Brain Tumor Res Treat.
2020 Apr;8(1):36-42. 10.14791/btrt.2020.8.e3.
Comparison of Diagnostic Performance of Two-Dimensionaland Three-Dimensional Fractal Dimension and LacunarityAnalyses for Predicting the Meningioma Grade
- Affiliations
-
- 1Department of Robotics Engineering, Daegu Gyeongbuk Institute of Science and Technology, Daegu, Korea
- 2Department of Radiology and Research Institute of Radiological Science, Yonsei University College of Medicine, Seoul, Korea
- 3Departments of Neurosurgery, Yonsei University College of Medicine, Seoul, Korea
- 4Departments of Pathology, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2500120
- DOI: http://doi.org/10.14791/btrt.2020.8.e3
Abstract
- Background
: To compare the diagnostic performance of two-dimensional (2D) and three-dimensional (3D) fractal dimension (FD) and lacunarity features from MRI for predicting the meningioma grade.
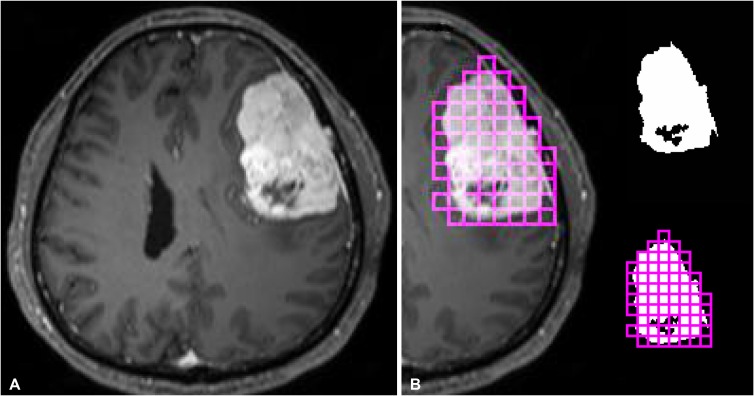
Methods
: This retrospective study included 123 meningioma patients [90 World Health Organization (WHO) grade I, 33 WHO grade II/III] with preoperative MRI including post-contrast T1-weighted imaging. The 2D and 3D FD and lacunarity parameters from the contrast-enhancing portion of the tumor were calculated. Reproducibility was assessed with the intraclass correlation coefficient. Multivariable logistic regression analysis using 2D or 3D fractal features was performed to predict the meningioma grade. The diagnostic ability of the 2D and 3D fractal models were compared.
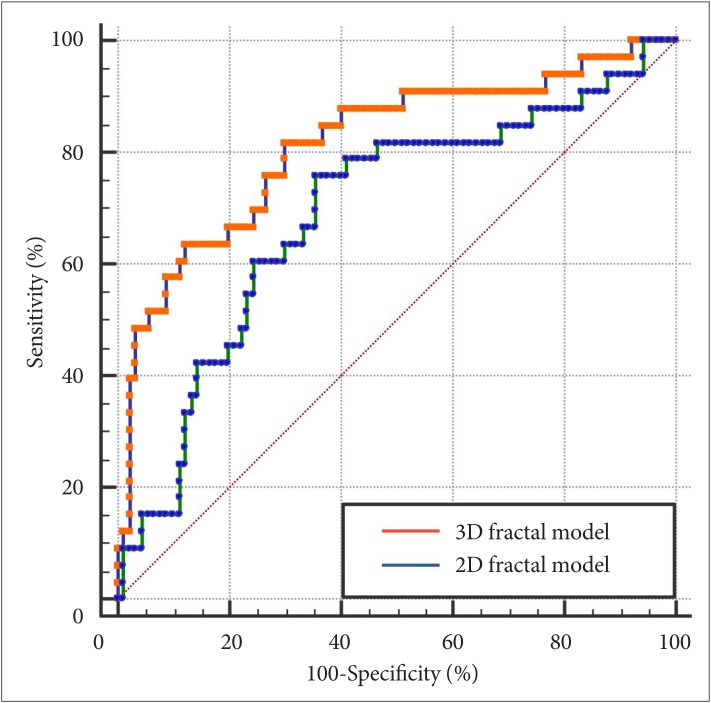
Results
: The reproducibility between observers was excellent, with intraclass correlation coefficients of 0.97, 0.95, 0.98, and 0.96 for 2D FD, 2D lacunarity, 3D FD, and 3D lacunarity, respectively. WHO grade II/III meningiomas had a higher 2D and 3D FD (p=0.003 and p<0.001, respectively) and higher 2D and 3D lacunarity (p=0.002 and p=0.006, respectively) than WHO grade I meningiomas. The 2D fractal model showed an area under the curve (AUC), accuracy, sensitivity, and specificity of 0.690 [95% confidence interval (CI) 0.581-0.799], 72.4%, 75.8%, and 64.4%, respectively. The 3D fractal model showed an AUC, accuracy, sensitivity, and specificity of 0.813 (95% CI 0.733-0.878), 82.9%, 81.8%, and 70.0%, respectively. The 3D fractal model exhibited significantly better diagnostic performance than the 2D fractal model (p<0.001).
Conclusion
: The 3D fractal analysis proved superiority in diagnostic performance to 2D fractal analysis in grading meningioma.
Keyword
Figure
Reference
-
1. Ostrom QT, Gittleman H, Xu J, et al. CBTRUS statistical report: primary brain and other central nervous system tumors diagnosed in the United States in 2009-2013. Neuro Oncol. 2016; 18(suppl_5):v1–v75. PMID: 28475809.2. Louis DN, Perry A, Reifenberger G, et al. The 2016 World Health Organization classification of tumors of the central nervous system: a summary. Acta Neuropathol. 2016; 131:803–820. PMID: 27157931.3. Kshettry VR, Ostrom QT, Kruchko C, Al-Mefty O, Barnett GH, Barnholtz-Sloan JS. Descriptive epidemiology of World Health Organization grades II and III intracranial meningiomas in the United States. Neuro Oncol. 2015; 17:1166–1173. PMID: 26008603.4. Rogers L, Barani I, Chamberlain M, et al. Meningiomas: knowledge base, treatment outcomes, and uncertainties. A RANO review. J Neurosurg. 2015; 122:4–23. PMID: 25343186.5. Goldbrunner R, Minniti G, Preusser M, et al. EANO guidelines for the diagnosis and treatment of meningiomas. Lancet Oncol. 2016; 17:e383–e391. PMID: 27599143.6. Nowosielski M, Galldiks N, Iglseder S, et al. Diagnostic challenges in meningioma. Neuro Oncol. 2017; 19:1588–1598. PMID: 28531331.7. Joo B, Han K, Choi YS, et al. Amide proton transfer imaging for differentiation of benign and atypical meningiomas. Eur Radiol. 2018; 28:331–339. PMID: 28687916.8. Sanverdi SE, Ozgen B, Oguz KK, et al. Is diffusion-weighted imaging useful in grading and differentiating histopathological subtypes of meningiomas? Eur J Radiol. 2012; 81:2389–2395. PMID: 21723681.9. Azizyan A, Eboli P, Drazin D, Mirocha J, Maya MM, Bannykh S. Differentiation of benign angiomatous and microcystic meningiomas with extensive peritumoral edema from high grade meningiomas with aid of diffusion weighted MRI. Biomed Res Int. 2014; 2014:650939. PMID: 25478572.10. Zhang H, Rödiger LA, Shen T, Miao J, Oudkerk M. Preoperative subtyping of meningiomas by perfusion MR imaging. Neuroradiology. 2008; 50:835–840. PMID: 18542938.11. Lee G, Lee HY, Park H, et al. Radiomics and its emerging role in lung cancer research, imaging biomarkers and clinical management: state of the art. Eur J Radiol. 2017; 86:297–307. PMID: 27638103.12. Lennon FE, Cianci GC, Cipriani NA, et al. Lung cancer-a fractal viewpoint. Nat Rev Clin Oncol. 2015; 12:664–675. PMID: 26169924.13. Liu S, Wang Y, Xu K, et al. Relationship between necrotic patterns in glioblastoma and patient survival: fractal dimension and lacunarity analyses using magnetic resonance imaging. Sci Rep. 2017; 7:8302. PMID: 28814802.14. Liu S, Fan X, Zhang C, et al. MR imaging based fractal analysis for differentiating primary CNS lymphoma and glioblastoma. Eur Radiol. 2019; 29:1348–1354. PMID: 30167811.15. Smitha KA, Gupta AK, Jayasree RS. Fractal analysis: fractal dimension and lacunarity from MR images for differentiating the grades of glioma. Phys Med Biol. 2015; 60:6937–6947. PMID: 26305773.16. Falconer K. Fractal geometry: mathematical foundations and applications. Hoboken: John Wiley & Sons;2004.17. Plotnick RE, Gardner RH, O'Neill RV. Lacunarity indices as measures of landscape texture. Landsc Ecol. 1993; 8:201–211.18. Metze K. Fractal dimension of chromatin: potential molecular diagnostic applications for cancer prognosis. Expert Rev Mol Diagn. 2013; 13:719–735. PMID: 24063399.19. Kane AJ, Sughrue ME, Rutkowski MJ, et al. Anatomic location is a risk factor for atypical and malignant meningiomas. Cancer. 2011; 117:1272–1278. PMID: 21381014.20. DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988; 44:837–845. PMID: 3203132.21. Sanghera B, Banerjee D, Khan A, et al. Reproducibility of 2D and 3D fractal analysis techniques for the assessment of spatial heterogeneity of regional blood flow in rectal cancer. Radiology. 2012; 263:865–873. PMID: 22438361.22. Park YW, Kim S, Ahn SS, et al. Magnetic resonance imaging-based 3-dimensional fractal dimension and lacunarity analyses may predict the meningioma grade. Eur Radiol. 2020; 4. 09. DOI: 10.1007/s00330-020-06788-8. [Epub].23. Nakasu S, Nakasu Y, Nakajima M, Matsuda M, Handa J. Preoperative identification of meningiomas that are highly likely to recur. J Neurosurg. 1999; 90:455–462. PMID: 10067913.24. Siegers HP, Zuber P, Hamou MF, van Melle GD, de Tribolet N. The implications of the heterogeneous distribution of Ki-67 labelled cells in meningiomas. Br J Neurosurg. 1989; 3:101–107. PMID: 2789703.25. Coroller TP, Bi WL, Huynh E, et al. Radiographic prediction of meningioma grade by semantic and radiomic features. PLoS One. 2017; 12:e0187908. PMID: 29145421.26. Park YW, Oh J, You SC, et al. Radiomics and machine learning may accurately predict the grade and histological subtype in meningiomas using conventional and diffusion tensor imaging. Eur Radiol. 2019; 29:4068–4076. PMID: 30443758.27. Park YW, Han K, Ahn SS, et al. Whole-tumor histogram and texture analyses of DTI for evaluation of IDH1-mutation and 1p/19q-codeletion status in World Health Organization grade II gliomas. AJNR Am J Neuroradiol. 2018; 39:693–698. PMID: 29519794.28. Park YW, Choi YS, Ahn SS, Chang JH, Kim SH, Lee SK. Radiomics MRI phenotyping with machine learning to predict the grade of lowergrade gliomas: a study focused on nonenhancing tumors. Korean J Radiol. 2019; 20:1381–1389. PMID: 31464116.29. Park CJ, Choi YS, Park YW, et al. Diffusion tensor imaging radiomics in lower-grade glioma: improving subtyping of isocitrate dehydrogenase mutation status. Neuroradiology. 2020; 62:319–326. PMID: 31820065.30. Park YW, Han K, Ahn SS, et al. Prediction of IDH1-mutation and 1p/19q-codeletion status using preoperative MR imaging phenotypes in lower grade gliomas. AJNR Am J Neuroradiol. 2018; 39:37–42. PMID: 29122763.31. Park JE, Park SY, Kim HJ, Kim HS. Reproducibility and generalizability in radiomics modeling: possible strategies in radiologic and statistical perspectives. Korean J Radiol. 2019; 20:1124–1137. PMID: 31270976.32. Toh CH, Castillo M, Wong AM, et al. Differentiation between classic and atypical meningiomas with use of diffusion tensor imaging. AJNR Am J Neuroradiol. 2008; 29:1630–1635. PMID: 18583409.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prediction of osteoporosis using fractal analysis on periapical and panoramic radiographs
- Fractal dimension from radiographs of bone as indicatos of possible osteoporosis
- Characterization of trabecular bone structure using 2D Fourier transformation and fractal analysis
- Prediction of osteoporosis using fractal analysis on periapical radiographs
- Fractal Dimension Of Ct Images Of Normal Parotid Glands