J Korean Med Sci.
2020 Apr;35(17):e115. 10.3346/jkms.2020.35.e115.
Prevalence and Incidence of Neuromyelitis Optica Spectrum Disorderin Korea: Population Based Study
- Affiliations
-
- 1Department of Neurology, Korea University College of Medicine, Seoul, Korea
- 2Department of Digital Healthcare, Samsung Advanced Institute for Health Sciences & Technology, Seoul, Korea
- 3Department of Neurology, Soonchunhyang University Cheonan Hospital, Soonchunhyang University College of Medicine, Cheonan, Korea
- 4Department of Neurology, Seoul Metropolitan Government-Seoul National University Boramae Medical Center, Seoul National University College of Medicine, Seoul, Korea
- 5Department of Medical Administration and Information, Daejeon Health Institute of Technology, Daejeon, Korea
- 6Department of Neurology, Yonsei University College of Medicine, Seoul, Korea
- 7Department of Biostatistics, Korea University College of Medicine, Seoul, Korea
- 8Department of Neurology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 9Neuroscience Center, Samsung Medical Center, Seoul, Korea
- KMID: 2500208
- DOI: http://doi.org/10.3346/jkms.2020.35.e115
Abstract
- Background
Although neuromyelitis optica spectrum disorder (NMOSD) is known to be a rare disease, its prevalence and incidence have not yet been studied in Korea. We performed a population-based study to examine the prevalence and incidence of NMOSD in Korea using data from the Korean National Health Insurance (NHI) claims database.
Methods
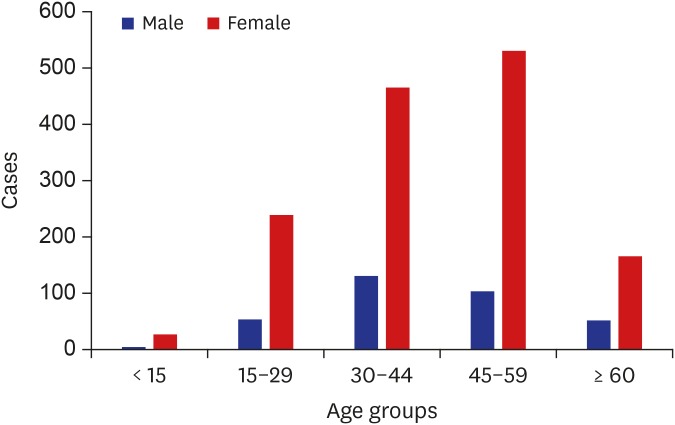
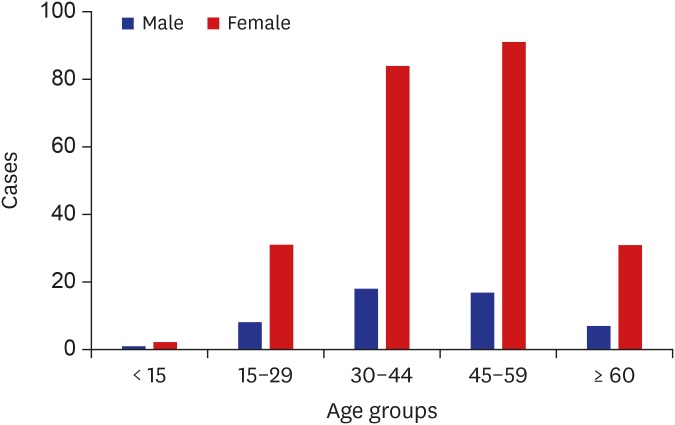
Data from 2013 to 2017 were obtained, with a washout period set as 2013 and 2014. The prevalence and incidence of NMOSD in 2016 and 2017 were calculated using population census data. Subjects were divided into 5 groups at 15-year intervals, depending on the age at which the diagnostic code was entered. The relative risk (RR) for each age group was compared with the oldest (≥ 60 years) age group.
Results
The overall prevalence was estimated to be 3.36 and 3.56 per 100,000 individuals, with an incidence of 0.41 and 0.65 per 100,000 individuals-year in 2016 and 2017, respectively. The mean age was 43.08 (standard deviation, 14.56) years, and the ratio of male to females was 1:4.7. The incidence was higher in female individuals aged between 30 and 59 years (RR, 2.8–3.05; P < 0.05).
Conclusion
Nationwide prevalence of NMOSD in Korea was 3.36 and 3.56/100,000 and its incidence was 0.41 and 0.65/100,000-year in 2016 and 2017 respectively.
Figure
Reference
-
1. Kitley J, Waters P, Woodhall M, Leite MI, Murchison A, George J, et al. Neuromyelitis optica spectrum disorders with aquaporin-4 and myelin-oligodendrocyte glycoprotein antibodies: a comparative study. JAMA Neurol. 2014; 71(3):276–283. PMID: 24425068.2. Cabre P. Environmental changes and epidemiology of multiple sclerosis in the French West Indies. J Neurol Sci. 2009; 286(1-2):58–61. PMID: 19520388.
Article3. Cabrera-Gómez JA, Kurtzke JF, González-Quevedo A, Lara-Rodríguez R. An epidemiological study of neuromyelitis optica in Cuba. J Neurol. 2009; 256(1):35–44. PMID: 19224310.
Article4. Jacob A, Panicker J, Lythgoe D, Elsone L, Mutch K, Wilson M, et al. The epidemiology of neuromyelitis optica amongst adults in the Merseyside county of United Kingdom. J Neurol. 2013; 260(8):2134–2137. PMID: 23689970.
Article5. Flanagan EP, Cabre P, Weinshenker BG, Sauver JS, Jacobson DJ, Majed M, et al. Epidemiology of aquaporin-4 autoimmunity and neuromyelitis optica spectrum. Ann Neurol. 2016; 79(5):775–783. PMID: 26891082.
Article6. Ashtari F, Safaei A, Shaygannejad V, Najafi MA, Vesal S. Neuromyelitis optica spectrum disease characteristics in Isfahan, Iran: a cross-sectional study. J Res Med Sci. 2017; 22:41. PMID: 28465700.
Article7. Hor JY, Lim TT, Chia YK, Ching YM, Cheah CF, Tan K, et al. Prevalence of neuromyelitis optica spectrum disorder in the multi-ethnic Penang Island, Malaysia, and a review of worldwide prevalence. Mult Scler Relat Disord. 2018; 19:20–24. PMID: 29100047.
Article8. Cossburn M, Tackley G, Baker K, Ingram G, Burtonwood M, Malik G, et al. The prevalence of neuromyelitis optica in South East Wales. Eur J Neurol. 2012; 19(4):655–659. PMID: 21967235.
Article9. Asgari N. Epidemiological, clinical and immunological aspects of neuromyelitis optica (NMO). Dan Med J. 2013; 60(10):B4730. PMID: 24083534.10. Kim SH, Mealy MA, Levy M, Schmidt F, Ruprecht K, Paul F, et al. Racial differences in neuromyelitis optica spectrum disorder. Neurology. 2018; 91(22):e2089–99. PMID: 30366977.
Article11. Bukhari W, Prain KM, Waters P, Woodhall M, O'Gorman CM, Clarke L, et al. Incidence and prevalence of NMOSD in Australia and New Zealand. J Neurol Neurosurg Psychiatry. 2017; 88(8):632–638. PMID: 28550069.12. Pandit L, Asgari N, Apiwattanakul M, Palace J, Paul F, Leite MI, et al. Demographic and clinical features of neuromyelitis optica: a review. Mult Scler. 2015; 21(7):845–853. PMID: 25921037.
Article13. Etemadifar M, Dashti M, Vosoughi R, Abtahi SH, Ramagopalan SV, Nasr Z. An epidemiological study of neuromyelitis optica in Isfahan. Mult Scler. 2014; 20(14):1920–1922. PMID: 24948686.
Article14. Marrie RA, Gryba C. The incidence and prevalence of neuromyelitis optica: a systematic review. Int J MS Care. 2013; 15(3):113–118. PMID: 24453773.15. Mealy MA, Wingerchuk DM, Greenberg BM, Levy M. Epidemiology of neuromyelitis optica in the United States: a multicenter analysis. Arch Neurol. 2012; 69(9):1176–1180. PMID: 22733096.
Article16. Houzen H, Kondo K, Niino M, Horiuchi K, Takahashi T, Nakashima I, et al. Prevalence and clinical features of neuromyelitis optica spectrum disorders in northern Japan. Neurology. 2017; 89(19):1995–2001. PMID: 28986408.
Article17. Miyamoto K, Fujihara K, Kira J, Kuriyama N, Matsui M, Tamakoshi A, et al. The prevalence and characteristics of neuromyelitis optica in Japan: a nationwide epidemiological study. J Neurol Sci. 2017; 381:787.
Article18. Cabre P, Heinzlef O, Merle H, Buisson GG, Bera O, Bellance R, et al. MS and neuromyelitis optica in Martinique (French West Indies). Neurology. 2001; 56(4):507–514. PMID: 11222796.
Article19. Kim NH, Kim HJ, Cheong HK, Kim BJ, Lee KH, Kim EH, et al. Prevalence of multiple sclerosis in Korea. Neurology. 2010; 75(16):1432–1438. PMID: 20956788.
Article20. Kim JE, Park SH, Han K, Kim HJ, Shin DW, Kim SM. Prevalence and incidence of neuromyelitis optica spectrum disorder and multiple sclerosis in Korea. Mult Scler. 2019; DOI: 10.1177/1352458519888609.
Article21. Langer-Gould A, Zhang JL, Chung J, Yeung Y, Waubant E, Yao J. Incidence of acquired CNS demyelinating syndromes in a multiethnic cohort of children. Neurology. 2011; 77(12):1143–1148. PMID: 21865580.
Article22. Cho GJ, Park HT, Shin JH, Hur JY, Kim YT, Kim SH, et al. Age at menarche in a Korean population: secular trends and influencing factors. Eur J Pediatr. 2010; 169(1):89–94. PMID: 19504269.
Article23. Park CY, Lim JY, Park HY. Age at natural menopause in Koreans: secular trends and influences thereon. Menopause. 2018; 25(4):423–429. PMID: 29112598.
Article24. Kim SM, Waters P, Woodhall M, Kim YJ, Kim JA, Cheon SY, et al. Gender effect on neuromyelitis optica spectrum disorder with aquaporin4-immunoglobulin G. Mult Scler. 2017; 23(8):1104–1111. PMID: 27760862.
Article25. Lee MH, Kim SH, Oh M, Lee KW, Park MJ. Age at menarche in Korean adolescents: trends and influencing factors. Reprod Health. 2016; 13(1):121. PMID: 27662834.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Postpartum Relapse of Neuromyelitis Optica Spectrum Disorder after a Long Period of Spontaneous Remission
- Neuromyelitis Optica Spectrum Disorder Presenting with Pseudoathetosis
- Differential Diagnosis between Multiple Sclerosis and Neuromyelitis Optica Spectrum Disorder
- Isolated Tongue Paralysis as Presentation of Seropositive Neuromyelitis Optica Spectrum Disorder
- Neuromyelitis Optica Spectrum Disorder Presented with Acute Memory Loss