Clin Endosc.
2020 Jan;53(1):73-81. 10.5946/ce.2019.052.
Practice Patterns and Use of Endoscopic Retrograde Cholangiopancreatography in the Management of Recurrent Acute Pancreatitis
- Affiliations
-
- 1Department of Medicine, Duke University, Durham, NC, USA
- 2Division of Digestive Disease, Department of Medicine, Emory University, Atlanta, GA, USA
- KMID: 2500908
- DOI: http://doi.org/10.5946/ce.2019.052
Abstract
- Background/Aims
There are conflicting opinions regarding the management of recurrent acute pancreatitis (RAP). While some physicians recommend endoscopic retrograde cholangiopancreatography (ERCP) in this setting, others consider it to be contraindicated in patients with RAP. The aim of this study was to assess the practice patterns and clinical features influencing the management of RAP in the US.
Methods
An anonymous 35-question survey instrument was developed and refined through multiple iterations, and its use was approved by our Institutional Review Board. The survey was distributed via email to 408 gastroenterologists to assess the practice patterns in the management of RAP in multiple clinical scenarios.
Results
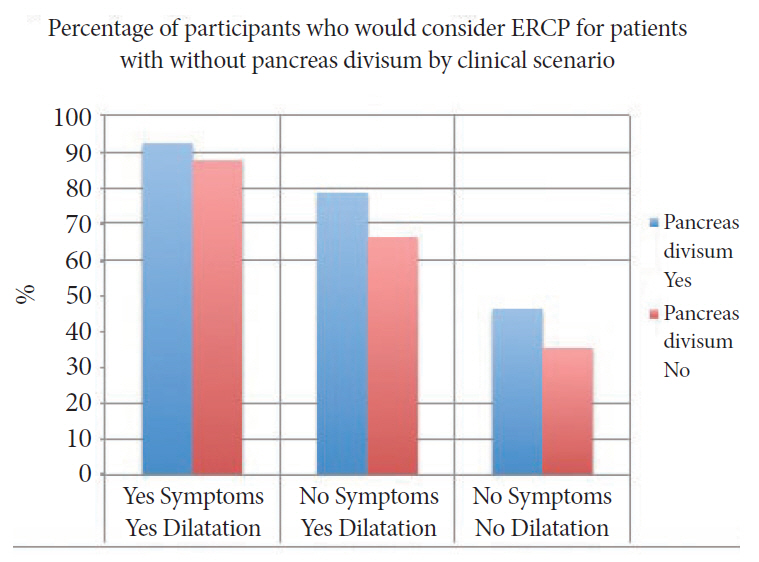
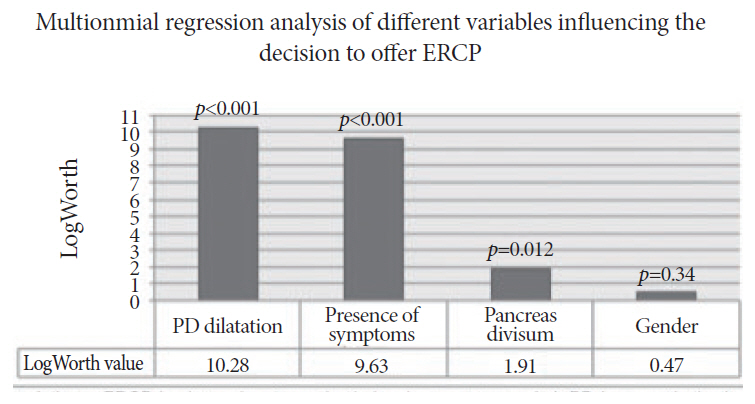
The survey was completed by 65 participants representing 36 of the top academic/tertiary care centers across the country. Approximately 90.8% of the participants indicated that they might offer or recommend ERCP in the management of RAP. Multinomial logistic regression analysis revealed that ductal dilatation and presence of symptoms were the most predictive variables (p<0.001) for offering ERCP.
Conclusions
A preponderance of the respondents would consider ERCP among patients with RAP presenting to tertiary care centers in the US. Ductal dilatation, presence of symptoms, and pancreas divisum significantly increased the likelihood of a recommendation for ERCP
Keyword
Figure
Cited by 1 articles
-
Endoscopic Retrograde Cholangiopancreatography in Recurrent Acute Pancreatitis: Determining the Optimal Subgroup of Patients in Whom the Procedure is Beneficial
Tae Yoon Lee, Takuji Iwashita
Clin Endosc. 2020;53(1):5-6. doi: 10.5946/ce.2020.004.
Reference
-
1. Das R, Yadav D, Papachristou GI. Endoscopic treatment of recurrent acute pancreatitis and smoldering acute pancreatitis. Gastrointest Endosc Clin N Am. 2015; 25:737–748.
Article2. Machicado JD, Yadav D. Epidemiology of recurrent acute and chronic pancreatitis: similarities and differences. Dig Dis Sci. 2017; 62:1683–1691.
Article3. Yadav D, Lowenfels AB. Trends in the epidemiology of the first attack of acute pancreatitis: a systematic review. Pancreas. 2006; 33:323–330.4. Shen HN, Lu CL, Li CY. Epidemiology of first-attack acute pancreatitis in Taiwan from 2000 through 2009: a nationwide population-based study. Pancreas. 2012; 41:696–702.5. Omdal T, Dale J, Lie SA, Iversen KB, Flaatten H, Ovrebo K. Time trends in incidence, etiology, and case fatality rate of the first attack of acute pancreatitis. Scand J Gastroenterol. 2011; 46:1389–1398.
Article6. Sankaran SJ, Xiao AY, Wu LM, Windsor JA, Forsmark CE, Petrov MS. Frequency of progression from acute to chronic pancreatitis and risk factors: a meta-analysis. Gastroenterology. 2015; 149:1490–1500. e1.
Article7. Roberts JR, Romagnuolo J. Endoscopic therapy for acute recurrent pancreatitis. Gastrointest Endosc Clin N Am. 2013; 23:803–819.
Article8. Steinberg W, Tenner S. Acute pancreatitis. N Engl J Med. 1994; 330:1198–1210.
Article9. Gabbrielli A, Pezzilli R, Uomo G, et al. ERCP in acute pancreatitis: what takes place in routine clinical practice? World J Gastrointest Endosc. 2010; 2:308–313.
Article10. Somani P, Navaneethan U. Role of ERCP in patients with idiopathic recurrent acute pancreatitis. Curr Treat Options Gastroenterol. 2016; 14:327–339.11. Kaw M, Brodmerkel GJ Jr. ERCP, biliary crystal analysis, and sphincter of Oddi manometry in idiopathic recurrent pancreatitis. Gastrointest Endosc. 2002; 55:157–162.
Article12. Mariani A, Di Leo M, Petrone MC, et al. Outcome of endotherapy for pancreas divisum in patients with acute recurrent pancreatitis. World J Gastroenterol. 2014; 20:17468–17475.
Article13. Bin-Sagheer ST, Brady PG, Mamel JJ, Robinson B. Reduction in the incidence of pancreatitis in patients undergoing sphincter of Oddi manometry: a successful quality improvement project. South Med J. 2003; 96:223–225.
Article14. Brackbill S, Young S, Schoenfeld P, Elta G. A survey of physician practices on prophylactic pancreatic stents. Gastrointest Endosc. 2006; 64:45–52.
Article15. Saltzman JR. Endoscopic treatment of pancreas divisum: why, when, and how? Gastrointest Endosc. 2006; 64:712–715.
Article16. Coté GA, Imperiale TF, Schmidt SE, et al. Similar efficacies of biliary, with or without pancreatic, sphincterotomy in treatment of idiopathic recurrent acute pancreatitis. Gastroenterology. 2012; 143:1502–1509. e1.
Article17. Watson RR, Klapman J, Komanduri S, Shah JN, Wani S, Muthusamy R. Wide disparities in attitudes and practices regarding Type II sphincter of Oddi dysfunction: a survey of expert U.S. endoscopists. Endosc Int Open. 2016; 4:E941–E946.
Article18. Fogel EL, Toth TG, Lehman GA, DiMagno MJ, DiMagno EP. Does endoscopic therapy favorably affect the outcome of patients who have recurrent acute pancreatitis and pancreas divisum? Pancreas. 2007; 34:21–45.
Article19. Moffatt DC, Coté GA, Avula H, et al. Risk factors for ERCP-related complications in patients with pancreas divisum: a retrospective study. Gastrointest Endosc. 2011; 73:963–970.
Article20. Chen JJ, Wang XM, Liu XQ, et al. Risk factors for post-ERCP pancreatitis: a systematic review of clinical trials with a large sample size in the past 10 years. Eur J Med Res. 2014; 19:26.
Article21. Cotton PB, Garrow DA, Gallagher J, Romagnuolo J. Risk factors for complications after ERCP: a multivariate analysis of 11,497 procedures over 12 years. Gastrointest Endosc. 2009; 70:80–88.
Article22. Perney P, Berthier E, Pageaux GP, et al. Are drugs a risk factor of post-ERCP pancreatitis? Gastrointest Endosc. 2003; 58:696–700.
Article23. Testoni PA, Mariani A, Giussani A, et al. Risk factors for post-ERCP pancreatitis in high- and low-volume centers and among expert and non-expert operators: a prospective multicenter study. Am J Gastroenterol. 2010; 105:1753–1761.
Article24. Wilcox CM, Phadnis M, Varadarajulu S. Biliary stent placement is associated with post-ERCP pancreatitis. Gastrointest Endosc. 2010; 72:546–550.
Article25. Cheng CL, Sherman S, Watkins JL, et al. Risk factors for post-ERCP pancreatitis: a prospective multicenter study. Am J Gastroenterol. 2006; 101:139–147.
Article26. Zhou W, Li Y, Zhang Q, et al. Risk factors for postendoscopic retrograde cholangiopancreatography pancreatitis: a retrospective analysis of 7,168 cases. Pancreatology. 2011; 11:399–405.
Article27. Christensen M, Matzen P, Schulze S, Rosenberg J. Complications of ERCP: a prospective study. Gastrointest Endosc. 2004; 60:721–731.
Article28. Barkay O, Sherman S, McHenry L, et al. Therapeutic EUS-assisted endoscopic retrograde pancreatography after failed pancreatic duct cannulation at ERCP. Gastrointest Endosc. 2010; 71:1166–1173.
Article29. Mallery S, Matlock J, Freeman ML. EUS-guided rendezvous drainage of obstructed biliary and pancreatic ducts: report of 6 cases. Gastrointest Endosc. 2004; 59:100–107.
Article30. Romagnuolo J, Durkalski V, Fogel EL, et al. Outcomes after minor papilla endoscopic sphincterotomy (MPES) for unexplained acute pancreatitis and pancreas divisum: final results of the multicenter prospective FRAMES (frequency of recurrent acute pancreatitis after minor papilla endoscopic sphincterotomy) study. Gastrointest Endosc. 2013; 77(5 Suppl):AB379.31. Testoni PA, Caporuscio S, Bagnolo F, Lella F. Idiopathic recurrent pancreatitis: long-term results after ERCP, endoscopic sphincterotomy, or ursodeoxycholic acid treatment. Am J Gastroenterol. 2000; 95:1702–1707.
Article32. Wehrmann T. Long-term results (≥ 10 years) of endoscopic therapy for sphincter of Oddi dysfunction in patients with acute recurrent pancreatitis. Endoscopy. 2011; 43:202–207.
Article33. Das R, Clarke B, Tang G, et al. Endoscopic sphincterotomy (ES) may not alter the natural history of idiopathic recurrent acute pancreatitis (IRAP). Pancreatology. 2016; 16:770–777.
Article34. Jacob L, Geenen JE, Catalano MF, Geenen DJ. Prevention of pancreatitis in patients with idiopathic recurrent pancreatitis: a prospective nonblinded randomized study using endoscopic stents. Endoscopy. 2001; 33:559–562.
Article35. Guo A, Poneros JM. The role of endotherapy in recurrent acute pancreatitis. Gastrointest Endosc Clin N Am. 2018; 28:455–476.
Article36. Cote GA. SpHincterotomy for acute recurrent pancreatitis (SHARP) [Internet]. Bethesda (MD): ClinicalTrials.gov;c2018 [updated 2019 May 23; cited 2019 May 23]. Available from: https://clinicaltrials.gov/ct2/show/NCT03609944.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Usefulness of ERCP in Acute Pancreatitis
- Gallstone pancreatitis: general clinical approach and the role of endoscopic retrograde cholangiopancreatography
- Evaluation of Recurrent or Idiopathic Pancreatitis
- Indications and Timing of ERCP and Cholecystectomy for Biliary Pancreatitis
- Endoscopic retrograde cholangiopancreatography complications: Techniques to reduce risk and management strategies