Ann Rehabil Med.
2020 Feb;44(1):85-89. 10.5535/arm.2020.44.1.85.
Thoracolumbar Junction Syndrome Accompanying Renal Artery Stenosis: A Case Report
- Affiliations
-
- 1Department of Physical Medicine and Rehabilitation, Soonchunhyang University Bucheon Hospital, Soonchunhyang University College of Medicine, Bucheon, Korea
- 2Department of Physical Medicine and Rehabilitation, Soonchunhyang University Cheonan Hospital, Soonchunhyang University College of Medicine, Cheonan, Korea
- 3Department of Family Medicine, Sarang Clinic, Jinju, Korea
- 4Department of Emergency Medicine, Soonchunhyang University Cheonan Hospital, Soonchunhyang University College of Medicine, Cheonan, Korea
- 5Department of Rehabilitation Medicine, Catholic University of Daegu School of Medicine, Daegu, Korea
- KMID: 2501049
- DOI: http://doi.org/10.5535/arm.2020.44.1.85
Abstract
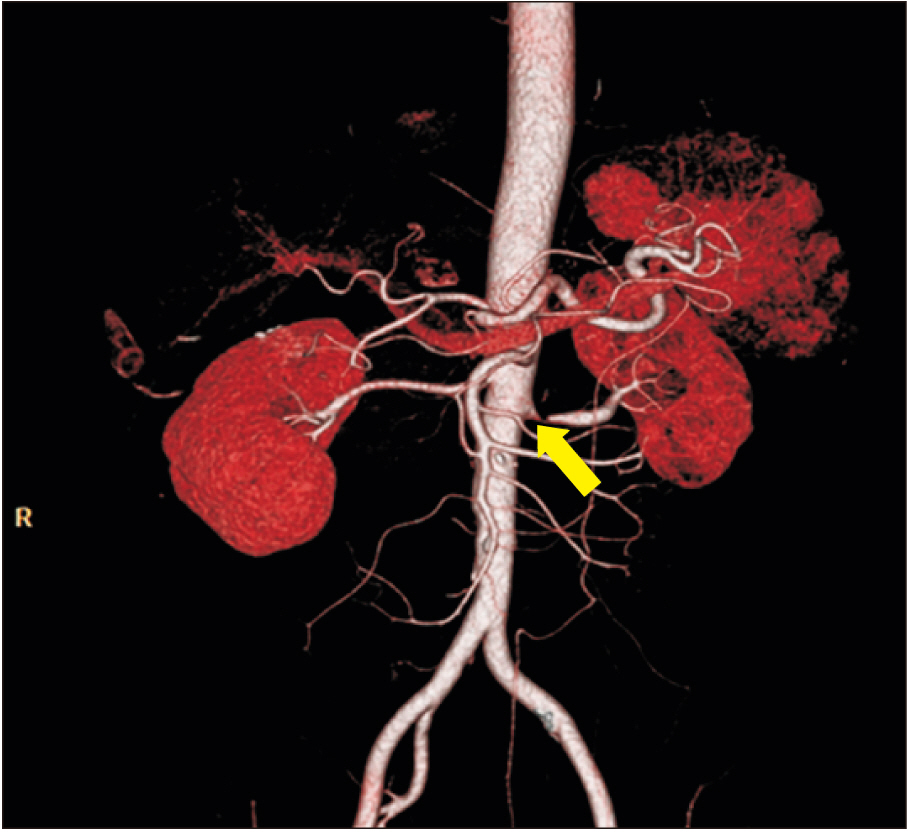
- Flank pain is a common reason for visits to the emergency room. The most common reason warranting hospital visits are urology-related problems. However, there are many other causes, such as musculoskeletal lesions, that difficult to achieve a correct diagnosis. Here, we describe a rare case of flank pain caused by thoracolumbar junction syndrome, accompanying renal artery stenosis. A 54-year-old male with hypertension presented with severe left flank pain for 1 week. Initially, he was diagnosed with left renal artery stenosis by computed tomography and decreased renal function on renal scan (Tc-99m DTPA). Although a stent was inserted into the left renal artery, flank pain persisted with only minor improvement. Through detailed physical examination, he was finally diagnosed with thoracolumbar junction syndrome. After three injections in the left deep paravertebral muscles at the T10–T12 levels, flank pain completely ceased. Clinicians must consider thoracolumbar junction syndrome, when treating patients with flank pain.
Figure
Reference
-
1. Bueschen AJ. Flank pain. In : Walker HK, Hall WD, Hurst JW, editors. Clinical methods: the history, physical, and laboratory examinations. 3rd ed. Boston: Butterworths;1990. p. 845–6.2. Smith RC, Levine J, Dalrymple NC, Barish M, Rosenfield AT. Acute flank pain: a modern approach to diagnosis and management. Semin Ultrasound CT MR. 1999; 20:108–35.3. Maigne R. Thoracolumbar junction syndrome. Diagnosis and treatment of pain of vertebral origin. 2nd ed. Boca Raton, FL: CRC Press;2006. p. 383–8.4. Singh RR, McArdle ZM, Iudica M, Easton LK, Booth LC, May CN, et al. Sustained Decrease in blood pressure and reduced anatomical and functional reinnervation of renal nerves in hypertensive sheep 30 months after catheter-based renal denervation. Hypertension. 2019; 73:718–27.
Article5. Kirkpatrick JJ, Leslie SW. Anatomy, abdomen and pelvis, kidney nerves [Internet]. Treasure Island, FL: StatPearls Publishing;2019. [cited 2020 Jan 15]. Available from: https://www.ncbi.nlm.nih.gov/pubmed/29083631.6. Shokeir AA. Renal colic: new concepts related to pathophysiology, diagnosis and treatment. Curr Opin Urol. 2002; 12:263–9.
Article7. Maigne R. Low back pain of thoracolumbar origin (T11-T12-L1). Diagnosis and treatment of pain of vertebral origin. 2nd ed. Boca Raton, FL: CRC Press;2006. p. 289–98.8. Seong JW. Principle and insight into pain. Paju, Korea: Koonja Press;2012. p. 844–55.9. Han SE, Lin CS, Boland RA, Kiernan MC. Nerve compression, membrane excitability, and symptoms of carpal tunnel syndrome. Muscle Nerve. 2011; 44:402–9.
Article10. Alptekin K, Ornek NI, Aydın T, Alkan M, Toprak M, A Balcı L, et al. Effectiveness of exercise and local steroid injections for the thoracolumbar junction syndrome (The Maigne’s syndrome) treatment. Open Orthop J. 2017; 11:467–77.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Renal Artery Stenosis Combined with Ureteropelvic Junction Obstruction in A Child
- A Case of Renovascular Hypertension Controlled by Renal Artery Embolization
- One Case Report with the Occlusion of the Superior Mesenteric Artery and Left Renal Artery Complicated in the Mitral Stenosis
- Detection of Segmental Branch Renal Artery Stenosis by Doppler US: A Case Report
- Pain Around the Posterior Iliac Crest of Thoracolumbar Origin