J Korean Med Sci.
2020 Apr;35(16):e108. 10.3346/jkms.2020.35.e108.
Association between Cardiac Arrest Time and Favorable Neurological Outcomes in Witnessed Out-of-Hospital Cardiac Arrest Patients Treated with Targeted Temperature Management
- Affiliations
-
- 1Department of Emergency Medicine, Samsung Changwon Hospital, Sungkyunkwan University School of Medicine, Changwon, Korea
- 2Department of Physical Education, Kyungnam University, Changwon, Korea
- KMID: 2500201
- DOI: http://doi.org/10.3346/jkms.2020.35.e108
Abstract
- Background
Patients who achieve a return of spontaneous circulation (ROSC) with prolonged cardiac arrest have been recognized to have a poor prognosis. This might lead to reluctance in the provision of post-resuscitation care. Hence, we evaluated the impact of cardiac arrest time on neurologic outcomes in out-of-hospital cardiac arrest (OHCA) patients.
Methods
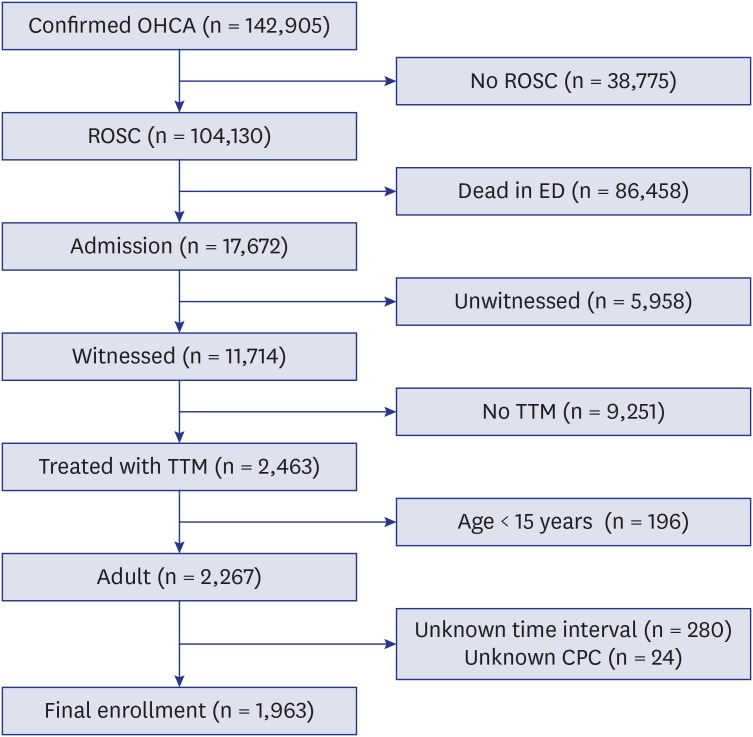
This cross-sectional study used a hospital-based nationwide registry of OHCAs in Korea between 2012 and 2016. All witnessed OHCA patients aged ≥ 15 years and treated with targeted temperature management were included. We collected the time from collapse to sustained ROSC, which was defined as the downtime. The primary outcome was a favorable neurological outcome at hospital discharge. A multiple logistic regression analysis was conducted to determine independent factors for primary outcome in patients with downtime > 30 minutes.
Results
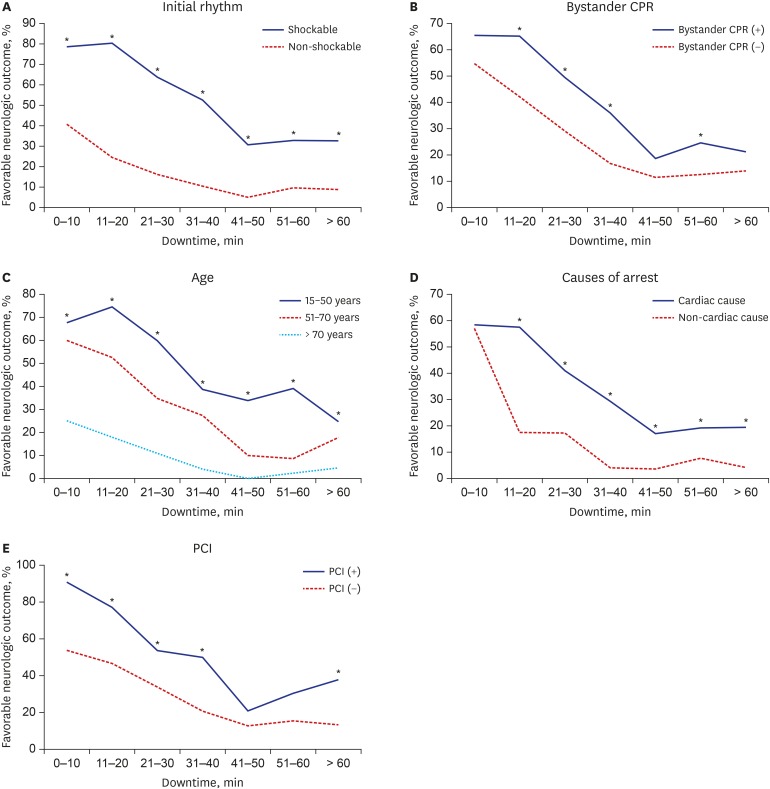
Overall, neurologically favorable outcome rates were 30.5% in 1,963 patients. When the downtime was stratified into categories of 0–10, 11–20, 21–30, 31–40, 41–50, 51–60, and > 60 minutes according to 10-minute intervals, neurologically favorable outcome rates were 58.2%, 52.3%, 37.3%, 24.6%, 14.1%, 17.4%, and 16.7%, respectively (P < 0.001). In patients with downtime > 30 minutes, age 51–70 years (odds ratio [OR], 5.35; 95% confidence interval [CI], 2.50–11.49), age ≤ 50 years (OR, 13.16; 95% CI, 6.06–28.57), shockable rhythm (OR, 3.92; 95% CI, 2.71–5.68), bystander resuscitation (OR, 1.80; 95% CI, 1.27–2.55), cardiac cause (OR, 3.50; 95% CI, 1.69–7.25), percutaneous coronary intervention (OR, 1.82; 95% CI, 1.18–2.81), and downtime ≤ 40 minutes (OR, 2.02; 95% CI, 1.42–2.88) were associated with favorable neurological outcomes.
Conclusion
In patients with prolonged downtime, predicting favorable neurologic outcome may be multifactorial. The cutoff value for downtime is not the only determining factor to provide post-resuscitation care.
Figure
Reference
-
1. Choi SW, Shin SD, Ro YS, Song KJ, Lee EJ, Ahn KO. Effect of therapeutic hypothermia on the outcomes after out-of-hospital cardiac arrest according to initial ECG rhythm and witnessed status: a nationwide observational interaction analysis. Resuscitation. 2016; 100:51–59. PMID: 26774175.
Article2. Yoon H, Kwon Y, An J, Hong S, Kim YT. Main outcomes of the sudden cardiac arrest survey 2006 to 2016. Clin Exp Emerg Med. 2019; 6(2):183–188. PMID: 31261487.
Article3. Hwang SO, Chung SP, Song KJ, Kim H, Rho TH, Park KN, et al. Part 1. The update process and highlights: 2015 Korean Guidelines for Cardiopulmonary Resuscitation. Clin Exp Emerg Med. 2016; 3(Suppl):S1–S9. PMID: 27752641.
Article4. Kim WY, Giberson TA, Uber A, Berg K, Cocchi MN, Donnino MW. Neurologic outcome in comatose patients resuscitated from out-of-hospital cardiac arrest with prolonged downtime and treated with therapeutic hypothermia. Resuscitation. 2014; 85(8):1042–1046. PMID: 24746783.
Article5. Kim WY, Ahn S, Hong JS, Cho GC, Seo DW, Jeung KW, et al. The impact of downtime on neurologic intact survival in patients with targeted temperature management after out-of-hospital cardiac arrest: National multicenter cohort study. Resuscitation. 2016; 105:203–208. PMID: 27060537.
Article6. Soga T, Nagao K, Sawano H, Yokoyama H, Tahara Y, Hase M, et al. Neurological benefit of therapeutic hypothermia following return of spontaneous circulation for out-of-hospital non-shockable cardiac arrest. Circ J. 2012; 76(11):2579–2585. PMID: 22813874.
Article7. Kjaergaard J, Nielsen N, Winther-Jensen M, Wanscher M, Pellis T, Kuiper M, et al. Impact of time to return of spontaneous circulation on neuroprotective effect of targeted temperature management at 33 or 36 degrees in comatose survivors of out-of hospital cardiac arrest. Resuscitation. 2015; 96:310–316. PMID: 26159609.
Article8. Camp-Rogers TR, Sawyer KN, McNicol DR, Kurz MC. An observational study of patient selection criteria for post-cardiac arrest therapeutic hypothermia. Resuscitation. 2013; 84(11):1536–1539. PMID: 23916552.
Article9. Ahn S, Lee BK, Youn CS, Kim YJ, Sohn CH, Seo DW, et al. Predictors of good neurologic outcome after resuscitation beyond 30 min in out-of-hospital cardiac arrest patients undergoing therapeutic hypothermia. Intern Emerg Med. 2018; 13(3):413–419. PMID: 28389857.10. Out-of-Hospital Cardiac Arrest Surveillance. Updated 2012. Accessed October 24, 2019. http://www.cdc.go.kr/board.es?mid=a20507020000&bid=0019&act=view&list_no=138037.11. Jeong J, Ro YS, Shin SD, Song KJ, Hong KJ, Ahn KO. Association of time from arrest to percutaneous coronary intervention with survival outcomes after out-of-hospital cardiac arrest. Resuscitation. 2017; 115:148–154. PMID: 28427881.
Article12. Kim MJ, Shin SD, McClellan WM, McNally B, Ro YS, Song KJ, et al. Neurological prognostication by gender in out-of-hospital cardiac arrest patients receiving hypothermia treatment. Resuscitation. 2014; 85(12):1732–1738. PMID: 25281187.
Article13. Kim KH, Shin SD, Song KJ, Ro YS, Kim YJ, Hong KJ, et al. Cooling methods of targeted temperature management and neurological recovery after out-of-hospital cardiac arrest: A nationwide multicenter multi-level analysis. Resuscitation. 2018; 125:56–65. PMID: 29409768.
Article14. Booth CM, Boone RH, Tomlinson G, Detsky AS. Is this patient dead, vegetative, or severely neurologically impaired? Assessing outcome for comatose survivors of cardiac arrest. JAMA. 2004; 291(7):870–879. PMID: 14970067.15. Lascarrou JB, Merdji H, Le Gouge A, Colin G, Grillet G, Girardie P, et al. Targeted temperature management for cardiac arrest with nonshockable rhythm. N Engl J Med. 2019; 381(24):2327–2337. PMID: 31577396.
Article16. Saarinen S, Castrén M, Virkkunen I, Kämäräinen A. Post resuscitation care of out-of-hospital cardiac arrest patients in the Nordic countries: a questionnaire study. Scand J Trauma Resusc Emerg Med. 2015; 23(1):60. PMID: 26353797.
Article17. Bailey ED, Wydro GC, Cone DC. National Association of EMS Physicians Standards and Clinical Practice Committee. Termination of resuscitation in the prehospital setting for adult patients suffering nontraumatic cardiac arrest. Prehosp Emerg Care. 2000; 4(2):190–195. PMID: 10782611.18. Nagao K, Nonogi H, Yonemoto N, Gaieski DF, Ito N, Takayama M, et al. Duration of prehospital resuscitation efforts after out-of-hospital cardiac arrest. Circulation. 2016; 133(14):1386–1396. PMID: 26920493.
Article19. Neumar RW, Otto CW, Link MS, Kronick SL, Shuster M, Callaway CW, et al. Part 8: adult advanced cardiovascular life support: 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2010; 122(18):Suppl 3. S729–S767. PMID: 20956224.
Article20. Atkins DL. Doing the same thing over and over, yet expecting different results. Circulation. 2013; 128(23):2465–2467. PMID: 24135072.
Article21. Reynolds JC, Grunau BE, Rittenberger JC, Sawyer KN, Kurz MC, Callaway CW. Association between duration of resuscitation and favorable outcome after out-of-hospital cardiac arrest: implications for prolonging or terminating resuscitation. Circulation. 2016; 134(25):2084–2094. PMID: 27760796.22. Terman SW, Shields TA, Hume B, Silbergleit R. The influence of age and chronic medical conditions on neurological outcomes in out of hospital cardiac arrest. Resuscitation. 2015; 89:169–176. PMID: 25640799.
Article23. Segal N, di Pompéo C, Escutnaire J, Wiel E, Dumont C, Castra L, et al. Evolution of survival in cardiac arrest with age in elderly patients: is resuscitation a dead end? J Emerg Med. 2018; 54(3):295–301. PMID: 29273461.
Article24. Kitamura T, Kiyohara K, Sakai T, Iwami T, Nishiyama C, Kajino K, et al. Epidemiology and outcome of adult out-of-hospital cardiac arrest of non-cardiac origin in Osaka: a population-based study. BMJ Open. 2014; 4(12):e006462.
Article25. Ro YS, Shin SD, Song KJ, Park CB, Lee EJ, Ahn KO, et al. A comparison of outcomes of out-of-hospital cardiac arrest with non-cardiac etiology between emergency departments with low- and high-resuscitation case volume. Resuscitation. 2012; 83(7):855–861. PMID: 22366719.
Article26. Engdahl J, Bång A, Karlson BW, Lindqvist J, Herlitz J. Characteristics and outcome among patients suffering from out of hospital cardiac arrest of non-cardiac aetiology. Resuscitation. 2003; 57(1):33–41. PMID: 12668297.
Article27. Rab T, Kern KB, Tamis-Holland JE, Henry TD, McDaniel M, Dickert NW, et al. Cardiac arrest: a treatment algorithm for emergent invasive cardiac procedures in the resuscitated comatose patient. J Am Coll Cardiol. 2015; 66(1):62–73. PMID: 26139060.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Management of post-cardiac arrest syndrome
- Predictors of Neurological Outcomes in Out-of-Hospital Cardiac Arrest Survivors Treated with Therapeutic Hypothermia
- Pilot study on a rewarming rate of 0.15°C/hr versus 0.25°C/hr and outcomes in post cardiac arrest patients
- Hemoglobin concentration is associated with neurologic outcome after cardiac arrest in patients treated with targeted temperature management
- Management of post-cardiac arrest syndrome