Anesth Pain Med.
2020 Jan;15(1):35-40. 10.17085/apm.2020.15.1.35.
Does desflurane need more irrigating-pump pressure for the visibility in arthroscopic shoulder surgery than sevoflurane?
- Affiliations
-
- 1Departments of Anesthesiology and Pain Medicine, National Health Insurance Service Ilsan Hospital, Goyang, Korea
- 2Departments of Orthopedic Surgery, National Health Insurance Service Ilsan Hospital, Goyang, Korea
- KMID: 2500452
- DOI: http://doi.org/10.17085/apm.2020.15.1.35
Abstract
- Background
In arthroscopic shoulder surgery, a mechanical fluid-irrigation system is used to wash out blood from the joint. If used at high pressure, it can cause side effects such as fluid extravasation, leading to airway obstruction after surgery. Desflurane is prone to increasing sympathetic nerve activity and plasma catecholamine release more than another inhalation anesthetics. The objective of this study was to determine whether desflurane could increase in the irrigation pump pressure than sevoflurane in shoulder arthroscopy.
Methods
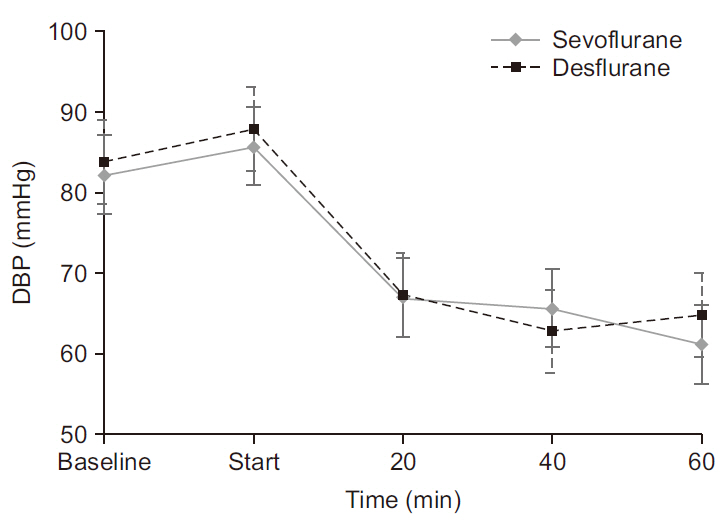
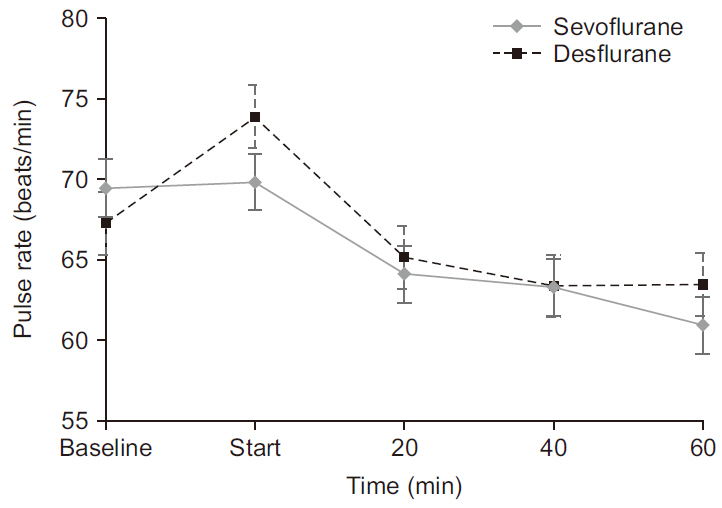
Patients were randomized into a sevoflurane group (group S) and a desflurane group (group D). Each included 20 patients. For group S, sevoflurane 1.2 MAC and intravenous remifentanil were administered for anesthesia maintenance. Group D received desflurane 1.2 MAC and intravenous remifentanil. Starting at 20 mmHg of pump pressure, the surgeon estimated the visibility of the surgical field (grade I–IV). After that, the pressure was freely adjusted by the surgeon to obtain clear vision with the arthroscope during the surgery.
Results
The maximum pressure of the mechanical water pump was higher in group D than group S (54.0 ± 6.8 mmHg vs. 48.9 ± 5.7 mmHg, P = 0.017), but the difference was not statistically significant at a significance level of 0.01. The arthroscopic visibility at the surgical site did not differ significantly between the two groups (P = 0.284).
Conclusions
When desflurane is used in arthroscopic shoulder surgery, it does not require more pressure from the irrigating-fluid pump to secure a clear vision of the surgical site, compared to sevoflurane.
Figure
Reference
-
Brülhart KB., Roggo A., Kossmann T., Duff C., Schimmer R., Glinz W. 1993. Arthroscopy of the shoulder joint. Technique, indications, surgery and complications. Langenbecks Arch Chir. 378:200–5. German. DOI: 10.1007/BF00184361. PMID: 8366732.Yamaguchi K., Levine WN., Marra G., Galatz LM., Klepps S., Flatow EL. 2003. Transitioning to arthroscopic rotator cuff repair: the pros and cons. Instr Course Lect. 52:81–92. DOI: 10.2106/00004623-200301000-00022. PMID: 12690842.Hsiao MS., Kusnezov N., Sieg RN., Owens BD., Herzog JP. 2016. Use of an irrigation pump system in arthroscopic procedures. Orthopedics. 39:e474–8. DOI: 10.3928/01477447-20160427-01. PMID: 27135450.Moen TC., Rudolph GH., Caswell K., Espinoza C., Burkhead WZ Jr., Krishnan SG. 2014. Complications of shoulder arthroscopy. J Am Acad Orthop Surg. 22:410–9. DOI: 10.5435/JAAOS-22-07-410. PMID: 24966247.Bomberg BC., Hurley PE., Clark CA., McLaughlin CS. 1992. Complications associated with the use of an infusion pump during knee arthroscopy. Arthroscopy. 8:224–8. DOI: 10.1016/0749-8063(92)90040-I. PMID: 1637436.Borgeat A., Bird P., Ekatodramis G., Dumont C. 2000. Tracheal compression caused by periarticular fluid accumulation: a rare complication of shoulder surgery. J Shoulder Elbow Surg. 9:443–5. DOI: 10.1067/mse.2000.109320. PMID: 11075331.Blumenthal S., Nadig M., Gerber C., Borgeat A. 2003. Severe airway obstruction during arthroscopic shoulder surgery. Anesthesiology. 99:1455–6. DOI: 10.1097/00000542-200312000-00033. PMID: 14639164.Saeki N., Kawamoto M. 2011. Tracheal obstruction caused by fluid extravasation during shoulder arthroscopy. Anaesth Intensive Care. 39:317–8. PMID: 21485693.Jakobsson J. 2012. Desflurane: a clinical update of a third-generation inhaled anaesthetic. Acta Anaesthesiol Scand. 56:420–32. DOI: 10.1111/j.1399-6576.2011.02600.x. PMID: 22188283.Leung JM., Pastor DA. 1998. Dissociation between haemodynamics and sympathetic activation during anaesthetic induction with desfluranes. Can J Anaesth. 45:533–40. DOI: 10.1007/BF03012703. PMID: 9669006.Marana E., Russo A., Colicci S., Polidori L., Bevilacqua F., Viviani D, et al. 2013. Desflurane versus sevoflurane: a comparison on stress response. Minerva Anestesiol. 79:7–14. PMID: 23090102.Bading B., Blank SG., Sculco TP., Pickering TG., Sharrock NE. 1994. Augmentation of calf blood flow by epinephrine infusion during lumbar epidural anesthesia. Anesth Analg. 78:1119–24. DOI: 10.1213/00000539-199406000-00015. PMID: 8198268.Freyschuss U., Hjemdahl P., Juhlin-Dannfelt A., Linde B. 1986. Cardiovascular and metabolic responses to low dose adrenaline infusion: an invasive study in humans. Clin Sci (Lond). 70:199–206. DOI: 10.1042/cs0700199. PMID: 3956110.van der Poll T T., Levi M., Dentener M., Jansen PM., Coyle SM., Braxton CC, et al. 1997. Epinephrine exerts anticoagulant effects during human endotoxemia. J Exp Med. 185:1143–8. DOI: 10.1084/jem.185.6.1143. PMID: 9091588. PMCID: PMC2196238.Ostrowski SR., Henriksen HH., Stensballe J., Gybel-Brask M., Cardenas JC., Baer LA, et al. 2017. Sympathoadrenal activation and endotheliopathy are drivers of hypocoagulability and hyperfibrinolysis in trauma: A prospective observational study of 404 severely injured patients. J Trauma Acute Care Surg. 82:293–301. DOI: 10.1097/TA.0000000000001304. PMID: 27779595.Zini C., Stieven-Filho E., Tabushi FI., Ribas CA., Ribas FM., Opolski AC, et al. 2016. Knee arthroscopic visibility alterations in obese and non-obese patients. Arq Bras Cir Dig. 29(Suppl 1):75–9. DOI: 10.1590/0102-6720201600s10019. PMID: 27683782. PMCID: PMC5064278.Johnson DS., Stewart H., Hirst P., Harper NJ. 2000. Is tourniquet use necessary for knee arthroscopy? Arthroscopy. 16:648–51. DOI: 10.1053/jars.2000.4826. PMID: 10976127.Matthews LS., Fadale PD. 1989. Subacromial anatomy for the arthroscopist. Arthroscopy. 5:36–40. DOI: 10.1016/0749-8063(89)90088-1. PMID: 2706049.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cerebrovascular reactivity to hypercapnia during sevoflurane or desflurane anesthesia in rats
- The hemodynamic changes during the infusion of remifentanil for patients under sevoflurane anesthesia during arthroscopic shoulder surgery
- The change of sevoflurane to desflurane after anesthesia induction induces rapid emergence without increased cardiovascular responses and emergence delirium in pediatric strabismus surgery patients
- Intramuscular Pressure of the Deltoid and the Efficacy of Cryotherapy in the Shoulder Arthroscopy
- Bispectral index and their relation with consciousness of the patients who receive desflurane or sevoflurane anesthesia during wake-up test for spinal surgery for correction