Korean J Orthod.
2020 Mar;50(2):136-144. 10.4041/kjod.2020.50.2.136.
Growth observation and orthodontic treatment of a hemifacial microsomia patient treated with distraction osteogenesis
- Affiliations
-
- 1Department of Orthodontics, School of Dentistry, Chonbuk National University, Jeonju, Korea. kjgortho@jbnu.ac.kr
- 2Institute of Oral Biosciences, School of Dentistry, Chonbuk National University, Jeonju, Korea.
- 3Research Institute of Clinical Medicine of Chonbuk National University-Biomedical Research Institute of Chonbuk National University Hospital, Jeonju, Korea.
- KMID: 2471874
- DOI: http://doi.org/10.4041/kjod.2020.50.2.136
Abstract
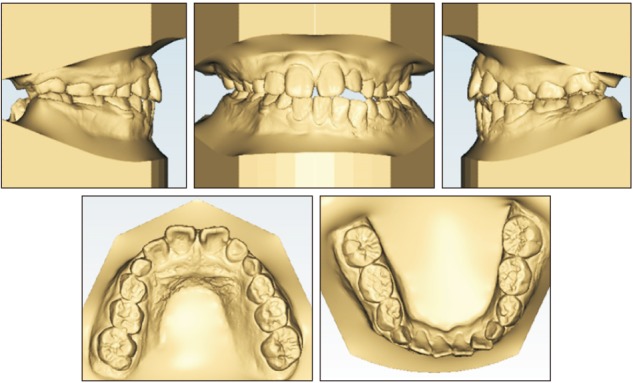
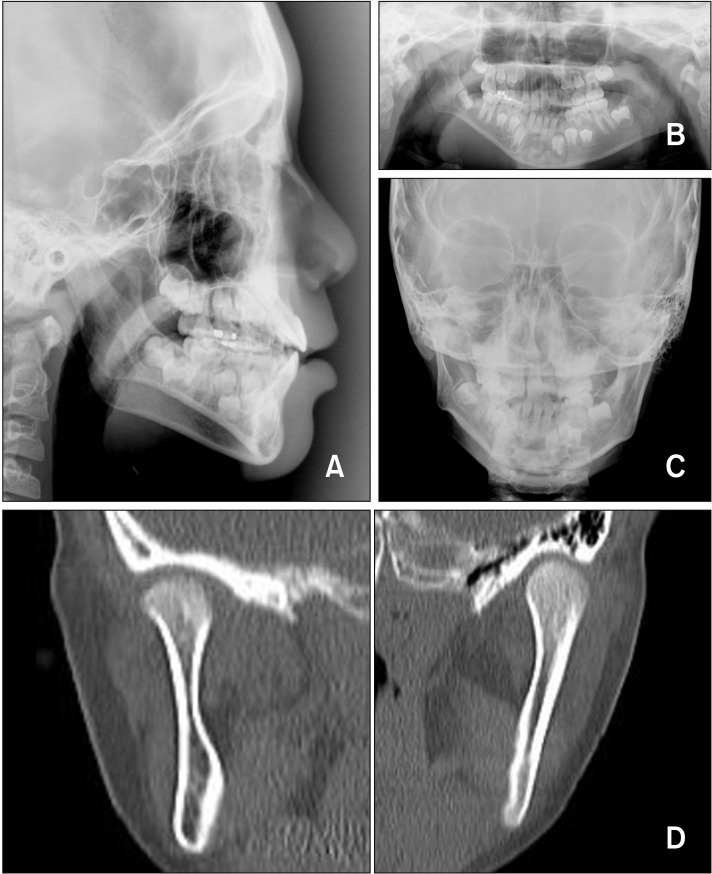
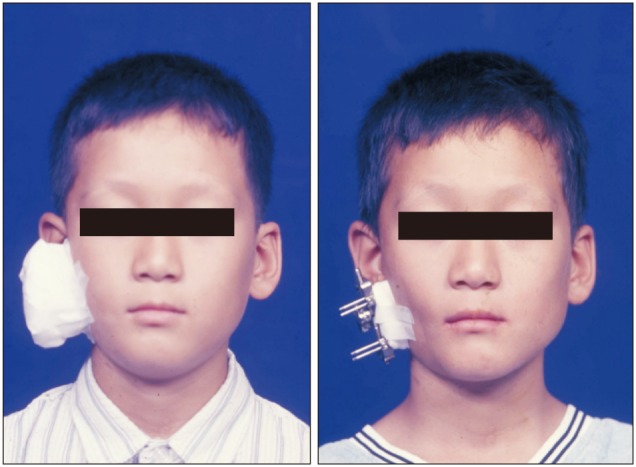
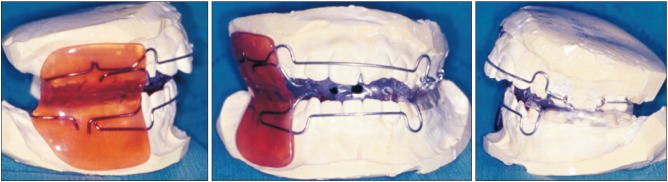
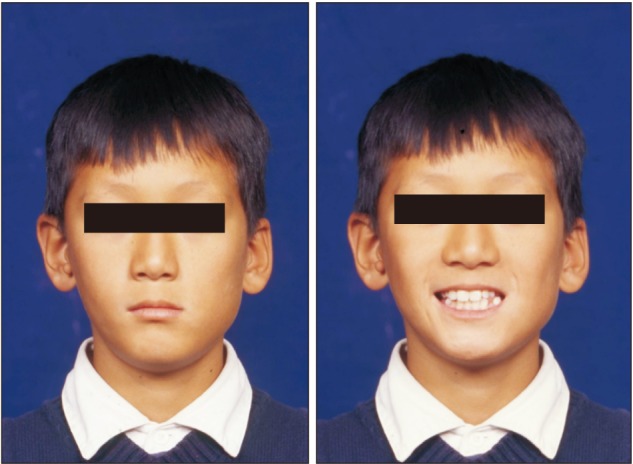
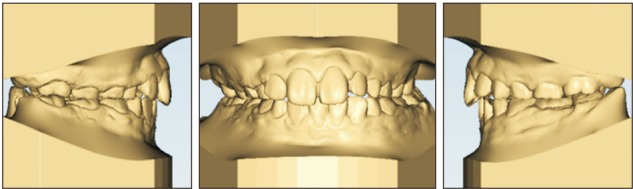
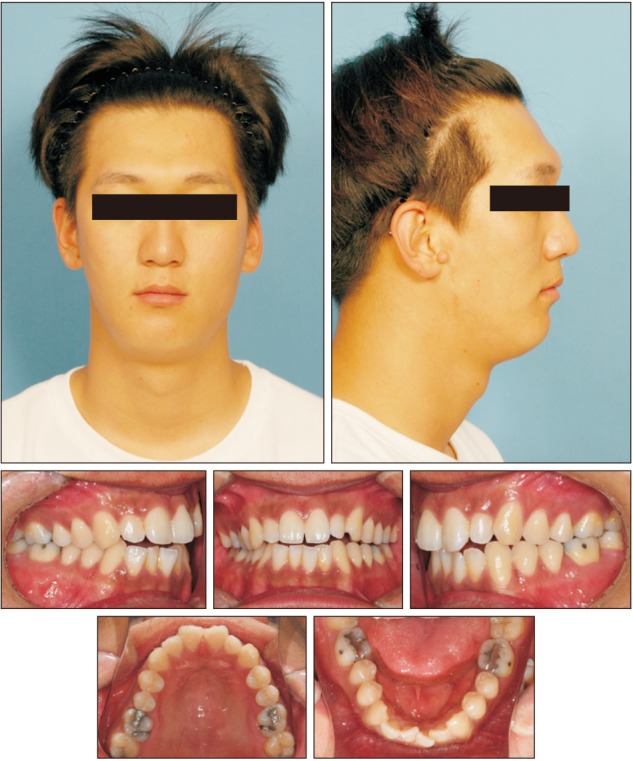
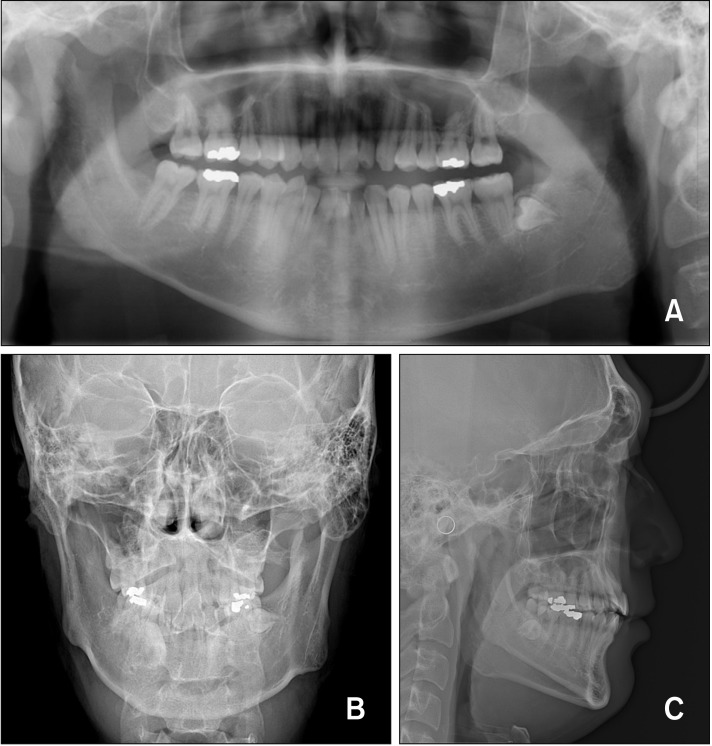
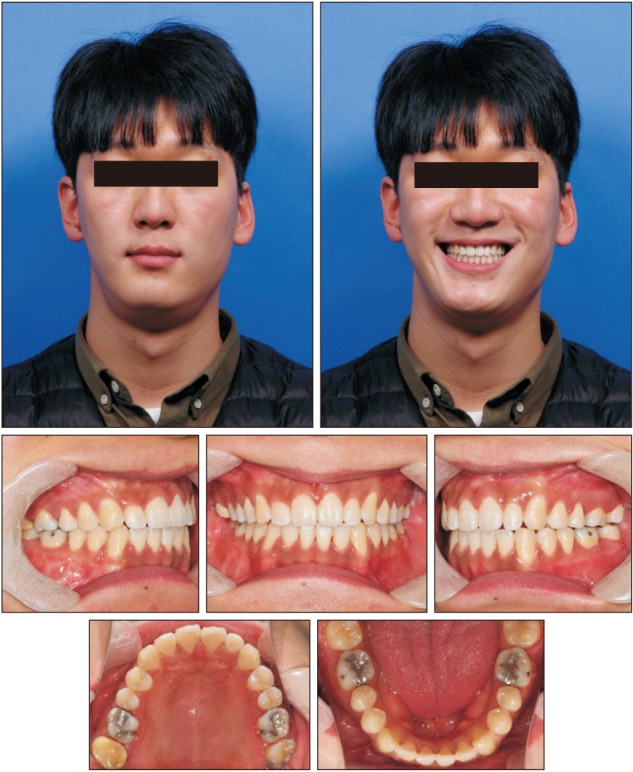
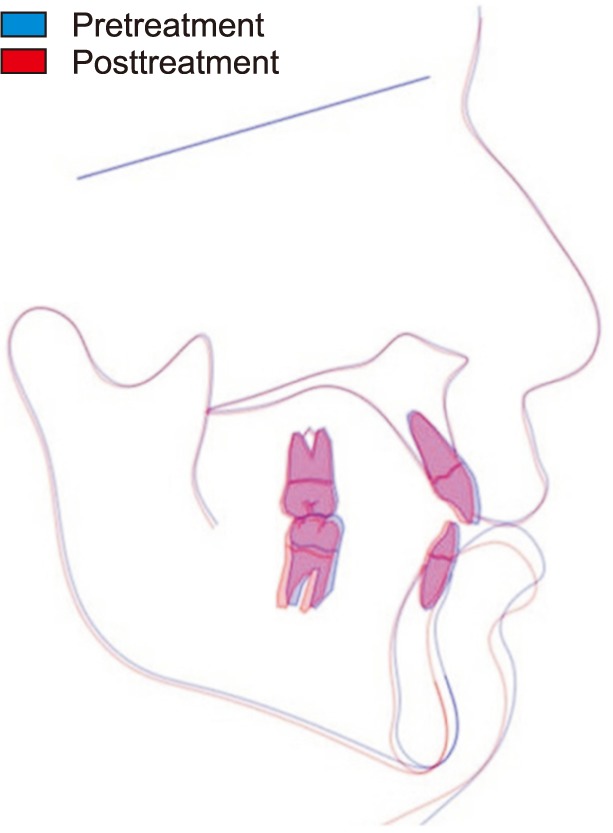
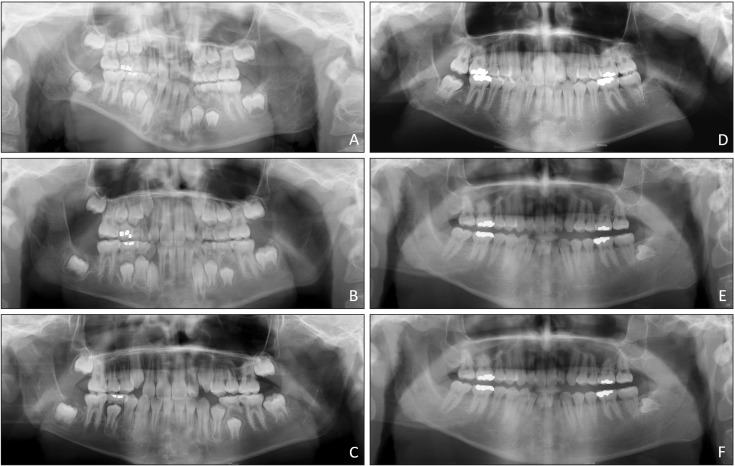
- Hemifacial microsomia (HFM) patients may experience emotional withdrawal during their growth period due to their abnormal facial appearance. Distraction osteogenesis at an early age to improve their appearance can encourage these patients. Some abnormalities of the affected side can be overcome by distraction osteogenesis at an early age. However, differences in the growth rate between the affected and unaffected sides during the rest of the growth period are inevitable due to the characteristics of HFM. Therefore, re-evaluation should be performed after completion of growth in order to achieve stable occlusion through either orthognathic surgery or camouflage orthodontic treatment. An eight-year-old patient visited the clinic exhibiting features of HFM with slight mandibular involvement. He received phase I treatment with distraction osteogenesis and a functional appliance. Distraction osteogenesis was performed at the right ramus, which resulted in an open bite at the right posterior dentition. After distraction osteogenesis, a functional appliance and partial fixed appliance were used to achieve extrusion of the affected posterior dentition and settlement of the occlusion adjustment on the unaffected posterior dentition. The patient visited the clinic regularly for follow-up assessments, and at the age of 20 years, he showed facial asymmetry of the mandible, which had deviated to the right side. He received orthodontic treatment to improve the occlusion of his posterior dentition after the growth period. Without orthognathic surgery, stable occlusion and a satisfactory facial appearance were obtained through camouflage orthodontic treatment.
MeSH Terms
Figure
Reference
-
1. Birgfeld CB, Heike C. Craniofacial microsomia. Semin Plast Surg. 2012; 26:91–104. PMID: 23633936.
Article2. Wang RR, Andres CJ. Hemifacial microsomia and treatment options for auricular replacement: a review of the literature. J Prosthet Dent. 1999; 82:197–204. PMID: 10424984.
Article3. Fan WS, Mulliken JB, Padwa BL. An association between hemifacial microsomia and facial clefting. J Oral Maxillofac Surg. 2005; 63:330–334. PMID: 15742282.
Article4. Kaban LB, Moses MH, Mulliken JB. Surgical correction of hemifacial microsomia in the growing child. Plast Reconstr Surg. 1988; 82:9–19. PMID: 3289066.
Article5. Prada Madrid JR, Montealegre G, Gomez V. A new classification based on the Kaban's modification for surgical management of craniofacial microsomia. Craniomaxillofac Trauma Reconstr. 2010; 3:1–7. PMID: 22110812.6. Mielnik-Błaszczak M, Olszewska K. Hemifacial microsomia-review of the literature. Dent Med Probl. 2011; 48:80–85.7. Mackool RJ, Hopper RA, Grayson BH, Holliday R, McCarthy JG. Volumetric change of the medial pterygoid following distraction osteogenesis of the mandible: an example of the associated soft-tissue changes. Plast Reconstr Surg. 2003; 111:1804–1807. PMID: 12711939.
Article8. Molina F, Ortiz Monasterio F. Mandibular elongation and remodeling by distraction: a farewell to major osteotomies. Plast Reconstr Surg. 1995; 96:825–840. discussion 841–2. PMID: 7652056.9. Pluijmers BI, Caron CJ, Dunaway DJ, Wolvius EB, Koudstaal MJ. Mandibular reconstruction in the growing patient with unilateral craniofacial microsomia: a systematic review. Int J Oral Maxillofac Surg. 2014; 43:286–295. PMID: 24332589.
Article10. Pertschuk MJ, Whitaker LA. Psychosocial outcome of craniofacial surgery in children. Plast Reconstr Surg. 1988; 82:741–746. PMID: 3174865.
Article11. McDowell EH, Baker IM. The skeletodental adaptations in deep bite correction. Am J Orthod Dentofacial Orthop. 1991; 100:370–375. PMID: 1927988.
Article12. Liu H, Zhang X, Liu L, Chen Q, Shao J, Luo E. Combined bimaxillary distraction osteogenesis associated with orthognathic surgery for hemifacial microsomia in adults. Aesthetic Plast Surg. 2017; 41:650–660. PMID: 28233131.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Distraction osteogenesis in patients with hemifacial microsomia
- Distraction Osteogenesis of Mandible using Short-Sagittal Osteotomy for the Patient with Hemifacial Microsomia
- Sequential treatment for a patient with hemifacial microsomia: 10 year-long term follow up
- Correction of Facial Asymmetry Using Costochondral Graft and Orthognathic Surgery in Hemifacial Microsomia Patient: Case Report
- Distraction osteogenesis of mandible in hemifacial microsomia