG Z0011 (Alliance) Randomized Clinical Trial. JAMA. 2017; 318:918–926. PMID: 28898379.22. Knight WA, Livingston RB, Gregory EJ, McGuire WL. Estrogen receptor as an independent prognostic factor for early recurrence in breast cancer. Cancer Res. 1977; 37:4669–4671. PMID: 922747.23. Parl FF, Schmidt BP, Dupont WD, Wagner RK. Prognostic significance of estrogen receptor status in breast cancer in relation to tumor stage, axillary node metastasis, and histopathologic grading. Cancer. 1984; 54:2237–2242. PMID: 6488142.24. Parise CA, Caggiano V. Risk of mortality of node-negative, ER/PR/HER2 breast cancer subtypes in T1, T2, and T3 tumors. Breast Cancer Res Treat. 2017; 165:743–750. PMID: 28689363.25. Kim H, Cho J, Kwon SY, Kang SH. Biologic subtype is a more important prognostic factor than nodal involvement in patients with stages I and II breast carcinoma. Ann Surg Treat Res. 2016; 90:1–9. PMID: 26793686.26. Roberts A, Nofech-Mozes S, Youngson B, McCready DR, Al-Assi M, Ramkumar S, et al. The importance of applying ACOSOG Z0011 criteria in the axillary management of invasive lobular carcinoma: a multi-institutional cohort study. Ann Surg Oncol. 2015; 22:3397–3401. PMID: 26215196.27. Wang J, Mittendorf EA, Sahin AA, Yi M, Caudle A, Hunt KK, et al. Outcomes of sentinel lymph node dissection alone vs. axillary lymph node dissection in early stage invasive lobular carcinoma: a retrospective study of the surveillance, epidemiology and end results (SEER) database. PLoS One. 2014; 9:e89778. PMID: 24587029.28. Loza CM, Mando P, Ponce C, Colo F, Fabiano V, Loza J, et al. Predictive factors for non-sentinel lymph node metastasis in patients with ACOSOG Z0011 criteria. Breast Care (Basel). 2018; 13:434–438. PMID: 30800038.29. Ozmen V, Karanlik H, Cabioglu N, Igci A, Kecer M, Asoglu O, et al. Factors predicting the sentinel and non-sentinel lymph node metastases in breast cancer. Breast Cancer Res Treat. 2006; 95:1–6. PMID: 16322900.30. Donker M, van Tienhoven G, Straver ME, Meijnen P, van de Velde CJ, Mansel RE, et al. Radiotherapy or surgery of the axilla after a positive sentinel node in breast cancer (EORTC 10981-22023 AMAROS): a randomised, multicentre, open-label, phase 3 non-inferiority trial. Lancet Oncol. 2014; 15:1303–1310. PMID: 25439688.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Significance of Rotter's Nodes in Patients with Breast Carcinomas
- Ultrasonography for Staging Axillary Lymph Node in Breast Cancer Patients
- Endoscopic Axillary Dissection in Breast Cancer
- Incidence of Axillary Lymph Node Metastases in T1 Breast Cancer
- Incidence of Axillary Lymph Node Metastases in T1 Breast Cancer