Ann Rehabil Med.
2020 Feb;44(1):69-76. 10.5535/arm.2020.44.1.69.
Factors Affecting the Discharge Destination of Patients With Spinal Bone Metastases
- Affiliations
-
- 1Division of Physical Therapy, Kochi Professional University of Rehabilitation, Kochi, Japan
- 2Department of Orthopaedic Surgery, Okayama University, Okayama, Japan
- 3Department of Rehabilitation Medicine, National Hospital Organization Shikoku Cancer Center, Ehime, Japan
- KMID: 2501047
- DOI: http://doi.org/10.5535/arm.2020.44.1.69
Abstract
Objective
To investigate the factors affecting the discharge destination of patients with spinal bone metastases.
Methods
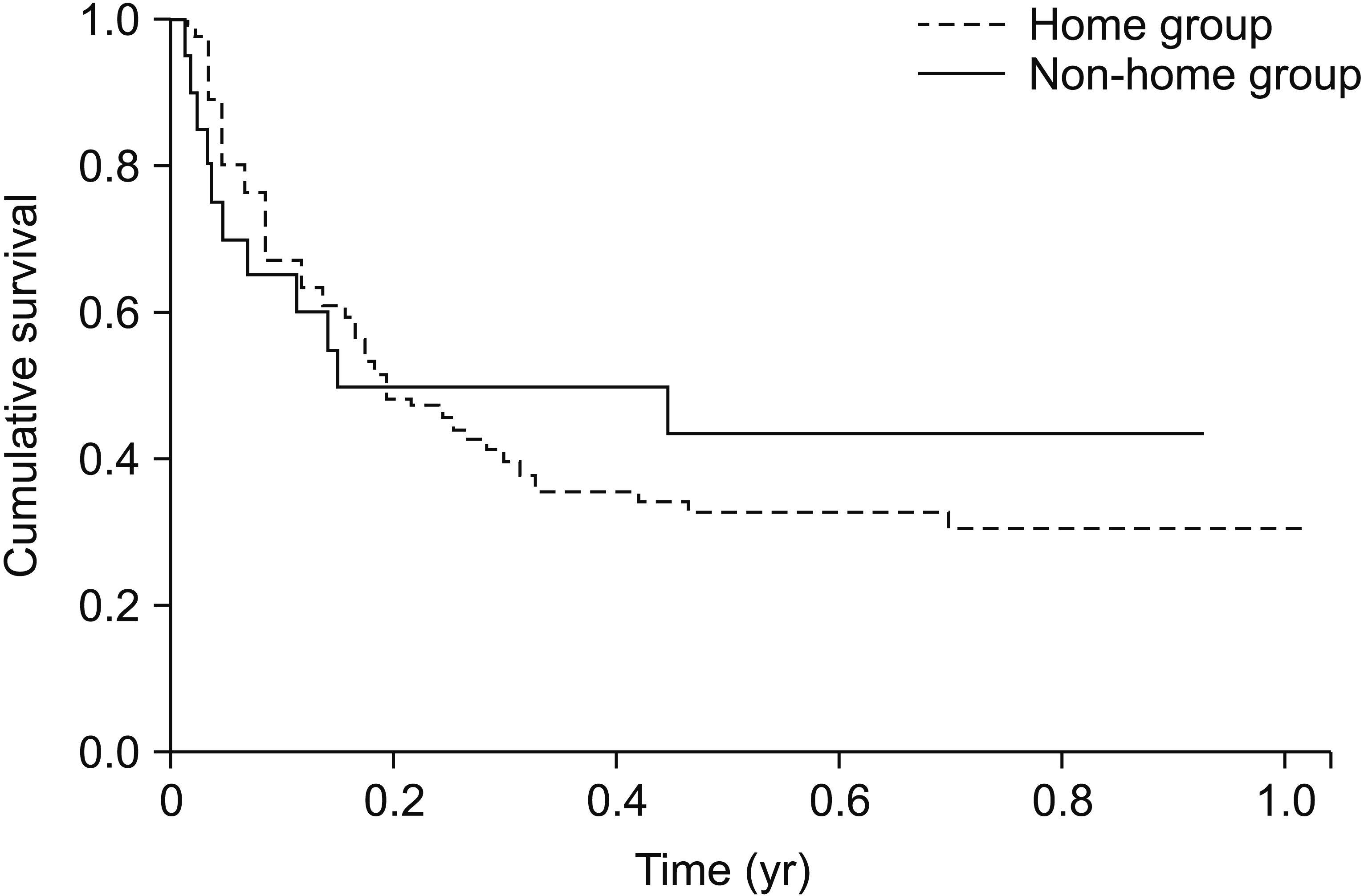
We reviewed the medical records of patients admitted to our institute with a diagnosis of skeletalrelated events secondary to malignant disease. Exclusion criteria comprised decreased cognitive function and hypercalcemia, brain metastasis, peritoneal dissemination, and pleural dissemination. The factors examined included the discharge destination, age, sex, the Barthel Index (BI) at admission and discharge, pain at admission and discharge, number of co-resident household members, length of hospital stay, treatment strategy, spinal instability neoplastic score, vertebral body collapse, spinal level of bone metastases, and motor paralysis. For the discharge destination, patients at discharge were grouped into two categories. The home group included patients discharged to their own homes, and the non-home group included patients discharged to other hospitals.
Results
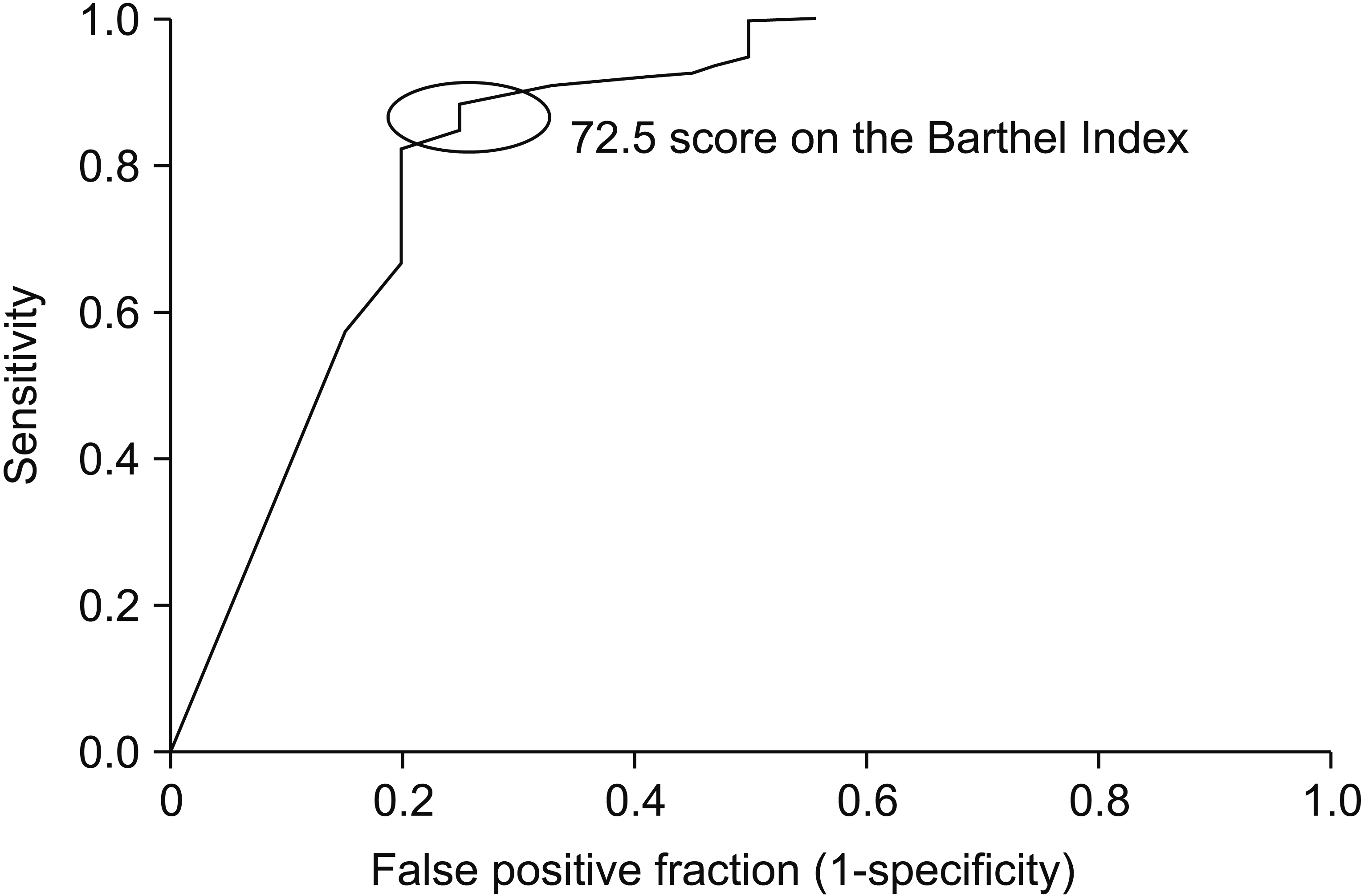
Of 140 patients, the home group comprised 120 patients and the non-home group comprised 20 patients. Activities of daily living (ADL) and pain at rest and during motion improved significantly in the home group, whereas only pain at rest and during motion improved significantly in the non-home group. The results indicated that discharge BI and motor paralysis were the best predictors of the discharge destination; a BI cut-off value of 72.5 predicted discharge to home.
Conclusion
This study showed that the ADL level on discharge and motor paralysis affected the discharge destination of patients with spinal bone metastases. These results are likely to be helpful in predicting the discharge destination of patients with spinal bone metastases.
Keyword
Figure
Reference
-
1. Coleman RE. Metastatic bone disease: clinical features, pathophysiology and treatment strategies. Cancer Treat Rev. 2001; 27:165–76.2. Harrington KD. Orthopedic surgical management of skeletal complications of malignancy. Cancer. 1997; 80:1614–27.
Article3. Barron KD, Hirano A, Araki S, Terry RD. Experiences with metastatic neoplasms involving the spinal cord. Neurology. 1959; 9:91–106.
Article4. Walsh GL, Gokaslan ZL, McCutcheon IE, Mineo MT, Yasko AW, Swisher SG, et al. Anterior approaches to the thoracic spine in patients with cancer: indications and results. Ann Thorac Surg. 1997; 64:1611–8.5. Black P. Spinal metastasis: current status and recommended guidelines for management. Neurosurgery. 1979; 5:726–46.6. Schaberg J, Gainor BJ. A profile of metastatic carcinoma of the spine. Spine (Phila Pa 1976). 1985; 10:19–20.
Article7. Stark RJ, Henson RA, Evans SJ. Spinal metastases: a retrospective survey from a general hospital. Brain. 1982; 105:189–213.8. Vieth RG, Odom GL. Extradural spinal metastases and their neurosurgical treatment. J Neurosurg. 1965; 23:501–8.
Article9. Bunting RW, Boublik M, Blevins FT, Dame CC, Ford LA, Lavine LS. Functional outcome of pathologic fracture secondary to malignant disease in a rehabilitation hospital. Cancer. 1992; 69:98–102.
Article10. Tang V, Harvey D, Park Dorsay J, Jiang S, Rathbone MP. Prognostic indicators in metastatic spinal cord compression: using functional independence measure and Tokuhashi scale to optimize rehabilitation planning. Spinal Cord. 2007; 45:671–7.
Article11. Denti L, Agosti M, Franceschini M. Outcome predictors of rehabilitation for first stroke in the elderly. Eur J Phys Rehabil Med. 2008; 44:3–11.12. Okuno Y, Miyasaka T, Dobashi K. Factors influencing the outcome of acute rehabilitation: functional independence measure assessment at discharge. J Phys Ther Sci. 2012; 24:491–4.
Article13. Fisher CG, DiPaola CP, Ryken TC, Bilsky MH, Shaffrey CI, Berven SH, et al. A novel classification system for spinal instability in neoplastic disease: an evidencebased approach and expert consensus from the Spine Oncology Study Group. Spine (Phila Pa 1976). 2010; 35:E1221–9.14. Mahoney FI, Barthel DW. Functional evaluation: the barthel index. Md State Med J. 1965; 14:61–5.15. Borg G. Psychophysical scaling with applications in physical work and the perception of exertion. Scand J Work Environ Health. 1990; 16 Suppl 1:55–8.
Article16. Oczkowski WJ, Barreca S. The functional independence measure: its use to identify rehabilitation needs in stroke survivors. Arch Phys Med Rehabil. 1993; 74:1291–4.
Article17. Massucci M, Perdon L, Agosti M, Celani MG, Righetti E, Recupero E, et al. Prognostic factors of activity limitation and discharge destination after stroke rehabilitation. Am J Phys Med Rehabil. 2006; 85:963–70.
Article18. Granger CV, Dewis LS, Peters NC, Sherwood CC, Barrett JE. Stroke rehabilitation: analysis of repeated Barthel index measures. Arch Phys Med Rehabil. 1979; 60:14–7.19. McKinley WO, Conti-Wyneken AR, Vokac CW, Cifu DX. Rehabilitative functional outcome of patients with neoplastic spinal cord compressions. Arch Phys Med Rehabil. 1996; 77:892–5.20. Agarwal V, McRae MP, Bhardwaj A, Teasell RW. A model to aid in the prediction of discharge location for stroke rehabilitation patients. Arch Phys Med Rehabil. 2003; 84:1703–9.21. Koyama T, Sako Y, Konta M, Domen K. Poststroke discharge destination: functional independence and sociodemographic factors in urban Japan. J Stroke Cerebrovasc Dis. 2011; 20:202–7.
Article22. Sommerfeld DK, von Arbin MH. Disability test 10 days after acute stroke to predict early discharge home in patients 65 years and older. Clin Rehabil. 2001; 15:528–34.
Article23. Cormie P, Newton RU, Spry N, Joseph D, Taaffe DR, Galvao DA. Safety and efficacy of resistance exercise in prostate cancer patients with bone metastases. Prostate Cancer Prostatic Dis. 2013; 16:328–35.
Article24. Cormie P, Galvao DA, Spry N, Joseph D, Taaffe DR, Newton RU. Functional benefits are sustained after a program of supervised resistance exercise in cancer patients with bone metastases: longitudinal results of a pilot study. Support Care Cancer. 2014; 22:1537–48.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Discharge Destination of Rehabilitation Inpatients in a Tertiary Hospital
- Factors Affecting Discharge Delay in Lumbar Spinal Surgery Patients Who were Treated according to a Critical Pathway
- Imaging Findings of Spinal Metastases with Differential Diagnosis: Focusing on Solitary Spinal Lesion in Older Patients
- Predictive Factors of Palliative Radiotherapy Response and Survival in Patients with Spinal Metastases from Hepatocellular Carcinoma
- Discharge Destinations after Acute Rehabilitation Care