Clin Exp Otorhinolaryngol.
2020 May;13(2):157-163. 10.21053/ceo.2019.00836.
Clinical Characteristics Other Than Intralesional Hyperdensity May Increase the Preoperative Diagnostic Accuracy of Maxillary Sinus Fungal Ball
- Affiliations
-
- 1Department of Otorhinolaryngology-Head and Neck Surgery, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea
- 2Department of Otorhinolaryngology-Head and Neck Surgery, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
- 3Department of Radiology, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea
- KMID: 2500288
- DOI: http://doi.org/10.21053/ceo.2019.00836
Abstract
Objectives
. This study aimed to evaluate the clinical characteristics of maxillary sinus fungus ball (MFB) to increase the preoperative diagnostic accuracy.
Methods
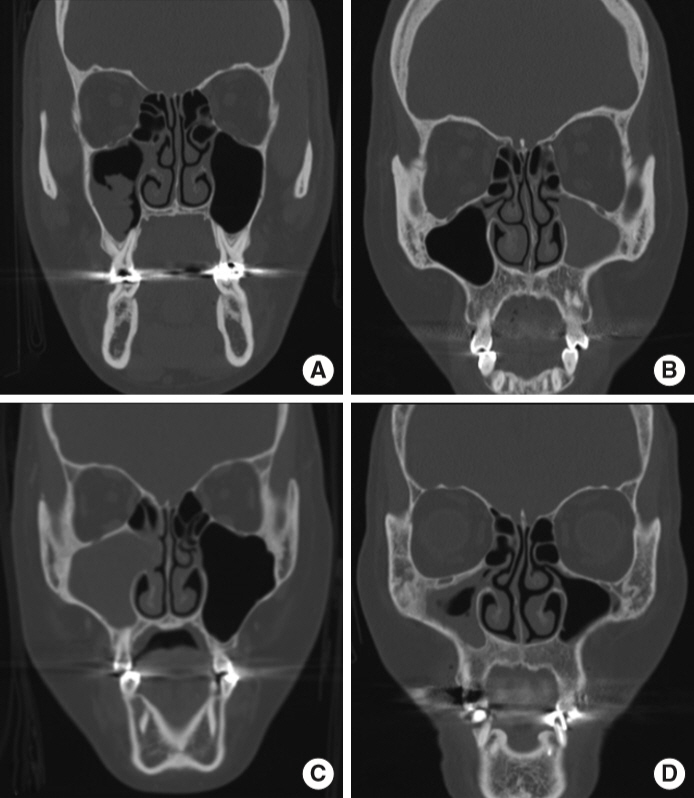
. A retrospective review of 247 patients who underwent endoscopic sinus surgery for unilateral maxillary sinusitis from January 2015 to December 2017 at a single institution was performed. Patients with pathologically proven MFB were compared to those with unilateral chronic maxillary sinusitis (CMS). Patient demographics and computed tomography (CT) findings were evaluated. The CT features were categorized as intralesional hyperdensity (calcification), the irregular lobulated protruding lesion (fuzzy appearance), maxillary sinus full haziness without mass effect, maxillary sinus full haziness with mass effect, and others. A regression tree analysis was performed.
Results
. In total, 247 patients were analyzed; among them, 179 (72.5%) had MFB and 68 (27.5%) had CMS. MFB showed predominance in older individuals. Among the radiological features, intralesional hyperdensity was most commonly associated with MFB. The presence of a fuzzy appearance or full opacity with mass effect was also associated with MFB. The highest area under the curve was noted with the regression tree analysis based on the model, which included the presence of intralesional hyperdensity, demographic data (age), and presence of fuzzy appearance or maxillary sinus full haziness with mass effect in case of absence of intralesional hyperdensity (0.904).
Conclusion
. A simple algorithm to optimize the preoperative diagnosis of MFB was developed. Physicians should be aware of such findings in the management of patients presenting with unilateral CMS.
Keyword
Figure
Cited by 3 articles
-
Unveiling the Diverse Spectrum of Fungal Rhinosinusitis
Seok Hyun Cho
Clin Exp Otorhinolaryngol. 2020;13(2):89-90. doi: 10.21053/ceo.2019.02026.Clinical Characteristics According to the Radiological Classifications of Maxillary Sinus Fungus Ball
Dong-Hyun Kim, Jung-Hun Kown, Hyung-Bon Koo, Jae-Hoon Lee
J Rhinol. 2022;29(1):32-37. doi: 10.18787/jr.2021.00392.Bacterial Ball in Concha Bullosa: Report of a Case With Unusual Location
Su-Jong Kim, Jee Won Moon, Yongmin Cho, Heung-Man Lee
Korean J Otorhinolaryngol-Head Neck Surg. 2023;66(5):335-339. doi: 10.3342/kjorl-hns.2021.01067.
Reference
-
1. Dufour X, Kauffmann-Lacroix C, Ferrie JC, Goujon JM, Rodier MH, Klossek JM. Paranasal sinus fungus ball: epidemiology, clinical features and diagnosis: a retrospective analysis of 173 cases from a single medical center in France, 1989-2002. Med Mycol. 2006; Feb. 44(1):61–7.
Article2. Jiang RS, Huang WC, Liang KL. Characteristics of sinus fungus ball: a unique form of rhinosinusitis. Clin Med Insights Ear Nose Throat. 2018; Aug. 11:1179550618792254.
Article3. Nomura K, Asaka D, Nakayama T, Okushi T, Matsuwaki Y, Yoshimura T, et al. Sinus fungus ball in the Japanese population: clinical and imaging characteristics of 104 cases. Int J Otolaryngol. 2013; 2013:731640.
Article4. Yoon YH, Xu J, Park SK, Heo JH, Kim YM, Rha KS. A retrospective analysis of 538 sinonasal fungus ball cases treated at a single tertiary medical center in Korea (1996-2015). Int Forum Allergy Rhinol. 2017; Nov. 7(11):1070–5.
Article5. deShazo RD, O’Brien M, Chapin K, Soto-Aguilar M, Swain R, Lyons M, et al. Criteria for the diagnosis of sinus mycetoma. J Allergy Clin Immunol. 1997; Apr. 99(4):475–85.
Article6. Chen JC, Ho CY. The significance of computed tomographic findings in the diagnosis of fungus ball in the paranasal sinuses. Am J Rhinol Allergy. 2012; Mar-Apr. 26(2):117–9.
Article7. Ho CF, Lee TJ, Wu PW, Huang CC, Chang PH, Huang YL, et al. Diagnosis of a maxillary sinus fungus ball without intralesional hyperdensity on computed tomography. Laryngoscope. 2019; May. 129(5):1041–5.
Article8. Dhong HJ, Jung JY, Park JH. Diagnostic accuracy in sinus fungus balls: CT scan and operative findings. Am J Rhinol. 2000; Jul-Aug. 14(4):227–31.
Article9. Seo YJ, Kim J, Kim K, Lee JG, Kim CH, Yoon JH. Radiologic characteristics of sinonasal fungus ball: an analysis of 119 cases. Acta Radiol. 2011; Sep. 52(7):790–5.
Article10. Klossek JM, Serrano E, Peloquin L, Percodani J, Fontanel JP, Pessey JJ. Functional endoscopic sinus surgery and 109 mycetomas of paranasal sinuses. Laryngoscope. 1997; Jan. 107(1):112–7.
Article11. McCarty JL, David RM, Lensing SY, Samant RS, Kumar M, Van Hemert RL, et al. Root cause analysis: an examination of odontogenic origins of acute maxillary sinusitis in both immunocompetent & immunocompromised patients. J Comput Assist Tomogr. 2017; May/Jun. 41(3):484–8.12. Smith TC, Frank E. Introducing machine learning concepts with WEKA. Methods Mol Biol. 2016; 1418:353–78.
Article13. Kim JS, So SS, Kwon SH. The increasing incidence of paranasal sinus fungus ball: a retrospective cohort study in two hundred forty-five patients for fifteen years. Clin Otolaryngol. 2017; Feb. 42(1):175–9.
Article14. Ferguson BJ. Fungus balls of the paranasal sinuses. Otolaryngol Clin North Am. 2000; Apr. 33(2):389–98.
Article15. Jiang Z, Zhang K, Huang W, Yuan Q. A preliminary study on sinus fungus ball with MicroCT and X-ray fluorescence technique. PLoS One. 2016; Mar. 11(3):e0148515.
Article16. Willinger B, Obradovic A, Selitsch B, Beck-Mannagetta J, Buzina W, Braun H, et al. Detection and identification of fungi from fungus balls of the maxillary sinus by molecular techniques. J Clin Microbiol. 2003; Feb. 41(2):581–5.
Article17. Wilson D, Citiulo F, Hube B. Zinc exploitation by pathogenic fungi. PLoS Pathog. 2012; Dec. 8(12):e1003034.
Article18. Eide DJ. Homeostatic and adaptive responses to zinc deficiency in Saccharomyces cerevisiae. J Biol Chem. 2009; Jul. 284(28):18565–9.
Article19. Zhu H, Zhang W, Guan J, Ye H, Su K. CT imaging and clinical features of sinus fungus ball with bone erosion. J Nat Sci. 2015; 1(4):e69.20. Ierodiakonou D, Postma DS, Koppelman GH, Boezen HM, Gerritsen J, Ten Hacken N, et al. E-cadherin gene polymorphisms in asthma patients using inhaled corticosteroids. Eur Respir J. 2011; Nov. 38(5):1044–52.
Article21. Robey AB, O’Brien EK, Richardson BE, Baker JJ, Poage DP, Leopold DA. The changing face of paranasal sinus fungus balls. Ann Otol Rhinol Laryngol. 2009; Jul. 118(7):500–5.
Article22. deShazo RD, Chapin K, Swain RE. Fungal sinusitis. N Engl J Med. 1997; Jul. 337(4):254–9.
Article23. deShazo RD. Fungal sinusitis. Am J Med Sci. 1998; Jul. 316(1):39–45.
Article24. Paz Silva M, Pinto JM, Corey JP, Mhoon EE, Baroody FM, Naclerio RM. Diagnostic algorithm for unilateral sinus disease: a 15-year retrospective review. Int Forum Allergy Rhinol. 2015; Jul. 5(7):590–6.25. Park GY, Kim HY, Min JY, Dhong HJ, Chung SK. Endodontic treatment: a significant risk factor for the development of maxillary fungal ball. Clin Exp Otorhinolaryngol. 2010; Sep. 3(3):136–40.
Article26. Tomazic PV, Dostal E, Magyar M, Lang-Loidolt D, Wolf A, Koele W, et al. Potential correlations of dentogenic factors to the development of clinically verified fungus balls: a retrospective computed tomography-based analysis. Laryngoscope. 2016; Jan. 126(1):39–43.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Actinomycosis of the Maxillary Sinus Accompanied with Fungal Ball
- A Case of Fungal Ball Caused by Retained Glass Foreign Body in Maxillary Sinus for 30 Years
- A Case of Fungal Ball Accompanied with a Microplate as Metallic Foreign Body in Maxillary Sinus
- Characteristic features of fungus ball in the maxillary sinus and the location of intralesional calcifications on computed tomographic images: A report of 2 cases
- Endodontic Treatment: A Significant Risk Factor for the Development of Maxillary Fungal Ball