Cancer Res Treat.
2020 Jan;52(1):85-97. 10.4143/crt.2019.007.
SUVmax Predicts Disease Progression after Stereotactic Ablative Radiotherapy in Stage I Non-small Cell Lung Cancer
- Affiliations
-
- 1Department of Radiation Oncology, Incheon St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 2Department of Radiation Oncology, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 3Department of Radiation Oncology, Eunpyeong St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 4Department of Nuclear Medicine, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- KMID: 2501204
- DOI: http://doi.org/10.4143/crt.2019.007
Abstract
- Purpose
Fluorodeoxyglucose positron emission tomography–computed tomography (PET-CT) is gaining evidence as a predictive factor in non-small cell lung cancer (NSCLC). Stereotactic ablative radiotherapy (SABR) is the standard treatment in early-stage NSCLC when a patient is unsuitable for surgery. We performed a study to assess the prognostic clinical significance of PET-CT after SABR in early-stage NSCLC.
Materials and Methods
Seventy-six patients with stage I NSCLC treated with SABR were investigated. Total radiation dose ranged from 36 to 63 Gy in three to eight fractions depending on tumor location and size. Respiratory motion control was implemented at simulation and during treatment. PET-CT prior to SABR was performed in 66 patients (86.8%).
Results
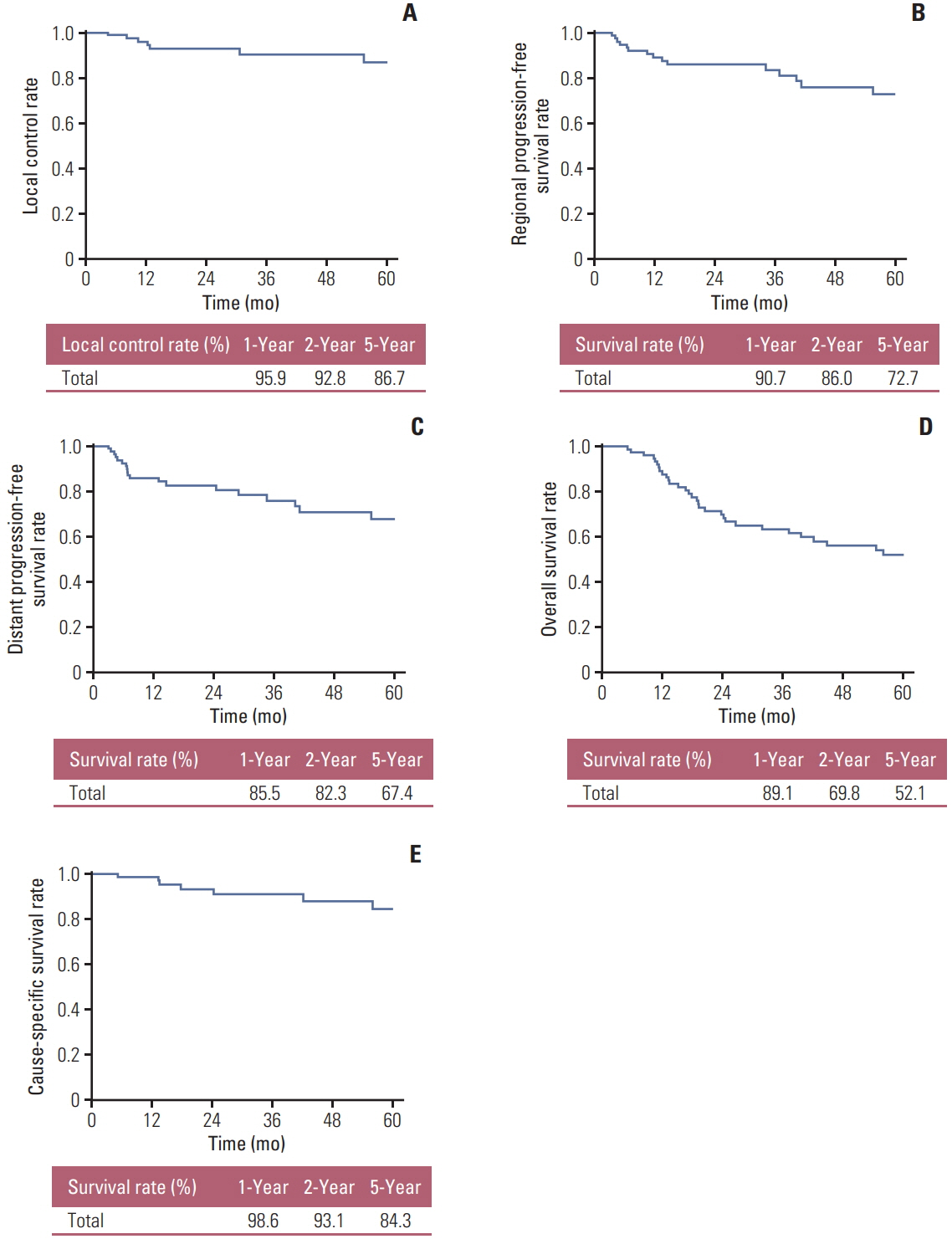
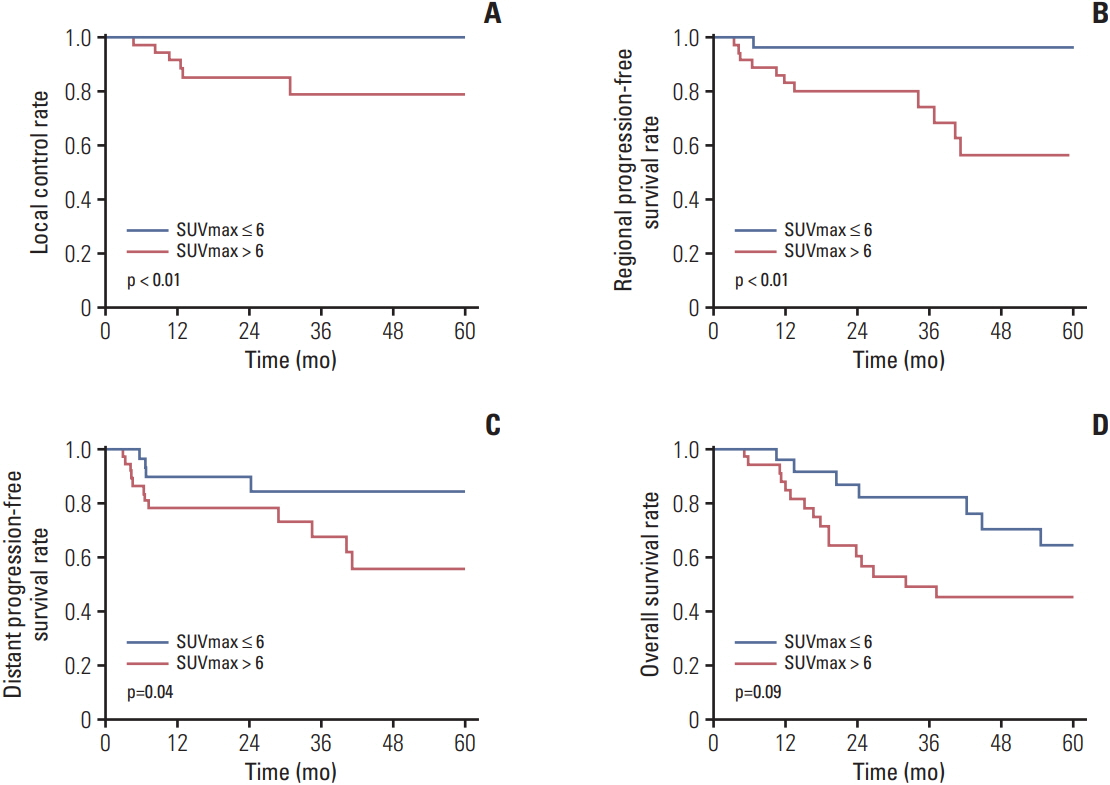
Median follow-up time was 32 months (range, 5 to 142 months). Local control rate at 1, 2, and 5 years were 95.9%, 92.8%, and 86.7%, respectively. Overall survival (OS) at 1, 2, and 5 years were 91.0%, 71.3%, and 52.1% respectively. Cause-specific survival at 1, 2, and 5 years were 98.6%, 93.1%, and 84.3% respectively. Tumor size and pre-SABR maximal standardized uptake value (SUVmax) demonstrated statistical significance in the Kaplan-Meier survival analyses with log-rank test. In multivariate analyses pre-SABR SUVmax remained statistically significant in correlation to OS (p=0.024; hazard ratio [HR], 3.2; 95% confidence interval [CI], 1.2 to 8.8) and with marginal significance in regards to regional progression-free survival (p=0.059; HR, 32.5; 95% CI, 2.6 to 402.5).
Conclusion
Pre-SABR SUVmax demonstrated a predictive power in statistical analyses. Tumors with SUVmax above 6 at diagnosis were associated with inferior outcomes.
Keyword
Figure
Reference
-
References
1. Senan S, Paul MA, Lagerwaard FJ. Treatment of early-stage lung cancer detected by screening: surgery or stereotactic ablative radiotherapy? Lancet Oncol. 2013; 14:e270.
Article2. Nguyen NP, Garland L, Welsh J, Hamilton R, Cohen D, Vinh-Hung V. Can stereotactic fractionated radiation therapy become the standard of care for early stage non-small cell lung carcinoma. Cancer Treat Rev. 2008; 34:719–27.
Article3. Huang K, Palma DA; IASLC Advanced Radiation Technology Committee. Follow-up of patients after stereotactic radiation for lung cancer: a primer for the nonradiation oncologist. J Thorac Oncol. 2015; 10:412–9.
Article4. Goldstraw P, Chansky K, Crowley J, Rami-Porta R, Asamura H, Eberhardt WE, et al. The IASLC Lung Cancer Staging Project: proposals for revision of the TNM stage groupings in the forthcoming (eighth) edition of the TNM classification for lung cancer. J Thorac Oncol. 2016; 11:39–51.5. Berghmans T, Dusart M, Paesmans M, Hossein-Foucher C, Buvat I, Castaigne C, et al. Primary tumor standardized uptake value (SUVmax) measured on fluorodeoxyglucose positron emission tomography (FDG-PET) is of prognostic value for survival in non-small cell lung cancer (NSCLC): a systematic review and meta-analysis (MA) by the European Lung Cancer Working Party for the IASLC Lung Cancer Staging Project. J Thorac Oncol. 2008; 3:6–12.
Article6. Paesmans M, Berghmans T, Dusart M, Garcia C, Hossein-Foucher C, Lafitte JJ, et al. Primary tumor standardized uptake value measured on fluorodeoxyglucose positron emission tomography is of prognostic value for survival in non-small cell lung cancer: update of a systematic review and metaanalysis by the European Lung Cancer Working Party for the International Association for the Study of Lung Cancer Staging Project. J Thorac Oncol. 2010; 5:612–9.
Article7. Goldstraw P. The 7th edition of the TNM classification for lung cancer: proposals from the IASLC staging project. Eur J Cancer Suppl. 2007; 5:15–22.
Article8. Lee DS, Kim YS, Yoo IR, Kang YN, Kim SJ, Oh JK, et al. Longterm clinical experience of high-dose ablative lung radiotherapy: high pre-treatment [18F]fluorodeoxyglucose-positron emission tomography maximal standardized uptake value of the primary tumor adversely affects treatment outcome. Lung Cancer. 2013; 80:172–8.
Article9. Graziano SL. Non-small cell lung cancer: clinical value of new biological predictors. Lung Cancer. 1997; 17 Suppl 1:S37–58.
Article10. Jeremic B, Milicic B, Dagovic A, Acimovic L, Milisavljevic S. Pretreatment prognostic factors in patients with early-stage (I/II) non-small-cell lung cancer treated with hyperfractionated radiation therapy alone. Int J Radiat Oncol Biol Phys. 2006; 65:1112–9.11. Trape J, Buxo J, Perez de Olaguer J, Vidal C. Tumor markers as prognostic factors in treated non-small cell lung cancer. Anticancer Res. 2003; 23:4277–81.12. Niklinski J, Niklinska W, Laudanski J, Chyczewska E, Chyczewski L. Prognostic molecular markers in non-small cell lung cancer. Lung Cancer. 2001; 34 Suppl 2:S53–8.
Article13. Li Q, Kim J, Balagurunathan Y, Qi J, Liu Y, Latifi K, et al. CT imaging features associated with recurrence in non-small cell lung cancer patients after stereotactic body radiotherapy. Radiat Oncol. 2017; 12:158.
Article14. Matsuo Y, Nakamoto Y, Nagata Y, Shibuya K, Takayama K, Norihisa Y, et al. Characterization of FDG-PET images after stereotactic body radiation therapy for lung cancer. Radiother Oncol. 2010; 97:200–4.
Article15. Henderson MA, Hoopes DJ, Fletcher JW, Lin PF, Tann M, Yiannoutsos CT, et al. A pilot trial of serial 18F-fluorodeoxyglucose positron emission tomography in patients with medically inoperable stage I non-small-cell lung cancer treated with hypofractionated stereotactic body radiotherapy. Int J Radiat Oncol Biol Phys. 2010; 76:789–95.
Article16. Wiegman EM, Pruim J, Ubbels JF, Groen HJ, Langendijk JA, Widder J. 18F-FDG PET during stereotactic body radiotherapy for stage I lung tumours cannot predict outcome: a pilot study. Eur J Nucl Med Mol Imaging. 2011; 38:1059–63.
Article17. Burdick MJ, Stephans KL, Reddy CA, Djemil T, Srinivas SM, Videtic GM. Maximum standardized uptake value from staging FDG-PET/CT does not predict treatment outcome for early-stage non-small-cell lung cancer treated with stereotactic body radiotherapy. Int J Radiat Oncol Biol Phys. 2010; 78:1033–9.
Article18. Miller CJ, Martin B, Stang K, Hutten R, Alite F, Small C, et al. Predictors of distant failure after stereotactic body radiation therapy for stages I to IIA non-small-cell lung cancer. Clin Lung Cancer. 2019; 20:37–42.
Article19. Sasaki R, Komaki R, Macapinlac H, Erasmus J, Allen P, Forster K, et al. [18F]fluorodeoxyglucose uptake by positron emission tomography predicts outcome of non-small-cell lung cancer. J Clin Oncol. 2005; 23:1136–43.
Article20. Zhang X, Liu H, Balter P, Allen PK, Komaki R, Pan T, et al. Positron emission tomography for assessing local failure after stereotactic body radiotherapy for non-small-cell lung cancer. Int J Radiat Oncol Biol Phys. 2012; 83:1558–65.
Article21. Park J, Choi Y, Ahn KJ, Park SK, Cho H, Lee JY. Maximum standardized uptake value at pre-treatment PET in estimating lung cancer progression after stereotactic body radiotherapy. Radiat Oncol J. 2019; 37:30–6.
Article22. Dong M, Liu J, Sun X, Xing L. Prognositc significance of SUVmax on pretreatment (18) F-FDG PET/CT in early-stage nonsmall cell lung cancer treated with stereotactic body radiotherapy: A meta-analysis. J Med Imaging Radiat Oncol. 2017; 61:652–9.23. Yamamoto T, Kadoya N, Shirata Y, Kaneta T, Koto M, Umezawa R, et al. Formula corrected maximal standardized uptake value in FDG-PET for partial volume effect and motion artifact is not a prognostic factor in stage I non-small cell lung cancer treated with stereotactic body radiotherapy. Ann Nucl Med. 2015; 29:666–73.
Article24. Nair VJ, MacRae R, Sirisegaram A, Pantarotto JR. Pretreatment [18F]-fluoro-2-deoxy-glucose positron emission tomography maximum standardized uptake value as predictor of distant metastasis in early-stage non-small cell lung cancer treated with definitive radiation therapy: rethinking the role of positron emission tomography in personalizing treatment based on risk status. Int J Radiat Oncol Biol Phys. 2014; 88:312–8.
Article25. Tanaka H, Hayashi S, Hoshi H. Pretreatment maximum standardized uptake value on 18F-fluorodeoxyglucose positron emission tomography is a predictor of outcome for stage I nonsmall cell lung cancer after stereotactic body radiotherapy. Asia Pac J Clin Oncol. 2016; 12:e113.
Article26. Kohutek ZA, Wu AJ, Zhang Z, Foster A, Din SU, Yorke ED, et al. FDG-PET maximum standardized uptake value is prognostic for recurrence and survival after stereotactic body radiotherapy for non-small cell lung cancer. Lung Cancer. 2015; 89:115–20.
Article27. Clarke K, Taremi M, Dahele M, Freeman M, Fung S, Franks K, et al. Stereotactic body radiotherapy (SBRT) for non-small cell lung cancer (NSCLC): is FDG-PET a predictor of outcome? Radiother Oncol. 2012; 104:62–6.
Article28. Chang JY, Liu H, Balter P, Komaki R, Liao Z, Welsh J, et al. Clinical outcome and predictors of survival and pneumonitis after stereotactic ablative radiotherapy for stage I non-small cell lung cancer. Radiat Oncol. 2012; 7:152.
Article29. Vu CC, Matthews R, Kim B, Franceschi D, Bilfinger TV, Moore WH. Prognostic value of metabolic tumor volume and total lesion glycolysis from (1)(8)F-FDG PET/CT in patients undergoing stereotactic body radiation therapy for stage I nonsmall-cell lung cancer. Nucl Med Commun. 2013; 34:959–63.
Article30. Takeda A, Yokosuka N, Ohashi T, Kunieda E, Fujii H, Aoki Y, et al. The maximum standardized uptake value (SUVmax) on FDG-PET is a strong predictor of local recurrence for localized non-small-cell lung cancer after stereotactic body radiotherapy (SBRT). Radiother Oncol. 2011; 101:291–7.
Article31. Horne ZD, Clump DA, Vargo JA, Shah S, Beriwal S, Burton SA, et al. Pretreatment SUVmax predicts progression-free survival in early-stage non-small cell lung cancer treated with stereotactic body radiation therapy. Radiat Oncol. 2014; 9:41.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Role of Radiation Therapy for Non-small Cell Lung Cancer: Focused on Stereotactic Ablative Radiation Therapy in Stage I
- Stereotactic Body Radiotherapy for Early Stage Lung Cancer
- The Role of Stereotactic Ablative Radiotherapy for Early-Stage and Oligometastatic Non-small Cell Lung Cancer: Evidence for Changing Paradigms
- Response Evaluation after Stereotactic Ablative Radiotherapy for Lung Cancer
- Local ablative radiotherapy for oligometastatic non-small cell lung cancer