Ann Surg Treat Res.
2020 Apr;98(4):199-205. 10.4174/astr.2020.98.4.199.
Characteristics of minute T1 colorectal cancer in relevance to pathology and treatment
- Affiliations
-
- 1Center for Colorectal Cancer, Research Institute and Hospital, National Cancer Center, Goyang, Korea
- 2Center for Cancer Prevention and Early Detection, Research Institute and Hospital, National Cancer Center, Goyang, Korea
- KMID: 2500820
- DOI: http://doi.org/10.4174/astr.2020.98.4.199
Abstract
- Purpose
Minute T1 colorectal cancer (CRC) lesions (≤5 mm) are rare; however, little is known about their characteristics and aggressiveness. In this study, we evaluated the characteristics of minute T1 CRC in relevance to pathology and treatment.
Methods
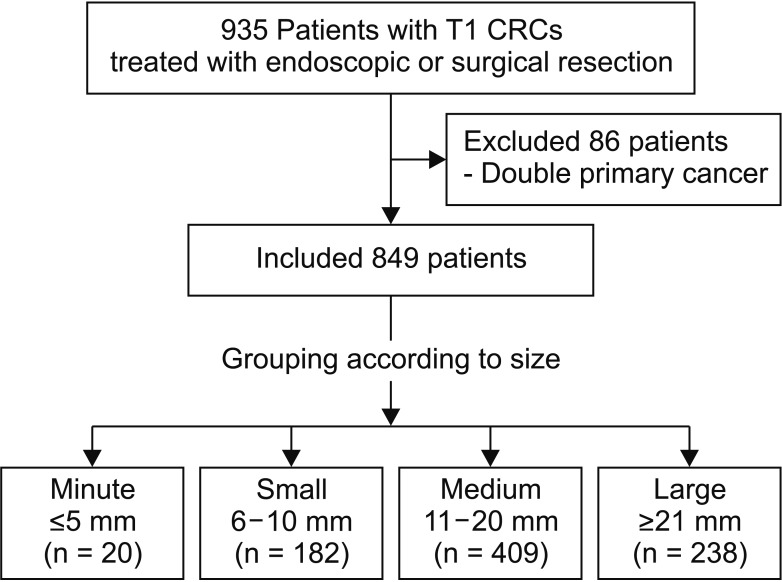
This retrospective study included 849 patients with T1 CRC endoscopically or surgically treated between January 2001 and December 2016. The patients were stratified into 4 groups according to tumor size; minute group (≤5 mm), small group (6–10 mm), medium group (11–20 mm), and large group (≥21 mm). Clinicopathological variables were evaluated with respect to tumor size.
Results
The incidence of the minute T1 CRC was 2.4% (20 of 849). Minute T1 CRC was significantly associated with flat type (minute, 25%; small, 12.6%; medium, 8.8%; large, 12.6%; P = 0.016), right-sided cancer (30%, 15.4%, 15.4%, 15.1%, P = 0.002) and the absence of background adenoma (BGA) (50%, 40.7%, 32.8%, 18.1%, P < 0.001). In patients who underwent surgery, lymph node metastasis (LNM) was significantly higher in the minute group (36.4%, 15.9%, 15.7%, 9.2%, P = 0.029).
Conclusion
Minute T1 CRC is significantly associated with flat type, right-sided cancers, as well as with the absence of BGA and LNM. These results suggested the minute T1 CRC lesions are often aggressive and are likely to be missed during colonoscopy.
Keyword
Figure
Reference
-
1. Togashi K, Utano K, Kijima S, Sato Y, Horie H, Sunada K, et al. Laterally spreading tumors: l imitations of computed tomography colonography. World J Gastroenterol. 2014; 20:17552–17557. PMID: 25516670.2. Kornprat P, Pollheimer MJ, Lindtner RA, Schlemmer A, Rehak P, Langner C. Value of tumor size as a prognostic variable in colorectal cancer: a critical reappraisal. Am J Clin Oncol. 2011; 34:43–49. PMID: 20101166.3. The Paris endoscopic classification of superficial neoplastic lesions: esophagus, stomach, and colon: November 30 to December 1, 2002. Gastrointest Endosc. 2003; 58(6 Suppl):S3–S43. PMID: 14652541.4. Jass JR. Do all colorectal carcinomas arise in preexisting adenomas? World J Surg. 1989; 13:45–51. PMID: 2658353.
Article5. Kleihues P, Cavenee WK. International Agency for Research on Cancer. Pathology and genetics of tumours of digestive system. Lyon: IARC Press;2000. (World Health Organization classification of tumours; v. 2).6. Kudo S. Endoscopic mucosal resection of flat and depressed types of early colorectal cancer. Endoscopy. 1993; 25:455–461. PMID: 8261988.
Article7. Kitajima K, Fujimori T, Fujii S, Takeda J, Ohkura Y, Kawamata H, et al. Correlations between lymph node metastasis and depth of submucosal invasion in submucosal invasive colorectal carcinoma: a Japanese collaborative study. J Gastroenterol. 2004; 39:534–543. PMID: 15235870.
Article8. Ueno H, Price AB, Wilkinson KH, Jass JR, Mochizuki H, Talbot IC. A new prognostic staging system for rectal cancer. Ann Surg. 2004; 240:832–839. PMID: 15492565.
Article9. Ha RK, Han KS, Sohn DK, Kim BC, Hong CW, Chang HJ, et al. Histopathologic risk factors for lymph node metastasis in patients with T1 colorectal cancer. Ann Surg Treat Res. 2017; 93:266–271. PMID: 29184880.
Article10. Kobayashi Y, Kudo SE, Miyachi H, Hosoya T, Ikehara N, Ohtsuka K, et al. Clinical usefulness of pit patterns for detecting colonic lesions requiring surgical treatment. Int J Colorectal Dis. 2011; 26:1531–1540. PMID: 21607587.
Article11. Uno Y, Munakata A. The non-lifting sign of invasive colon cancer. Gastrointest Endosc. 1994; 40:485–489. PMID: 7926542.
Article12. Soetikno RM, Kaltenbach T, Rouse RV, Park W, Maheshwari A, Sato T, et al. Prevalence of nonpolypoid (flat and depressed) colorectal neoplasms in asymptomatic and symptomatic adults. JAMA. 2008; 299:1027–1035. PMID: 18319413.
Article13. Heresbach D, Barrioz T, Lapalus MG, Coumaros D, Bauret P, Potier P, et al. Miss rate for colorectal neoplastic polyps: a prospective multicenter study of back-to-back video colonoscopies. Endoscopy. 2008; 40:284–290. PMID: 18389446.
Article14. Benedict M, Galvao Neto A, Zhang X. Interval colorectal carcinoma: an unsolved debate. World J Gastroenterol. 2015; 21:12735–12741. PMID: 26668498.
Article15. Bressler B, Paszat LF, Chen Z, Rothwell DM, Vinden C, Rabeneck L. Rates of new or missed colorectal cancers af ter colonoscopy and thei r r isk factors: a population-based analysis. Gastroenterology. 2007; 132:96–102. PMID: 17241863.16. Singh S, Singh PP, Murad MH, Singh H, Samadder NJ. Prevalence, risk factors, and outcomes of interval colorectal cancers: a systematic review and meta-analysis. Am J Gastroenterol. 2014; 109:1375–1389. PMID: 24957158.
Article17. Chen TH, Yen MF, Lai MS, Koong SL, Wang CY, Wong JM, et al. Evaluation of a selective screening for colorectal carcinoma: the Taiwan Multicenter Cancer Screening (TAMCAS) project. Cancer. 1999; 86:1116–1128. PMID: 10506694.18. Kanazawa T, Watanabe T, Nagawa H. Does early polypoid colorectal cancer with depression have a pathway other than adenoma-carcinoma sequence? Tumori. 2003; 89:408–411. PMID: 14606645.
Article19. Mueller JD, Bethke B, Stolte M. Colorectal de novo carcinoma: a review of its diagnosis, histopathology, molecular biology, and clinical relevance. Virchows Arch. 2002; 440:453–460. PMID: 12021919.
Article20. Han KS, Lim SW, Sohn DK, Chang HJ, Oh JH, Lee JH, et al. Clinicopathological characteristics of T1 colorectal cancer without background adenoma. Colorectal Dis. 2013; 15:e124–e129. PMID: 23294594.
Article21. Nascimbeni R, Burgart LJ, Nivatvongs S, Larson DR. Risk of lymph node metastasis in T1 carcinoma of the colon and rectum. Dis Colon Rectum. 2002; 45:200–206. PMID: 11852333.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Risk Stratification of T1 Colorectal Cancer Metastasis to Lymph Nodes: Current Status and Perspective
- Clinical Implications of Microsatellite Instability in T1 Colorectal Cancer
- Reply on "Data on the Characteristics and the Survival of Korean Patients With Colorectal Cancer From the Korea Central Cancer Registry"
- Challenges in Implementing Endoscopic Resection for T2 Colorectal Cancer
- Commentary on "Data on the Characteristics and the Survival of Korean Patients With Colorectal Cancer From the Korea Central Cancer Registry"