Prevalence and Duration of Acute Loss of Smell or Taste in COVID-19 Patients
- Affiliations
-
- 1Daegu Medical Association, Daegu, Korea
- 2Department of Internal Medicine, School of Medicine, Kyungpook National University, Daegu, Korea
- KMID: 2500221
- DOI: http://doi.org/10.3346/jkms.2020.35.e174
Abstract
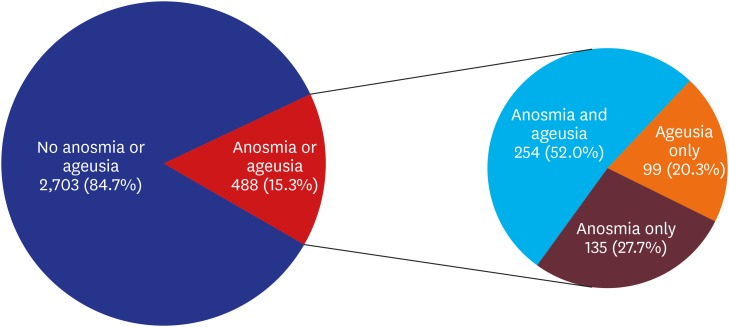
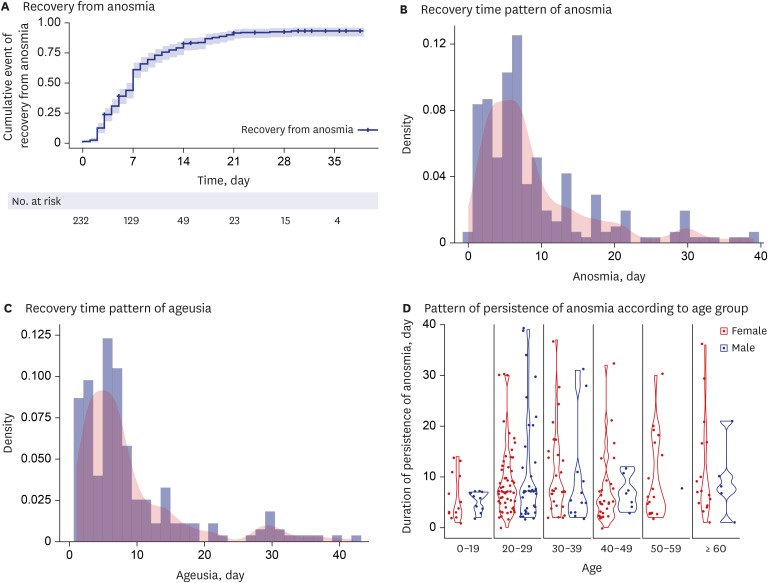
- Initially, acute loss of smell (anosmia) and taste (ageusia) was not considered important symptoms for coronavirus disease 2019 (COVID-19). To determine the prevalence of these symptoms and to evaluate their diagnostic significance, we (approximately 150 physicians of the Daegu Medical Association) prospectively collected data of cases of anosmia and ageusia from March 8, 2020, via telephone interview among 3,191 patients in Daegu, Korea. Acute anosmia or ageusia was observed in 15.3% (488/3,191) patients in the early stage of COVID-19 and in 15.7% (367/2,342) patients with asymptomatic-to-mild disease severity. Their prevalence was significantly more common among females and younger individuals (P = 0.01 and P < 0.001, respectively). Most patients with anosmia or ageusia recovered within 3 weeks. The median time to recovery was 7 days for both symptoms. Anosmia and ageusia seem to be part of important symptoms and clues for the diagnosis of COVID-19, particularly in the early stage of the disease.
Keyword
Figure
Cited by 12 articles
-
Olfactory and Gustatory Dysfunction in a COVID-19 Patient with Ankylosing Spondylitis Treated with Etanercept: Case Report
Jong-Mok Lee, Sang Jin Lee
J Korean Med Sci. 2020;35(21):e201. doi: 10.3346/jkms.2020.35.e201.Trend of Olfactory and Gustatory Dysfunction in COVID-19 Patients in a Quarantine Facility
Min Young Seo, Hyeri Seok, Sun Jin Hwang, Hee Kyoung Choi, Ji Hoon Jeon, Jang Wook Sohn, Dae Won Park, Seung Hoon Lee, Won Suk Choi
J Korean Med Sci. 2020;35(41):e375. doi: 10.3346/jkms.2020.35.e375.Coping with Dementia in the Middle of the COVID-19 Pandemic
Nayoung Ryoo, Jung-Min Pyun, Min Jae Baek, Jeewon Suh, Min Ju Kang, Min Jeong Wang, Young Chul Youn, Dong Won Yang, Seong Yoon Kim, Young Ho Park, SangYun Kim
J Korean Med Sci. 2020;35(42):e383. doi: 10.3346/jkms.2020.35.e383.Clinical Characteristics and Outcomes of COVID-19 Cohort Patients in Daegu Metropolitan City Outbreak in 2020
Shin-Woo Kim, Seung-Mee Kim, Yu Kyung Kim, Jong-yeon Kim, Yu-Mi Lee, Bong-Ok Kim, Suhyun Hwangbo, Taesung Park
J Korean Med Sci. 2020;36(1):e12. doi: 10.3346/jkms.2021.36.e12.Validation of Olfactory Questionnaire in Koreans: an Alternative for Conventional Psychophysical Olfactory Tests
Jeong-Whun Kim, Hyo sang Kim, Minju Kim, Su Hwan Kim, Sung-Woo Cho, Jin Youp Kim
J Korean Med Sci. 2021;36(6):e34. doi: 10.3346/jkms.2021.36.e34.Regional and Chronological Variation of Chemosensory Dysfunction in COVID-19: a Meta-Analysis
Jeong-Whun Kim, Seung Cheol Han, Hyung Dong Jo, Sung-Woo Cho, Jin Youp Kim
J Korean Med Sci. 2021;36(4):e40. doi: 10.3346/jkms.2021.36.e40.Analysis of PubMed and KoreaMed Indexed Korean Publications on COVID-19
Jong-Min Kim, Jin-Hong Yoo, Hae Kyung Cho, Sung-Tae Hong
J Korean Med Sci. 2021;36(49):e345. doi: 10.3346/jkms.2021.36.e345.Characteristics and Prognosis of COVID-19 Induced Olfactory and Gustatory Dysfunction in Daegu
Sung Jae Heo, Tae Hoon Kim, Seung-Heon Shin, Mi-Kyung Ye
Korean J Otorhinolaryngol-Head Neck Surg. 2021;64(10):720-725. doi: 10.3342/kjorl-hns.2020.00948.COVID-19 and Smell Loss
Joon Kon Kim, Doo Hee Han
Korean J Otorhinolaryngol-Head Neck Surg. 2020;63(11):491-496. doi: 10.3342/kjorl-hns.2020.01039.Novel respiratory infectious diseases in Korea
Hyun Jung Kim
Yeungnam Univ J Med. 2020;37(4):286-295. doi: 10.12701/yujm.2020.00633.Effects of Air Pollution on Chemosensory Dysfunction in COVID-19 Patients
Young-Sook Choi, Byeong-Su Jeong, Yeon-Kyeng Lee, Yong-Dae Kim
J Korean Med Sci. 2022;37(39):e290. doi: 10.3346/jkms.2022.37.e290.Comparative Analysis of Olfactory and Gustatory Function of Patients With COVID-19 Olfactory Dysfunction and Non-COVID-19 Postinfectious Olfactory Dysfunction
Taesik Jung, Bo Yoon Choi, Minho Jang, Taehee Kim, EunHye Seo, Jin Kook Kim
J Korean Med Sci. 2023;38(43):e352. doi: 10.3346/jkms.2023.38.e352.
Reference
-
1. Kim SW, Lee KS, Kim K, Lee JJ, Kim JY, Association DM; Daegu Medical Association. A brief telephone severity scoring system and therapeutic living centers solved acute hospital-bed shortage during the COVID-19 outbreak in Daegu, Korea. J Korean Med Sci. 2020; 35(15):e152. PMID: 32301298.
Article2. van Riel D, Verdijk R, Kuiken T. The olfactory nerve: a shortcut for influenza and other viral diseases into the central nervous system. J Pathol. 2015; 235(2):277–287. PMID: 25294743.
Article3. Hummel T, Landis BN, Hüttenbrink KB. Smell and taste disorders. GMS Curr Top Otorhinolaryngol Head Neck Surg. 2011; 10:Doc04. PMID: 22558054.4. Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020; 8(5):S2213-2600(20)30079-5.
Article5. Novel Coronavirus Pneumonia Emergency Response Epidemiology Team. The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China. Zhonghua Liu Xing Bing Xue Za Zhi. 2020; 41(2):145–151. PMID: 32064853.6. Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020; 395(10223):507–513. PMID: 32007143.
Article7. Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020; 382(18):1708–1720. PMID: 32109013.8. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020; 395(10223):497–506. PMID: 31986264.
Article9. Kim ES, Chin BS, Kang CK, Kim NJ, Kang YM, Choi JP, et al. Clinical course and outcomes of patients with severe acute respiratory syndrome coronavirus 2 infection: a preliminary report of the first 28 patients from the Korean Cohort Study on COVID-19. J Korean Med Sci. 2020; 35(13):e142. PMID: 32242348.
Article10. Lechien JR, Chiesa-Estomba CM, De Siati DR, Horoi M, Le Bon SD, Rodriguez A, et al. Olfactory and gustatory dysfunctions as a clinical presentation of mild-to-moderate forms of the coronavirus disease (COVID-19): a multicenter European study. Eur Arch Otorhinolaryngol. Forthcoming 2020.
Article11. Giacomelli A, Pezzati L, Conti F, Bernacchia D, Siano M, Oreni L, et al. Self-reported olfactory and taste disorders in SARS-CoV-2 patients: a cross-sectional study. Clin Infect Dis. Forthcoming 2020.12. Eliezer M, Hautefort C, Hamel AL, Verillaud B, Herman P, Houdart E, et al. Sudden and complete olfactory loss function as a possible symptom of COVID-19. JAMA Otolaryngol Head Neck Surg. Forthcoming 2020.13. Jang Y, Son HJ, Lee S, Lee EJ, Kim TH, Park SY. Olfactory and taste disorder: the first and only sign in a patient with SARS-CoV-2 pneumonia. Infect Control Hosp Epidemiol. Forthcoming 2020.
Article14. Netland J, Meyerholz DK, Moore S, Cassell M, Perlman S. Severe acute respiratory syndrome coronavirus infection causes neuronal death in the absence of encephalitis in mice transgenic for human ACE2. J Virol. 2008; 82(15):7264–7275. PMID: 18495771.
Article15. Xu H, Zhong L, Deng J, Peng J, Dan H, Zeng X, et al. High expression of ACE2 receptor of 2019-nCoV on the epithelial cells of oral mucosa. Int J Oral Sci. 2020; 12(1):8. PMID: 32094336.
Article16. Cheng HY, Jian SW, Liu DP, Ng TC, Huang WT, Lin HH, et al. Contact tracing assessment of COVID-19 transmission dynamics in Taiwan and risk at different exposure periods before and after symptom onset. JAMA Intern Med. Forthcoming 2020.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- COVID-19 and Smell Loss
- Taste and Smell Disturbances in Patients with Gastroparesis and Gastroesophageal Reflux Disease
- Comparative Analysis of Olfactory and Gustatory Function of Patients With COVID-19 Olfactory Dysfunction and Non-COVID-19 Postinfectious Olfactory Dysfunction
- Symptoms and Characteristics Which Require Attention During COVID-19 Screening at a Port of Entry
- Clinical Investigations in Patients with Taste Disorder