J Korean Med Sci.
2020 Apr;35(18):e117. 10.3346/jkms.2020.35.e117.
Comparisons of Clinical Outcomes between Weekday-Only and Full-Time, 24-Hour/7-Day Coverage HospitalistSystems
- Affiliations
-
- 1Department of Internal Medicine, Seoul National University Hospital, Seoul, Korea
- 2Cancer Research Institute, Seoul National University College of Medicine, Seoul, Korea
- 3Department of Internal Medicine and Liver Research Institute, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2500216
- DOI: http://doi.org/10.3346/jkms.2020.35.e117
Abstract
- Background
Since the launch of pilot programs in 2016, varying ranges of hospitalist coverage exist in Korea. We evaluated the effects of differing depths of hospitalist coverage on clinical outcomes.
Methods
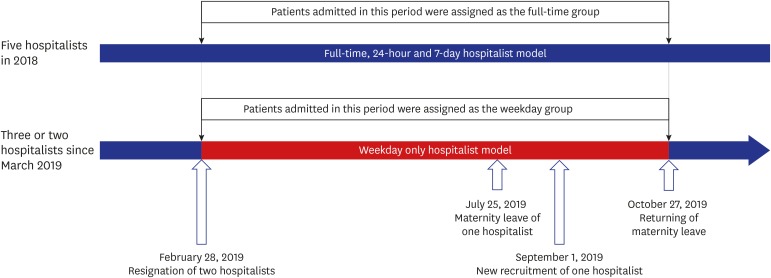
This study retrospectively reviewed the records of 513 patients admitted to a medical hospitalist unit through emergency department at Seoul National University Hospital. The full-time group included patients admitted in 2018 who received 24/7 hospitalist service, whereas the weekday group included patients admitted in 2019 with only weekday hospitalist service. In-hospital clinical outcomes were compared between the two groups.
Results
Unplanned intensive care unit admission rate was lower in the full-time group than in the weekday group (0.4% vs. 2.9%; P = 0.042). Discharges to local hospitals for subacute or chronic care were more frequent in the full-time group than in the weekday group (12.6% vs. 5.8%; P = 0.007). The weekday coverage was a predictive factor of in-ward mortality (odds ratio, 2.00; 95% confidence interval, 1.01–3.99) after adjusting for potential confounding factors.
Conclusion
Uninterrupted weekend coverage hospitalist service is helpful for care-plan decision and timely care transitions for acutely and severely ill patients.
Keyword
Figure
Reference
-
1. Wachter RM. An introduction to the hospitalist model. Ann Intern Med. 1999; 130(4 Pt 2):338–342. PMID: 10068402.
Article2. Diamond HS, Goldberg E, Janosky JE. The effect of full-time faculty hospitalists on the efficiency of care at a community teaching hospital. Ann Intern Med. 1998; 129(3):197–203. PMID: 9696727.
Article3. Salim SA, Elmaraezy A, Pamarthy A, Thongprayoon C, Cheungpasitporn W, Palabindala V. Impact of hospitalists on the efficiency of inpatient care and patient satisfaction: a systematic review and meta-analysis. J Community Hosp Intern Med Perspect. 2019; 9(2):121–134. PMID: 31044043.
Article4. Wachter RM, Goldman L. Zero to 50,000 - the 20th anniversary of the hospitalist. N Engl J Med. 2016; 375(11):1009–1011. PMID: 27508924.
Article5. Jeon B, Kwon S. Health and long-term care systems for older people in the republic of Korea: policy challenges and lessons. Health Syst Reform. 2017; 3(3):214–223. PMID: 31514668.
Article6. Jang SI, Jang SY, Park EC. Trends of US hospitalist and suggestions for introduction of Korean hospitalist. Korean J Med. 2015; 89(1):1–5.
Article7. Eom JS. Operating the hospitalist system. J Korean Med Assoc. 2016; 59(5):342–344.
Article8. Kim J. The impact of hospitalist care in Korea. J Korean Med Sci. 2019; 34(25):e177. PMID: 31243936.
Article9. Ohn JH, Kim NH, Kim ES, Baek SH, Lim Y, Hur J, et al. An acute medical unit in a Korean tertiary care hospital reduces the length of stay and waiting time in the emergency department. J Korean Med Sci. 2017; 32(12):1917–1920. PMID: 29115071.
Article10. Lee JH, Kim AJ, Kyong TY, Jang JH, Park J, Lee JH, et al. Evaluating the outcome of multi-morbid patients cared for by hospitalists: a report of integrated medical model in Korea. J Korean Med Sci. 2019; 34(25):e179. PMID: 31243937.
Article11. Kim HW. The current status of hospital medicine in Korea, 2019. Korean J Med. 2019; 94(2):139–144.
Article12. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987; 40(5):373–383. PMID: 3558716.
Article13. Korean Health Insurance Review and Assessment Service. News & notice. Updated 2017. Accessed October 22, 2019. http://www.hira.or.kr/bbsDummy.do?pgmid=HIRAA020002000100.14. Goodwin JS, Li S, Kuo YF. Association of the work schedules of hospitalists with patient outcomes of hospitalization. JAMA Intern Med. 2020; 180(2):215–222.
Article15. You JJ, Downar J, Fowler RA, Lamontagne F, Ma IW, Jayaraman D, et al. Barriers to goals of care discussions with seriously ill hospitalized patients and their families: a multicenter survey of clinicians. JAMA Intern Med. 2015; 175(4):549–556. PMID: 25642797.16. Gott M, Ingleton C, Bennett MI, Gardiner C. Transitions to palliative care in acute hospitals in England: qualitative study. BMJ Support Palliat Care. 2011; 1(1):42–48.
Article17. Auerbach AD, Pantilat SZ. End-of-life care in a voluntary hospitalist model: effects on communication, processes of care, and patient symptoms. Am J Med. 2004; 116(10):669–675. PMID: 15121493.
Article18. Blecker S, Goldfeld K, Park H, Radford MJ, Munson S, Francois F, et al. Impact of an intervention to improve weekend hospital care at an academic medical center: an observational study. J Gen Intern Med. 2015; 30(11):1657–1664. PMID: 25947881.
Article19. Blecker S, Shine D, Park N, Goldfeld K, Scott Braithwaite R, Radford MJ, et al. Association of weekend continuity of care with hospital length of stay. Int J Qual Health Care. 2014; 26(5):530–537. PMID: 24994844.
Article20. van Walraven C. The influence of inpatient physician continuity on hospital discharge. J Gen Intern Med. 2019; 34(9):1709–1714. PMID: 31197735.
Article21. Epstein K, Juarez E, Epstein A, Loya K, Singer A. The impact of fragmentation of hospitalist care on length of stay. J Hosp Med. 2010; 5(6):335–338. PMID: 20803671.
Article22. Arabi Y, Alshimemeri A, Taher S. Weekend and weeknight admissions have the same outcome of weekday admissions to an intensive care unit with onsite intensivist coverage. Crit Care Med. 2006; 34(3):605–611. PMID: 16521254.
Article23. Gajic O, Afessa B, Hanson AC, Krpata T, Yilmaz M, Mohamed SF, et al. Effect of 24-hour mandatory versus on-demand critical care specialist presence on quality of care and family and provider satisfaction in the intensive care unit of a teaching hospital. Crit Care Med. 2008; 36(1):36–44. PMID: 18007270.
Article24. Nishisaki A, Pines JM, Lin R, Helfaer MA, Berg RA, Tenhave T, et al. The impact of 24-hr, in-hospital pediatric critical care attending physician presence on process of care and patient outcomes. Crit Care Med. 2012; 40(7):2190–2195. PMID: 22564956.
Article25. Vinh KP, Walston SL, Szychowski J, Hernandez SR. The effect of hospitalists on average length of stay. J Healthc Manag. 2019; 64(3):169–184. PMID: 31999267.
Article26. Lucas BP, Trick WE, Evans AT, Mba B, Smith J, Das K, et al. Effects of 2- vs 4-week attending physician inpatient rotations on unplanned patient revisits, evaluations by trainees, and attending physician burnout: a randomized trial. JAMA. 2012; 308(21):2199–2207. PMID: 23212497.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Characteristics of Sleep Pattern among Korean College Students
- Comparison of food and nutrient intake between weekday and weekend for elementary and middle school students by gender in Busan and some parts of Kyungsangnamdo
- A Study on Food and Nutrient Intakes of Weekday and Weekend Among High School Boys in Seoul
- 24-hour urine sodium excretion among renal donors in India: a cross-sectional study
- A study on Performing Time of Neurobehavioral Test in Workers exposed to Organic Solvents