Ann Hepatobiliary Pancreat Surg.
2020 May;24(2):192-197. 10.14701/ahbps.2020.24.2.192.
Reuse of liver allograft from a brain-dead recipient: A case report
- Affiliations
-
- 1Division of Hepatobiliary Surgery and Liver Transplantation, Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2500805
- DOI: http://doi.org/10.14701/ahbps.2020.24.2.192
Abstract
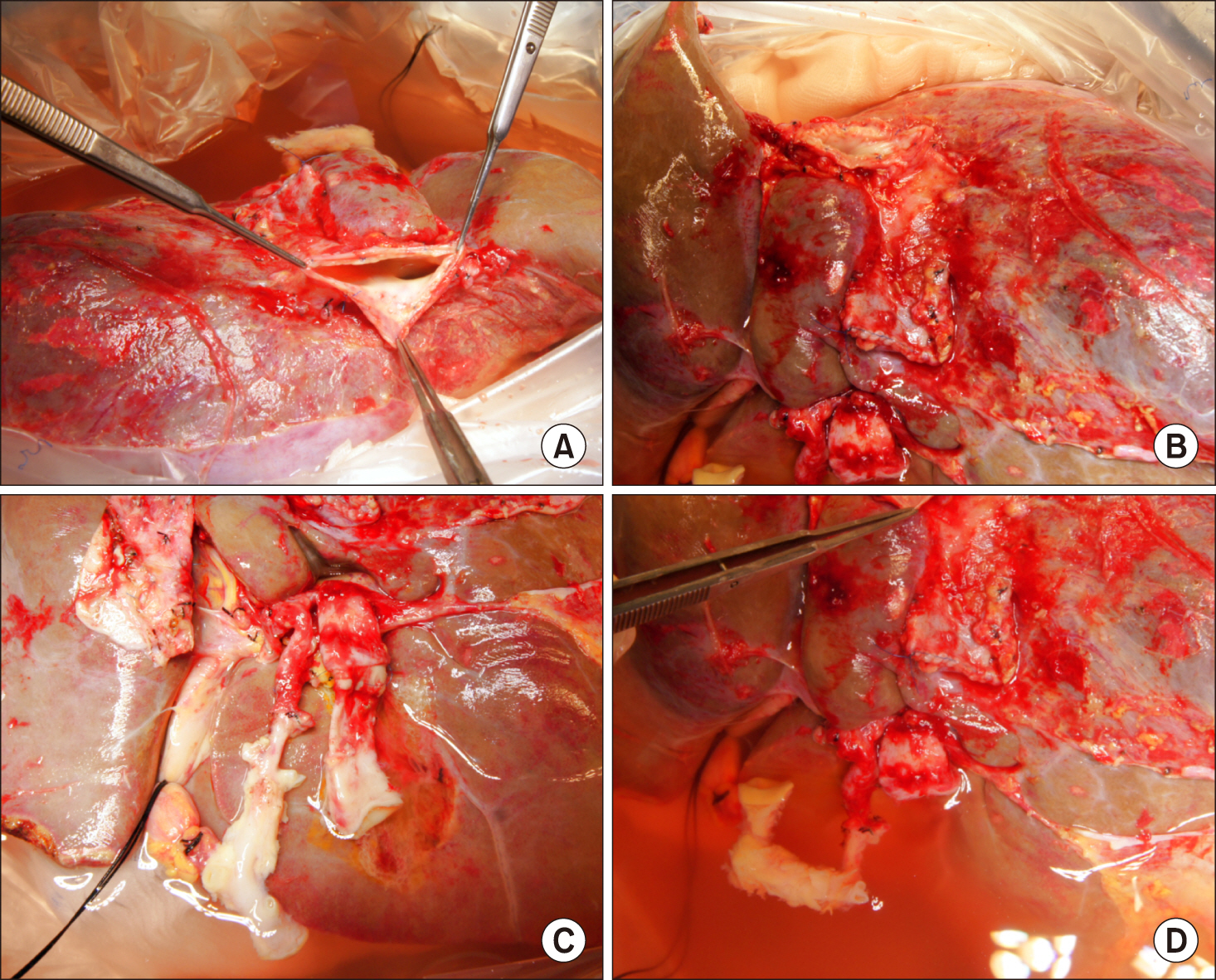
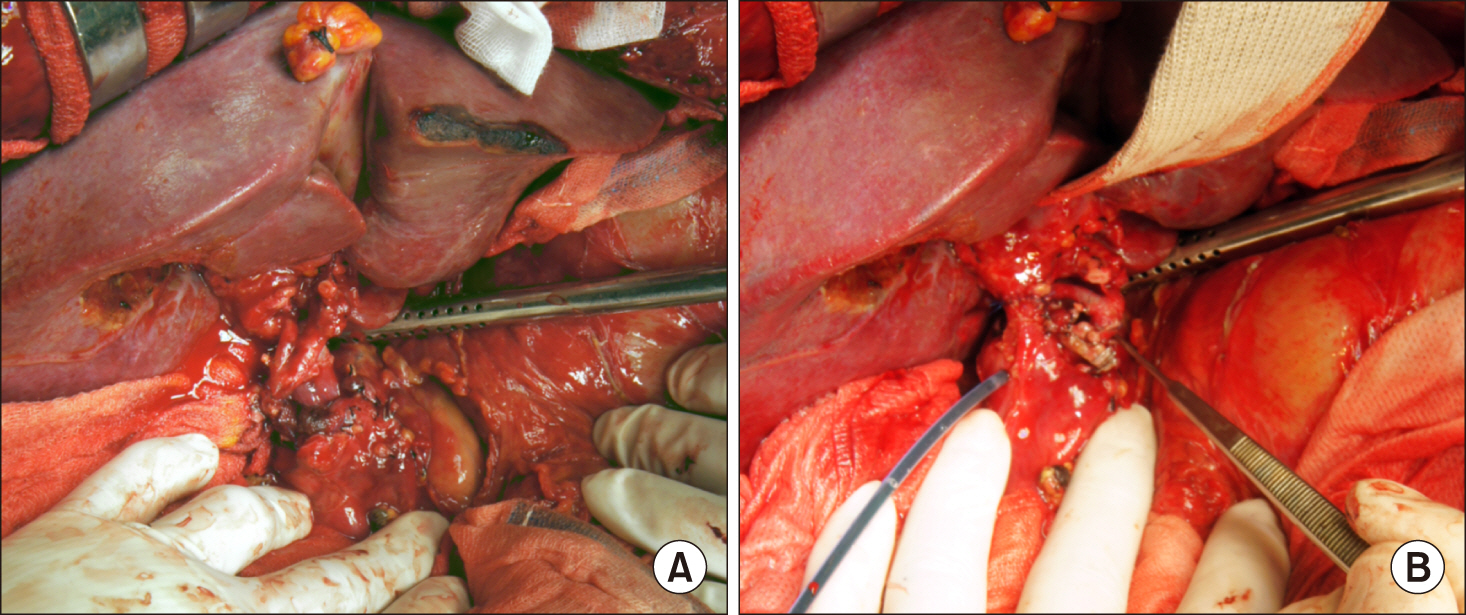
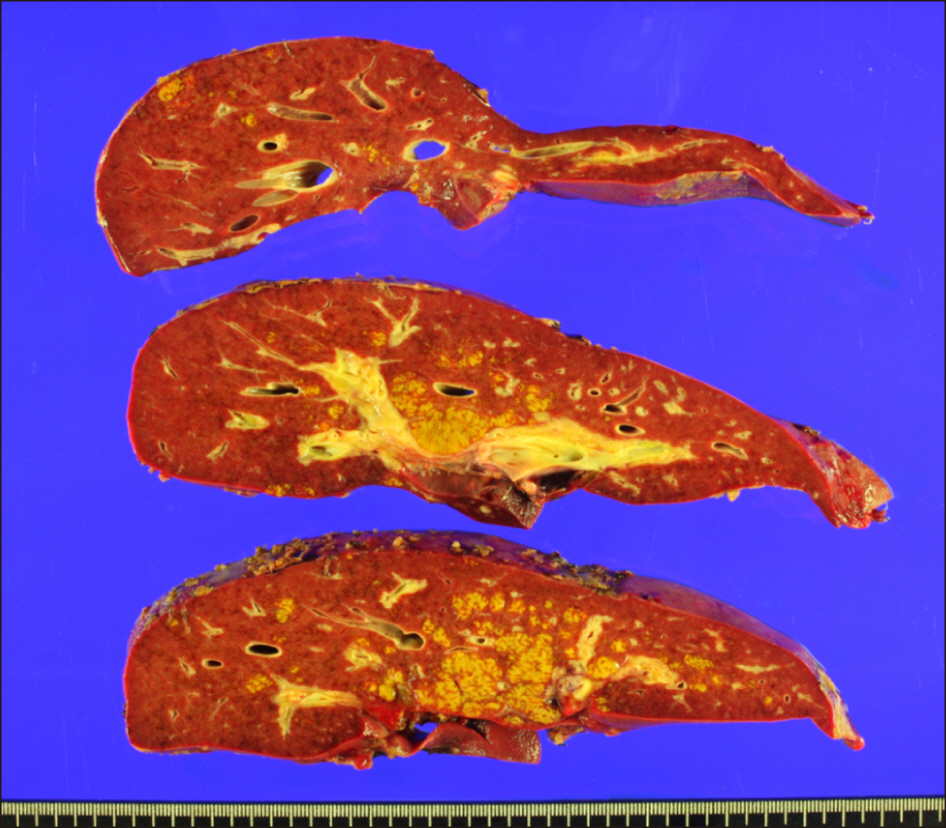
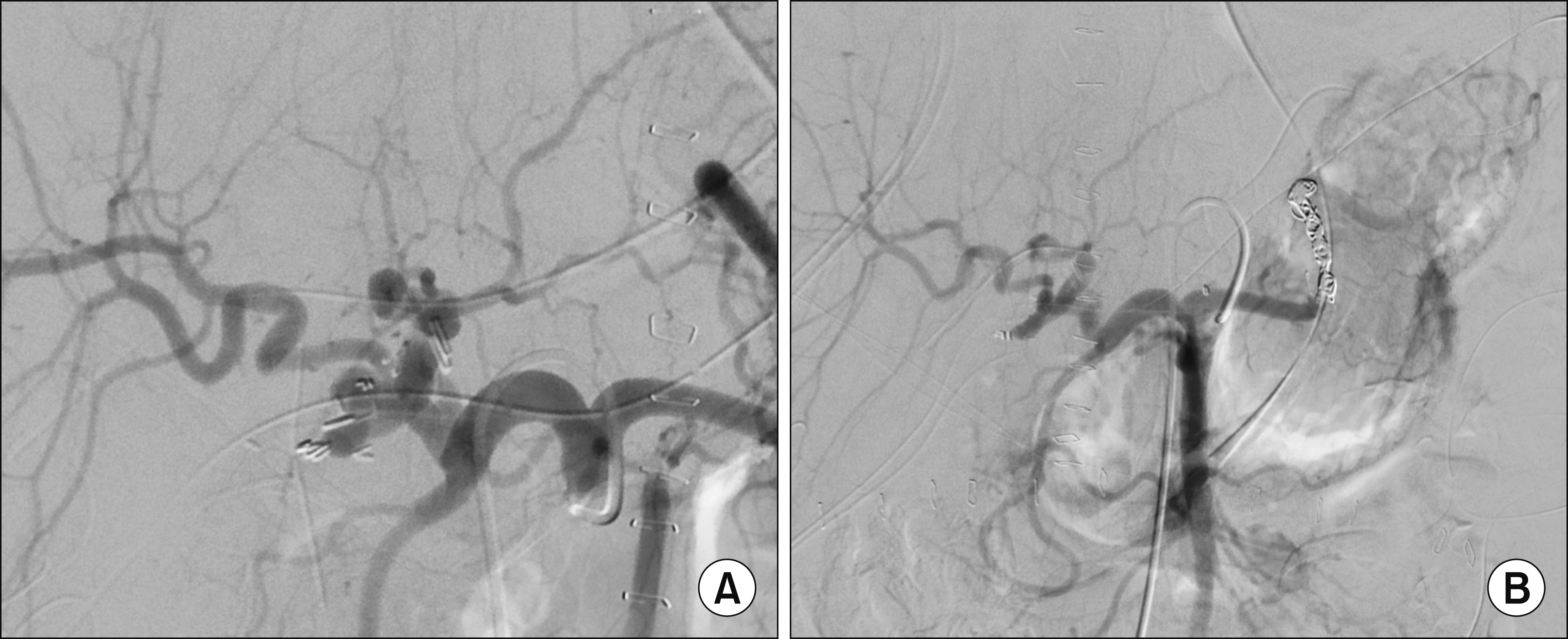
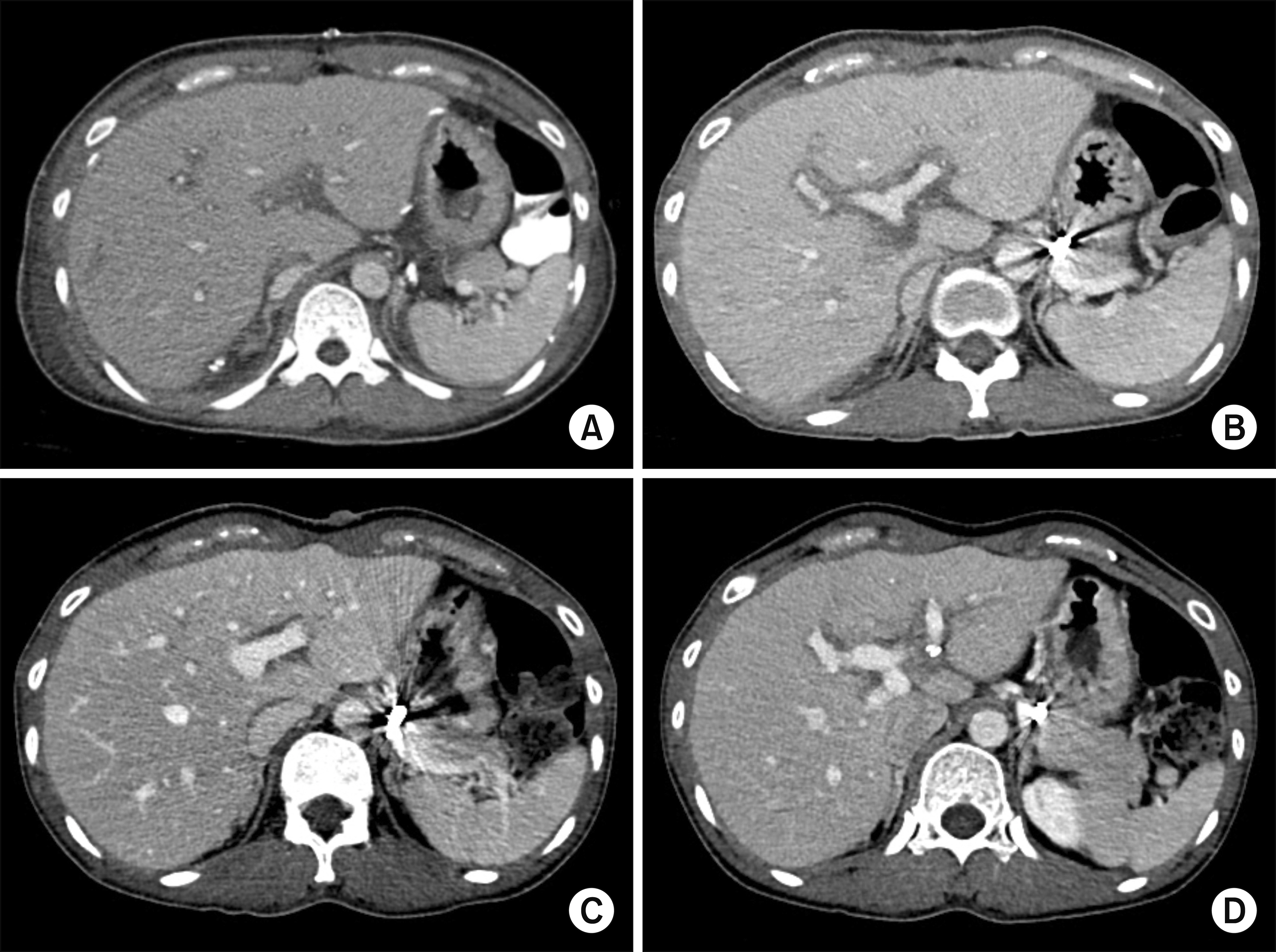
- We report our first case of deceased-donor liver transplantation (LT) using a reuse liver graft after the first LT. The recipient was a 38-year-old female with fulminant hepatic failure from toxic hepatitis. She had a history of herb intake and her liver function deteriorated progressively. She was enrolled as the Korean Network for Organ Sharing (KONOS) status 1 and the model for end-stage liver disease score was 34. The donor was a 42-year-old male patient who fell into brain death after LT for alcoholic liver cirrhosis. Donation of multiple organs including the transplanted liver graft was performed 10 days after the first LT operation. Since the liver graft appeared to be normal and frozen-section liver biopsy showed only mild fatty changes, we decided to reuse the liver graft. A modified piggy-back technique of the suprahepatic inferior vena cava reconstruction was used. Other surgical procedures were comparable to the standard deceased-donor LT procedures. The explant liver pathology revealed submassive hepatic necrosis, which was compatible with toxic hepatitis. The peak of serum liver enzyme levels were aspartate transaminase 1,063 IU/L and alanine transaminase 512 IU/L at posttransplant day 3. Since the pretransplant general condition of the recipient was very poor, hospital stay was prolonged and she was discharged 51 days after LT operation. She is currently doing well for 3 years to date. Experience in our case and the literature review suggest that a reuse liver graft can be regarded as one of the marginal grafts which can be transplantable to the LT candidates requiring urgent LT.
Keyword
Figure
Cited by 1 articles
-
Reusing hepatic grafts in Korea: a case report
Hye Young Kim, Byunghyun Choi, Minhwa Kim, YounJung Choi, Jeongrim Lee, Won Hyun Cho
Korean J Transplant. 2021;35(3):200-206. doi: 10.4285/kjt.21.0005.
Reference
-
1. López-Navidad A, Caballero F. 2003; Extended criteria for organ acceptance. Strategies for achieving organ safety and for increasing organ pool. Clin Transplant. 17:308–324. DOI: 10.1034/j.1399-0012.2003.00119.x. PMID: 12868987.
Article2. Moreno EG, García GI, González-Pinto I, Gómez SR, Loinaz SC. 1991; Successful reuse of a liver graft. Br J Surg. 78:813–814. DOI: 10.1002/bjs.1800780715. PMID: 1873708.
Article3. Tantawi B, Cherqui D, Duvoux C, Dhumeaux D, Fagniez PL. 1996; Reuse of a liver graft five days after initial transplantation. Transplantation. 62:868–869. DOI: 10.1097/00007890-199609270-00029. PMID: 8824492.
Article4. Moreno González E, Gómez R, Gonzalez Pinto I, Loinaz C, Garcia I, Maffettone V, et al. 1996; Reuse of liver grafts after early death of the first recipient. World J Surg. 20:309–312. discussion 312–313. DOI: 10.1007/s002689900049. PMID: 8661836.5. Figueras J, Pares D, González C, Ramos E, Rafecas A, Fabregat J, et al. 1997; Reuse of a transplanted liver. Transpl Int. 10:335–337. DOI: 10.1111/j.1432-2277.1997.tb00714.x. PMID: 9249947.
Article6. Pruvot FR, Roumilhac D, Dharancy S, Lambotte P, Auboiron A, Gambiez L, et al. 2004; Re-use of a liver graft and multi-organ procurement from a liver transplant patient. Transpl Int. 17:49–53. DOI: 10.1111/j.1432-2277.2004.tb00384.x. PMID: 14745488.
Article7. Rubay R, Wittebolle X, Ciccarelli O, Roggen F, Talpe S, Laterre PF, et al. 2003; Re-use of a liver allograft; an exceptional opportunity to enlarge the organ donor pool. Transpl Int. 16:497–499. DOI: 10.1111/j.1432-2277.2003.tb00355.x. PMID: 12712236.
Article8. Ortiz J, Reich DJ, Manzarbeitia C, Humar A. 2005; Successful re-use of liver allografts: three case reports and a review of the UNOS database. Am J Transplant. 5:189–192. DOI: 10.1111/j.1600-6143.2004.00635.x. PMID: 15636629.
Article9. Tayar C, Karoui M, Laurent A, Hadjhamida MB, Nhieu JT, Duvoux C, et al. 2006; Successful reuse of liver graft 13 years after initial transplantation. Transplantation. 82:1547–1548. DOI: 10.1097/01.tp.0000228238.40172.2f. PMID: 17164732.
Article10. Nafidi O, Letourneau R, Willems BE, Lapointe RW. 2007; Reuse of liver graft from a brain dead recipient. Clin Transplant. 21:773–776. DOI: 10.1111/j.1399-0012.2007.00724.x. PMID: 17988273.
Article11. Rentsch M, Meyer J, Andrassy J, Fischer-Fröhlich CL, Rust C, Mueller S, et al. 2010; Late reuse of liver allografts from brain-dead graft recipients: the Munich experience and a review of the literature. Liver Transpl. 16:701–704. DOI: 10.1002/lt.22053. PMID: 20517903.
Article12. Wong TC, She WH, Cheung TT, Chan SC, Lo CM. 2015; Case report of relay liver transplantation with graft infected with hepatitis B virus. Transplant Proc. 47:2768–2770. DOI: 10.1016/j.transproceed.2015.09.036. PMID: 26680090.
Article13. Cho WH. 2019; Organ donation in Korea in 2018 and an introduction of the Korea national organ donation system. Korean J Transplant. 33:83–97. DOI: 10.4285/jkstn.2019.33.4.83.
Article14. Ha HS, Hong JJ, Kim IO, Lee SR, Lee AY, Ha TY, et al. 2019; Deceased donor liver transplantation under the Korean model for end-stage liver disease score-based liver allocation system: 2-year allocation results at a high-volume transplantation center. Korean J Transplant. 33:112–117. DOI: 10.4285/jkstn.2019.33.4.112.
Article15. Hu XG, Kim IG, Wang HJ, Kim BW, Hong SY, Kim YB, et al. 2018; Reuse of living-donor liver graft in second recipient with long-term survival. Transplant Proc. 50:3984–3987. DOI: 10.1016/j.transproceed.2018.03.004. PMID: 30577301.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Successful Reuse of a Kidney Allograft from a Brain-Dead Donor into a Second Recipient: A Case Report
- Reuse of liver allograft from a brain-dead recipient: a case report
- Reusing Recipient Vessel in Microsurgery for the Reconstruction of Lower Extremity Burn: A Case Report
- Nocardia Brain Abscess in a Liver Transplant Recipient
- Reusing hepatic grafts in Korea: a case report