J Cerebrovasc Endovasc Neurosurg.
2020 Mar;22(1):15-19. 10.7461/jcen.2020.22.1.15.
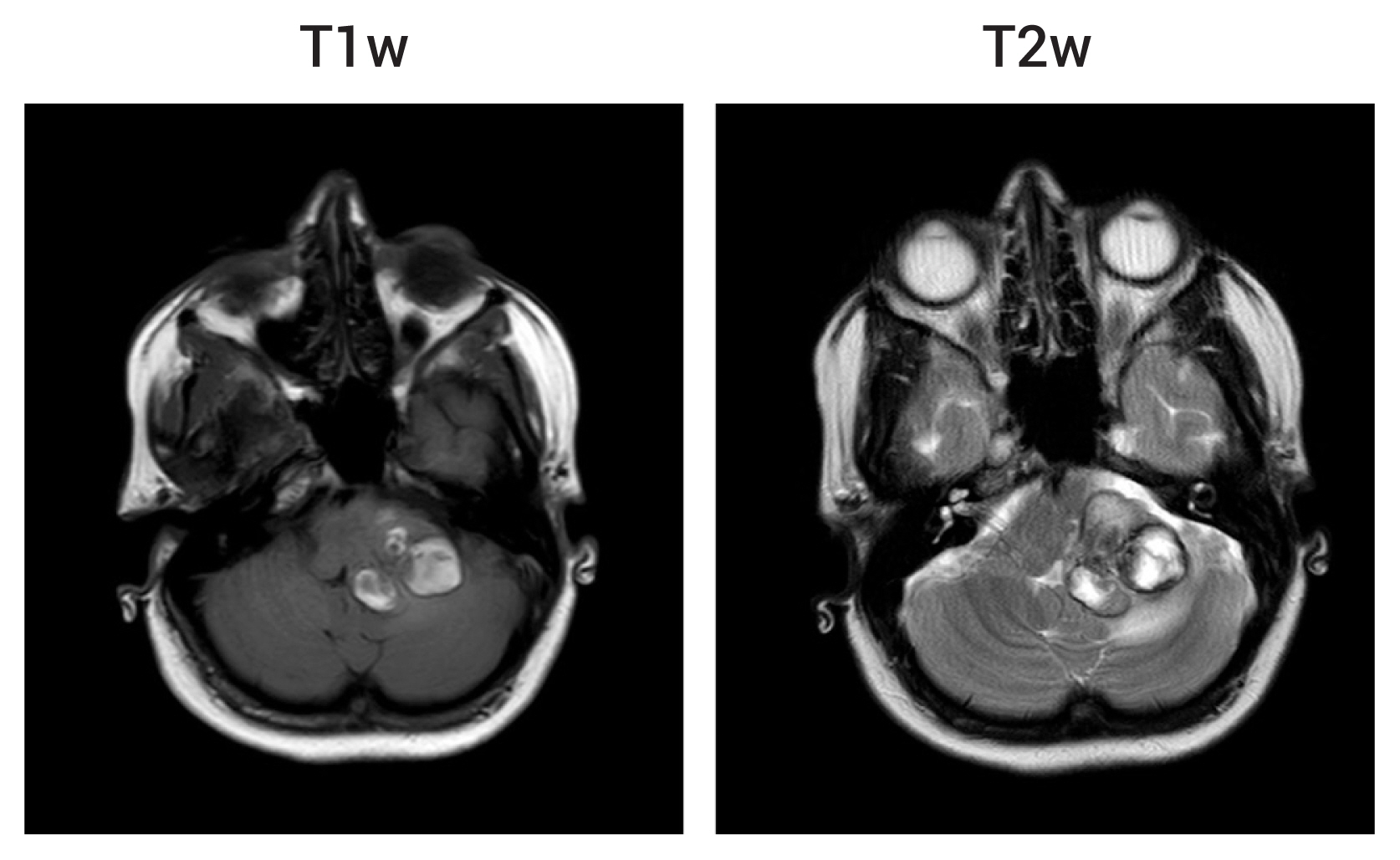
Multiple cerebral cavernousmalformations in association witha Dubowitz-like syndrome
- Affiliations
-
- 1Department of Neurosurgery, Royal Preston Hospital, Lancashire Teaching Hospitals NHS Trust, Preston, PR2 9HT, UK
- KMID: 2500069
- DOI: http://doi.org/10.7461/jcen.2020.22.1.15
Abstract
- Cerebral cavernous malformations (CCMs) are proliferative sinusoidal vascular lesions and are the most common vascular malformations of the brain. They can occur sporadically or secondary to an underlying genetic predisposition where multiple lesions are commonly seen. Dubowitz syndrome is a clinically-diagnosed rare genetic disorder with an unknown molecular basis. An association between these conditions has not been reported previously. A 30-year-old woman with a Dubowitz- like syndrome presented with acute left leg weakness, gait ataxia and transient loss of consciousness. Imaging revealed five CCMs with recent hemorrhage in relation to one lesion in the left middle cerebellar peduncle. A recurrent hemorrhage from the same lesion occurred ten weeks later and she underwent microsurgical excision of this malformation. Genetic analysis revealed an unbalanced chromosomal rearrangement involving partial deletion of chromosome 7q21, the locus of the CCM1/ KRIT1 gene known to be associated with familial CCMs. This is the first description of CCMs in association with the Dubowitz phenotype. The genetic basis of Dubowitz syndrome may be heterogeneous but, for the first time, overlap is demonstrated between this condition and multiple CCMs, with a possible common genetic etiology. Knowledge of this association may be of help in the management of acute neurological presentations in Dubowitz-like syndromes.
Figure
Reference
-
1. Batra S, Lin D, Recinos PF, Zhang J, Rigamonti D. Cavernous malformations: natural history, diagnosis and treatment. Nat Rev Neurol. 2009; Dec. 5(12):659–70.
Article2. Bergametti F, Denier C, Labauge P, Arnoult M, Boetto S, Clanet M, et al. Mutations within the programmed cell death 10 gene cause cerebral cavernous malformations. Am J Hum Genet. 2005; Jan. 76(1):42–51.
Article3. Craig HD, Gunel M, Cepeda O, Johnson EW, Ptacek L, Steinberg GK, et al. Multilocus linkage identifies two new loci for a mendelian form of stroke, cerebral cavernous malformation, at 7p15-13 and 3q25.2-27. Hum Mol Genet. 1998; Nov. 7(12):1851–8.
Article4. Dieks JK, Baumer A, Wilichowski E, Rauch A, Sigler M. Microcephalic osteodysplastic primordial dwarfism type II (MOPD II) with multiple vascular complications misdiagnosed as Dubowitz syndrome. Eur J Pediatr. 2014; Sep. 173(9):1253–6.
Article5. Dubovsky J, Zabramski JM, Kurth J, Spetzler RF, Rich SS, Orr HT, et al. A gene responsible for cavernous malformations of the brain maps to chromosome 7q. Hum Mol Genet. 1995; Mar. 4(3):453–8.
Article6. Dubowitz V. Familial low birthweight dwarfism with an unusual facies and a skin eruption. J Med Genet. 1965; Mar. 2(1):12–7.
Article7. Gil-Nagel A, Dubovsky J, Wilcox KJ, Stewart JM, Anderson VE, Leppik IE, et al. Familial cerebral cavernous angioma: a gene localized to a 15-cM interval on chromosome 7q. Ann Neurol. 1996; Jun. 39(6):807–10.
Article8. Kim J. Introduction to cerebral cavernous malformation: a brief review. BMB Rep. 2016; May. 49(5):255–62.
Article9. Liquori CL, Berg MJ, Siegel AM, Huang E, Zawistowski JS, Stoffer T, et al. Mutations in a gene encoding a novel protein containing a phosphotyrosine-binding domain cause type 2 cerebral cavernous malformations. Am J Hum Genet. 2003; Dec. 73(6):1459–64.
Article10. Oguz KK, Ozgen B, Erdem Z. Cranial midline abnormalities in Dubowitz syndrome: MR imaging findings. Eur Radiol. 2003; May. 13(5):1056–7.
Article11. Sahoo T, Johnson EW, Thomas JW, Kuehl PM, Jones TL, Dokken CG, et al. Mutations in the gene encoding KRIT1, a Krev-1/rap1a binding protein, cause cerebral cavernous malformations (CCM1). Hum Mol Genet. 1999; Nov. 8(12):2325–33.
Article12. Stewart DR, Pemov A, Johnston JJ, Sapp JC, Yeager M, He J, et al. Dubowitz syndrome is a complex comprised of multiple, genetically distinct and phenotypically overlapping disorders. PLoS One. 2014; Jun. 9(6):e98686.
Article13. Sunku AJ, Gomez MR, Klass DW. Epileptic seizures, EEG abnormalities, and neuronal heterotopia in the Dubowitz syndrome. Am J Electroneurodiagnostic Technol. 1998; 38(3):156–63.
Article14. Swartz KR, Resnick D, Iskandar BJ, Wargowski D, Brockmeyer D, Opitz J. Craniocervical anomalies in Dubowitz syndrome. Three cases and a literature review. Pediatr Neurosurg. 2003; May. 38(5):238–43.15. Tsukahara M, Opitz JM. Dubowitz syndrome: review of 141 cases including 36 previously unreported patients. Am J Med Genet. 1996; May. 63(1):277–89.
Article16. Urquhart JE, Williams SG, Bhaskar SS, Bowers N, Clayton-Smith J, Newman WG. Deletion of 19q13 reveals clinical overlap with Dubowitz syndrome. J Hum Genet. 2015; Dec. 60(12):781–5.
Article17. Washington CW, McCoy KE, Zipfel GJ. Update on the natural history of cavernous malformations and factors predicting aggressive clinical presentation. Neurosurg Focus. 2010; Sep. 29(3):E7.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Anesthesia of a patient with Dubowitz syndrome: A case report
- A Case of the Dubowitz Syndrome
- Multiple Cerebral Infarction in Cogan's Syndrome
- Reversible Cerebral Vasoconstriction Syndrome Induced by Blood Transfusion
- Bilateral Anterior Cerebral Artery Infarction Associated with Reversible Cerebral Vasoconstriction Syndrome