Neonatal Med.
2020 Feb;27(1):1-7. 10.5385/nm.2020.27.1.1.
Changes in the Incidence of Bronchopulmonary Dysplasia among Preterm Infants in a Single Center over 10 Years
- Affiliations
-
- 1Department of Pediatrics, Inje University Busan Paik Hospital, Inje University College of Medicine, Busan, Korea
- KMID: 2502086
- DOI: http://doi.org/10.5385/nm.2020.27.1.1
Abstract
- Purpose
Bronchopulmonary dysplasia (BPD) is one of the most fatal respiratory morbidities in preterm infants, causing adverse respiratory and neurodevelopmental outcomes. Despite advances in neonatal ventilator care, the incidence of BPD has been static or even increased. The purpose of this study was to evaluate the incidence of BPD in a single center over 10 years.
Methods
Preterm infants with gestational age (GA) <30 weeks who were admitted to Inje University Busan Paik Hospital from January 2009 to December 2018 and sur vived 28 days or more were enrolled. The incidence of BPD according to year and GA and the risk factors of BPD were evaluated.
Results
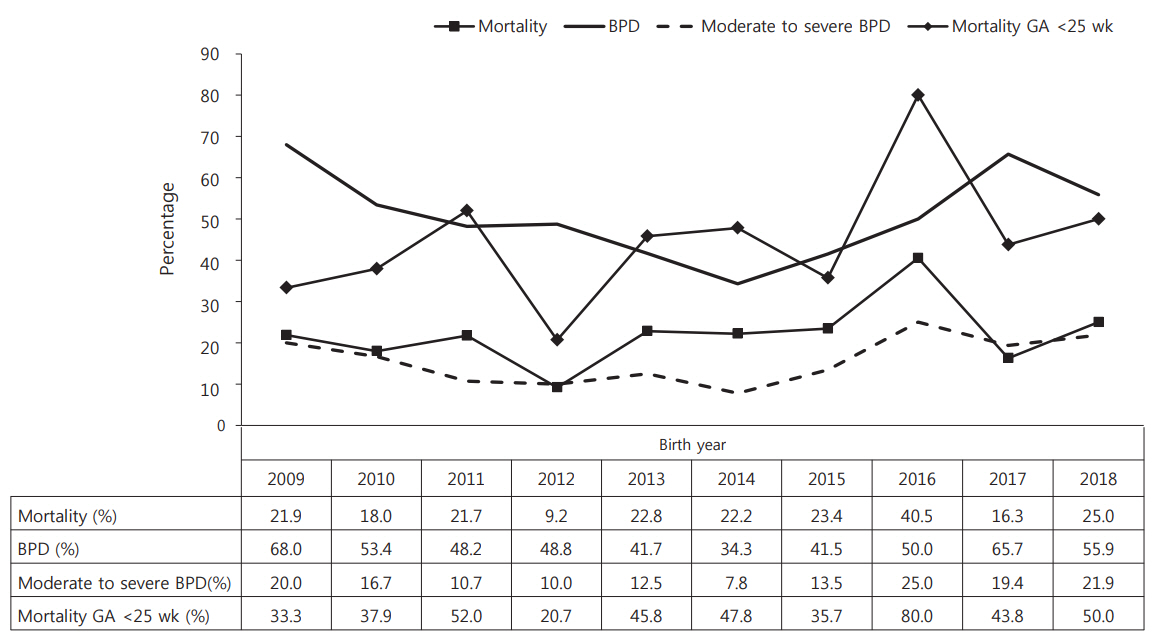
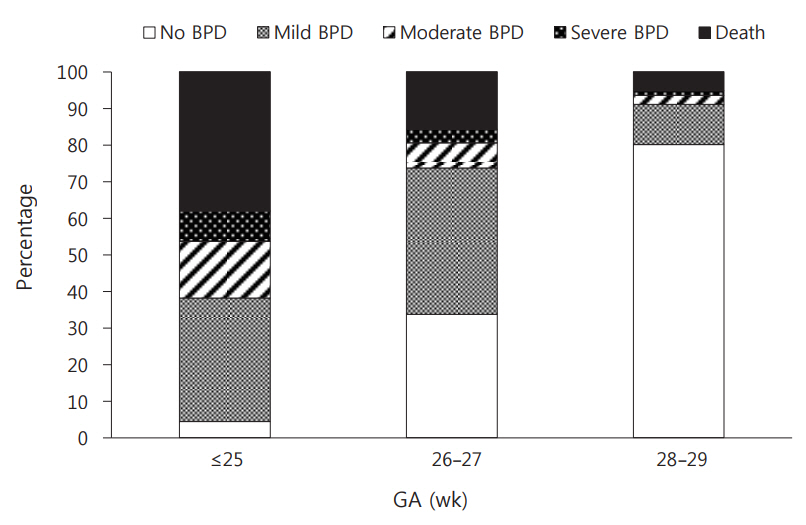
Among 629 infants, 521 infants who survived 28 days or more were enrolled (BPD group, n=252; non-BPD group, n=269). The incidence of BPD was 48.4%, with moderate to severe BPD accounting for 13.9%. In preterm infants with GA ≤25, 26 to 27, and 28 to 29 weeks, the incidences of BPD were 57.5%, 51.5%, and 14.6%, respectively, with moderate to severe BPD accounting for 23.8%, 10.5%, and 3.7%, respectively. The incidence of BPD decreased from 68% in 2009 to 34.3% in 2014. Subsequently, it increased. Surfactant re-dosing and patent ductus arteriosus were more frequent in the BPD group than in the non-BPD group.
Conclusion
BPD did not decrease over the previous 10 years despite advances in neonatal care.
Keyword
Figure
Reference
-
1. Northway WH Jr, Rosan RC, Porter DY. Pulmonary disease following respirator therapy of hyaline-membrane disease. Bronchopulmonary dysplasia. N Engl J Med. 1967; 276:357–68.2. H1ahn WH, Chang JY, Chang YS, Shim KS, Bae CW. Recent trends in neonatal mortality in very low birth weight Korean infants: in comparison with Japan and the USA. J Korean Med Sci. 2011; 26:467–73.3. Stoll BJ, Hansen NI, Bell EF, Walsh MC, Carlo WA, Shankaran S, et al. Trends in care practices, morbidity, and mortality of extremely preterm neonates, 1993-2012. JAMA. 2015; 314:1039–51.4. Baud O, Maury L, Lebail F, Ramful D, El Moussawi F, Nicaise C, et al. Effect of early low-dose hydrocortisone on survival without bronchopulmonary dysplasia in extremely preterm infants (PREMILOC): a double-blind, placebo-controlled, multicentre, randomised trial. Lancet. 2016; 387:1827–36.5. Ambalavanan N, Walsh M, Bobashev G, Das A, Levine B, Carlo WA, et al. Intercenter differences in bronchopulmonary dysplasia or death among very low birth weight infants. Pediatrics. 2011; 127:e106–16.6. Stevenson DK, Wright LL, Lemons JA, Oh W, Korones SB, Papile LA, et al. Very low birth weight outcomes of the National Institute of Child Health and Human Development Neonatal Research Network, January 1993 through December 1994. Am J Obstet Gynecol. 1998; 179(6 Pt 1):1632–9.7. Malavolti AM, Bassler D, Arlettaz-Mieth R, Faldella G, Latal B, Natalucci G. Bronchopulmonary dysplasia-impact of severity and timing of diagnosis on neurodevelopment of preterm infants: a retrospective cohort study. BMJ Paediatr Open. 2018; 2:e000165.8. Majnemer A, Riley P, Shevell M, Birnbaum R, Greenstone H, Coates AL. Severe bronchopulmonary dysplasia increases risk for later neurological and motor sequelae in preterm survivors. Dev Med Child Neurol. 2000; 42:53–60.9. Kinsella JP, Greenough A, Abman SH. Bronchopulmonary dysplasia. Lancet. 2006; 367:1421–31.10. Jobe AH, Bancalari E. Bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2001; 163:1723–9.11. Jeng SF, Hsu CH, Tsao PN, Chou HC, Lee WT, Kao HA, et al. Bronchopulmonary dysplasia predicts adverse developmental and clinical outcomes in very-low-birthweight infants. Dev Med Child Neurol. 2008; 50:51–7.12. Karagianni P, Tsakalidis C, Kyriakidou M, Mitsiakos G, Chatziioanidis H, Porpodi M, et al. Neuromotor outcomes in infants with bronchopulmonary dysplasia. Pediatr Neurol. 2011; 44:40–6.13. Synnes A, Luu TM, Moddemann D, Church P, Lee D, Vincer M, et al. Determinants of developmental outcomes in a very preterm Canadian cohort. Arch Dis Child Fetal Neonatal Ed. 2017; 102:F235–4.14. Baveja R, Christou H. Pharmacological strategies in the prevention and management of bronchopulmonary dysplasia. Semin Perinatol. 2006; 30:209–18.15. Tropea K, Christou H. Current pharmacologic approaches for prevention and treatment of bronchopulmonary dysplasia. Int J Pediatr. 2012; 2012:598606.16. Beam KS, Aliaga S, Ahlfeld SK, Cohen-Wolkowiez M, Smith PB, Laughon MM. A systematic review of randomized controlled trials for the prevention of bronchopulmonary dysplasia in infants. J Perinatol. 2014; 34:705–10.17. Jeon GW, Oh M, Sin JB. Efficacy of surfactant-TA, calfactant and poractant alfa for preterm infants with respiratory distress syndrome: a retrospective study. Yonsei Med J. 2015; 56:433–9.18. Morley CJ, Davis PG, Doyle LW, Brion LP, Hascoet JM, Carlin JB, et al. Nasal CPAP or intubation at birth for very preterm infants. N Engl J Med. 2008; 358:700–8.19. SUPPORT Study Group of the Eunice Kennedy Shriver NICHD Neonatal Research Network, Finer NN, Carlo WA, Walsh MC, Rich W, Gantz MG, et al. Early CPAP versus surfactant in extremely preterm infants. N Engl J Med. 2010; 362:1970–9.20. Stevens TP, Harrington EW, Blennow M, Soll RF. Early surfactant administration with brief ventilation vs. selective surfactant and continued mechanical ventilation for preterm infants with or at risk for respiratory distress syndrome. Cochrane Database Syst Rev. 2007; 4:CD003063.21. Kanmaz HG, Erdeve O, Canpolat FE, Mutlu B, Dilmen U. Surfactant administration via thin catheter during spontaneous breathing: randomized controlled trial. Pediatrics. 2013; 131:e502–9.22. Shennan AT, Dunn MS, Ohlsson A, Lennox K, Hoskins EM. Abnormal pulmonary outcomes in premature infants: prediction from oxygen requirement in the neonatal period. Pediatrics. 1988; 82:527–32.23. Walsh MC, Yao Q, Gettner P, Hale E, Collins M, Hensman A, et al. Impact of a physiologic definition on bronchopulmonary dysplasia rates. Pediatrics. 2004; 114:1305–11.24. Kim SH, Lee KH, Lee SH, You DK, Choi SJ, Hwang JH, et al. The comparison of severity according to preceding causes of bronchopulmonary dysplasia in very low birth weight infants. J Korean Soc Neonatol. 2003; 10:47–54.25. Choi CW, Kim BI, Kim EK, Song ES, Lee JJ. Incidence of bronchopulmonary dysplasia in Korea. J Korean Med Sci. 2012; 27:91421.26. Jo HS, Cho KH, Cho SI, Song ES, Kim BI. Recent changes in the incidence of bronchopulmonary dysplasia among very-lowbirth-weight infants in Korea. J Korean Med Sci. 2015; 30 Suppl 1:S81–7.27. Fanaroff AA, Stoll BJ, Wright LL, Carlo WA, Ehrenkranz RA, Stark AR, et al. Trends in neonatal morbidity and mortality for very low birthweight infants. Am J Obstet Gynecol. 2007; 196:147.28. Payne NR, LaCorte M, Karna P, Chen S, Finkelstein M, Goldsmith JP, et al. Reduction of bronchopulmonary dysplasia after participation in the Breathsavers Group of the Vermont Oxford Network Neonatal Intensive Care Quality Improvement Collaborative. Pediatrics. 2006; 118 Suppl 2:S73–7.29. Smith VC, Zupancic JA, McCormick MC, Croen LA, Greene J, Escobar GJ, et al. Trends in severe bronchopulmonary dysplasia rates between 1994 and 2002. J Pediatr. 2005; 146:469–73.30. Kalikkot Thekkeveedu R, Guaman MC, Shivanna B. Bronchopulmonary dysplasia: a review of pathogenesis and pathophysiology. Respir Med. 2017; 132:170–7.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prevention and Treatment of Bronchopulmonary Dysplasia
- Association of Positive Ureaplasma in Gastric Fluid with Clinical Features in Preterm Infants
- Bronchopulmonary dysplasia: how can we improve its outcomes?
- Optimal Ventilatory Strategies in Preterm Infants: Permissive Hypercapnia
- Factors Associated with Clinical Response to Low-Dose Dexamethasone Therapy for Bronchopulmonary Dysplasia in Very Low Birth Weight Infants