Korean J Gastroenterol.
2020 Mar;75(3):167-171. 10.4166/kjg.2020.75.3.167.
Liver Graft Failure and Bile Cast Nephropathy
- Affiliations
-
- 1Department of Internal Medicine, Merkur University Hospital, Zagreb, Croatia. anna.mrzljak@mef.hr
- 2Department of Medicine, School of Medicine, University of Zagreb, Zagreb, Croatia.
- 3Department of Surgery, Merkur University Hospital, Zagreb, Croatia.
- 4Unit for Renal Pathology and Electron Microscopy, Department of Pathology and Cytology, Dubrava University Hospital, Zagreb, Croatia.
- KMID: 2471901
- DOI: http://doi.org/10.4166/kjg.2020.75.3.167
Abstract
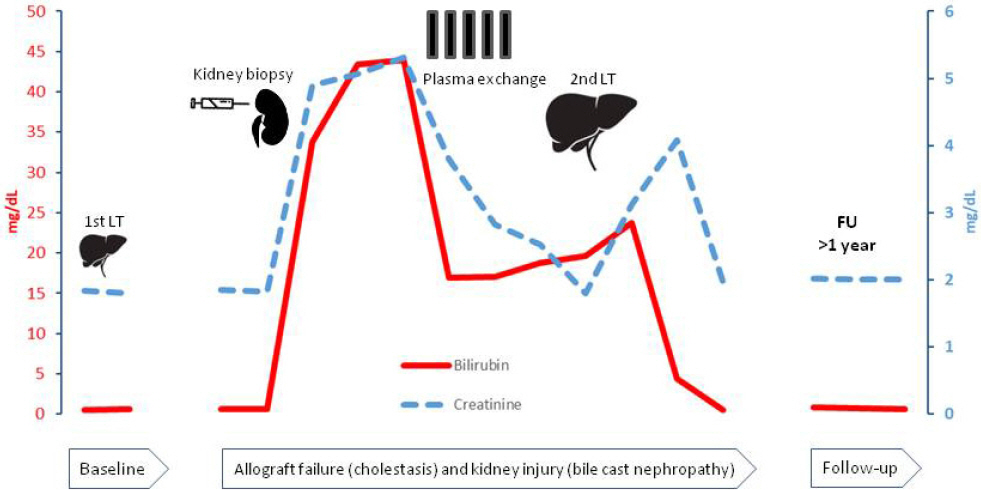
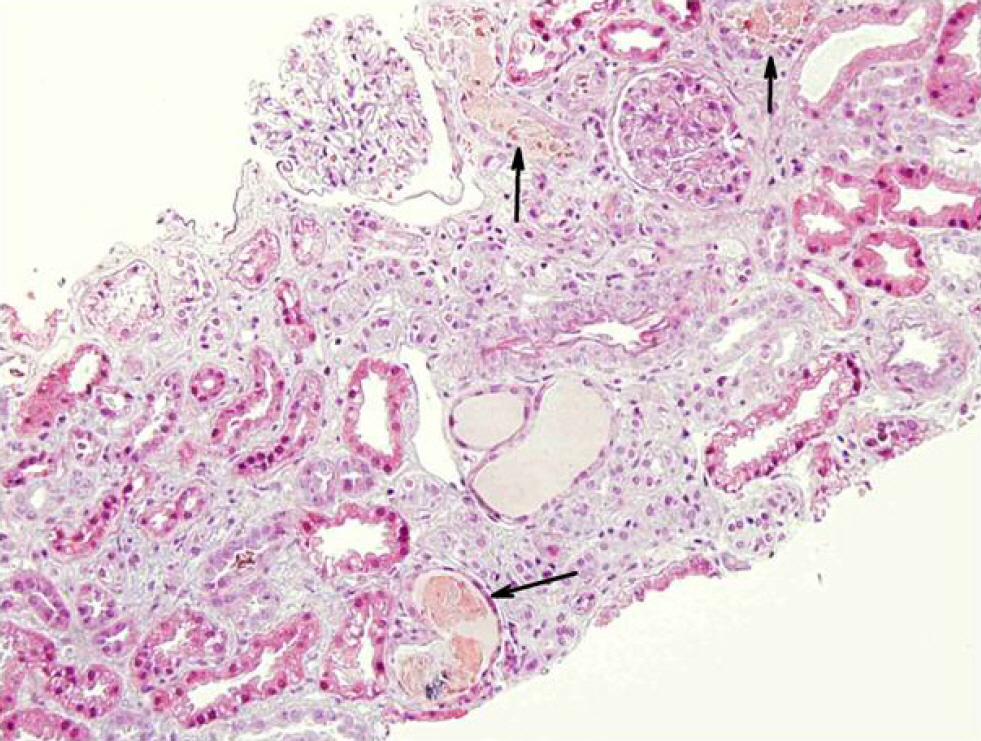
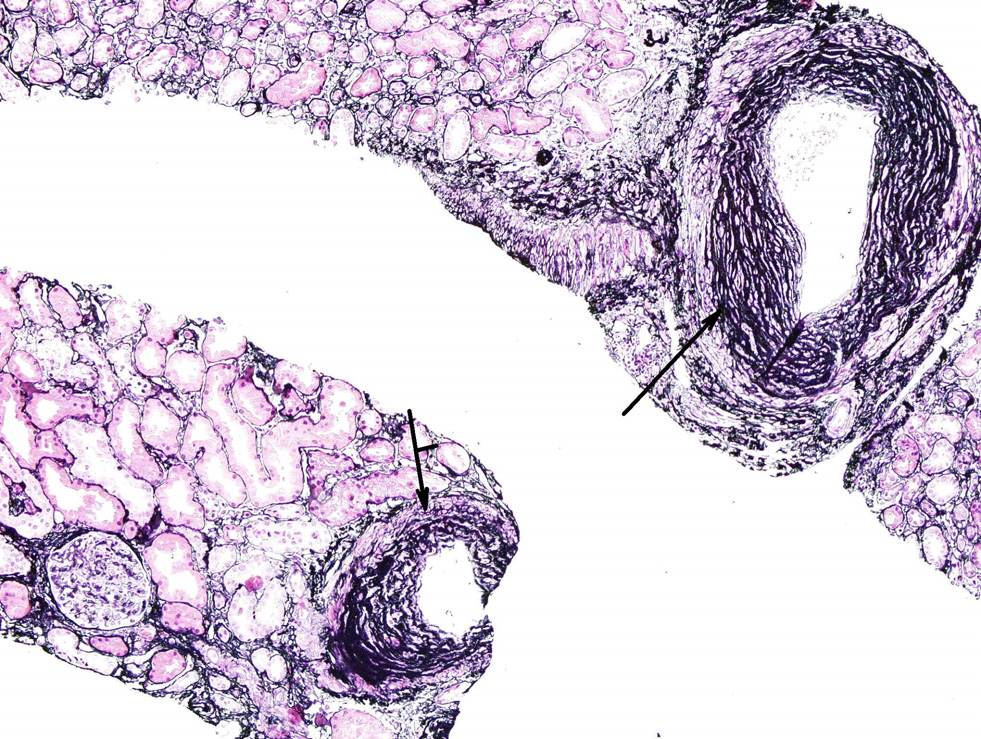
- The consequences of graft failure after liver transplantation (LT) range far beyond the liver. The kidneys are often affected, where persistent and progressive cholestasis can result in acute kidney injury (AKI) leading to the development of bile cast nephropathy (BCN). BCN is an often unrecognized condition that is characterized by proximal tubulopathy and the formation of bile casts in the distal tubules, which is almost diagnosed exclusively on a kidney biopsy or autopsy. This condition is potentially reversible, provided the bilirubin levels can be reduced early. LT may represent a treatment option in the case of irreversible liver (or liver graft) failure, which is beneficial for both the liver and the kidney. This paper reports a case of BCN in a patient with idiopathic graft failure after LT. Despite his chronic kidney disease, liver re-transplantation led to the successful improvement of his AKI.
MeSH Terms
Figure
Reference
-
References
1. Ojo AO, Held PJ, Port FK, et al. Chronic renal failure after transplantation of a nonrenal organ. N Engl J Med. 2003; 349:931–940.
Article2. Hussaini T, Yoshida EM, Partovi N, et al. Early persistent progressive acute kidney injury and graft failure post liver transplantation. Transplant Direct. 2019; 5:e429.
Article3. Krones E, Pollheimer MJ, Rosenkranz AR, Fickert P. Cholemic nephropathy - historical notes and novel perspectives. Biochim Biophys Acta Mol Basis Dis. 2018; 1864(4 Pt B):1356–1366.
Article4. Aniort J, Poyet A, Kemeny JL, Philipponnet C, Heng AE. Bile cast nephropathy caused by obstructive cholestasis. Am J Kidney Dis. 2017; 69:143–146.
Article5. Chan S, Spraggon ES, Francis L, Wolley MJ. Bile cast nephropathy in a patient with obstructive jaundice. Kidney Int Rep. 2018; 4:338–340.
Article6. Flores A, Nustas R, Nguyen HL, Rahimi RS. Severe cholestasis and bile acid nephropathy from anabolic steroids successfully treated with plasmapheresis. ACG Case Rep J. 2016; 3:133–135.
Article7. Torrealba J, Sweed NT, Burguete D, Hendricks AR. Bile cast nephropathy: a pathologic finding with manifold causes dis-played in an adult with alcoholic steatohepatitis and in a child with Wilson's disease. Case Rep Nephrol Dial. 2018; 8:207–215.
Article8. Betjes MG, Bajema I. The pathology of jaundice-related renal in-sufficiency: cholemic nephrosis revisited. J Nephrol. 2006; 19:229–233.9. Fickert P, Krones E, Pollheimer MJ, et al. Bile acids trigger cholemic nephropathy in common bile-duct-ligated mice. Hepatology. 2013; 58:2056–2069.
Article10. Krones E, Wagner M, Eller K, Rosenkranz AR, Trauner M, Fickert P. Bile acid-induced cholemic nephropathy. Dig Dis. 2015; 33:367–375.
Article11. van Slambrouck CM, Salem F, Meehan SM, Chang A. Bile cast nephropathy is a common pathologic finding for kidney injury associated with severe liver dysfunction. Kidney Int. 2013; 84:192–197.
Article12. Rector WG Jr, Kanel GC, Rakela J, Reynolds TB. Tubular dysfunction in the deeply jaundiced patient with hepatorenal syndrome. Hepatology. 1985; 5:321–326.
Article13. Bairaktari E, Liamis G, Tsolas O, Elisaf M. Partially reversible renal tubular damage in patients with obstructive jaundice. Hepatology. 2001; 33:1365–1369.
Article14. Bomzon A, Holt S, Moore K. Bile acids, oxidative stress, and renal function in biliary obstruction. Semin Nephrol. 1997; 17:549–562.15. Chawla LS, Eggers PW, Star RA, Kimmel PL. Acute kidney injury and chronic kidney disease as interconnected syndromes. N Engl J Med. 2014; 371:58–66.
Article16. Pitlick M, Rastogi P. All that glitters yellow is not gold: presentation and pathophysiology of bile cast nephropathy. Int J Surg Pathol. 2017; 25:652–658.
Article17. Sens F, Bacchetta J, Rabeyrin M, Juillard L. Efficacy of extracorporeal albumin dialysis for acute kidney injury due to cholestatic jaundice nephrotoxicity. BMJ Case Rep. 2016; 2016:bcr2015213257.
Article18. Patel J, Walayat S, Kalva N, Palmer-Hill S, Dhillon S. Bile cast nephropathy: a case report and review of the literature. World J Gastroenterol. 2016; 22:6328–6334.
Article19. van de Ven SE, Pavlov KV, Beutler JJ, Scheffer RC. Bile cast nephropathy caused by obstructive pancreatic carcinoma and failed ERCP. ACG Case Rep J. 2018; 5:e88.
Article20. Daga Ruiz D, Fonseca San Miguel F, González de Molina FJ, Úbeda-Iglesias A, Navas Pérez A, Jannone Forés R. Plasmapheresis and other extracorporeal filtration techniques in critical patients. Med Intensiva. 2017; 41:174–187.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Biliary Cast Syndrome with a Biliary Stricture and Suppurative Cholangitis after Liver Transplantation
- A Case of Biliary Cast Syndrome After Endoscopic and Percutaneous Management of Common Bile Duct Stone
- Biliary Cast Syndrome in Non-Liver Surgery Patients
- Biliary Cast Successfully Removed by Percutaneous Transhepatic Cholangioscopy, and This Developed in a Patient Who Received Orthotopic Liver Transplantation
- Bile Cast Nephropathy Associated with Acute Hepatitis A