J Korean Ophthalmol Soc.
2020 Mar;61(3):319-324. 10.3341/jkos.2020.61.3.319.
Acute Leukemia Relapse Presenting as Recurrent Involvement of the Optic Nerve
- Affiliations
-
- 1Department of Ophthalmology, Ajou University College of Medicine, Suwon, Korea. mingming8@naver.com
- KMID: 2471776
- DOI: http://doi.org/10.3341/jkos.2020.61.3.319
Abstract
- PURPOSE
To report two cases with recurrent involvement of the optic nerve as the initial sign of acute leukemic relapse.
CASE SUMMARY
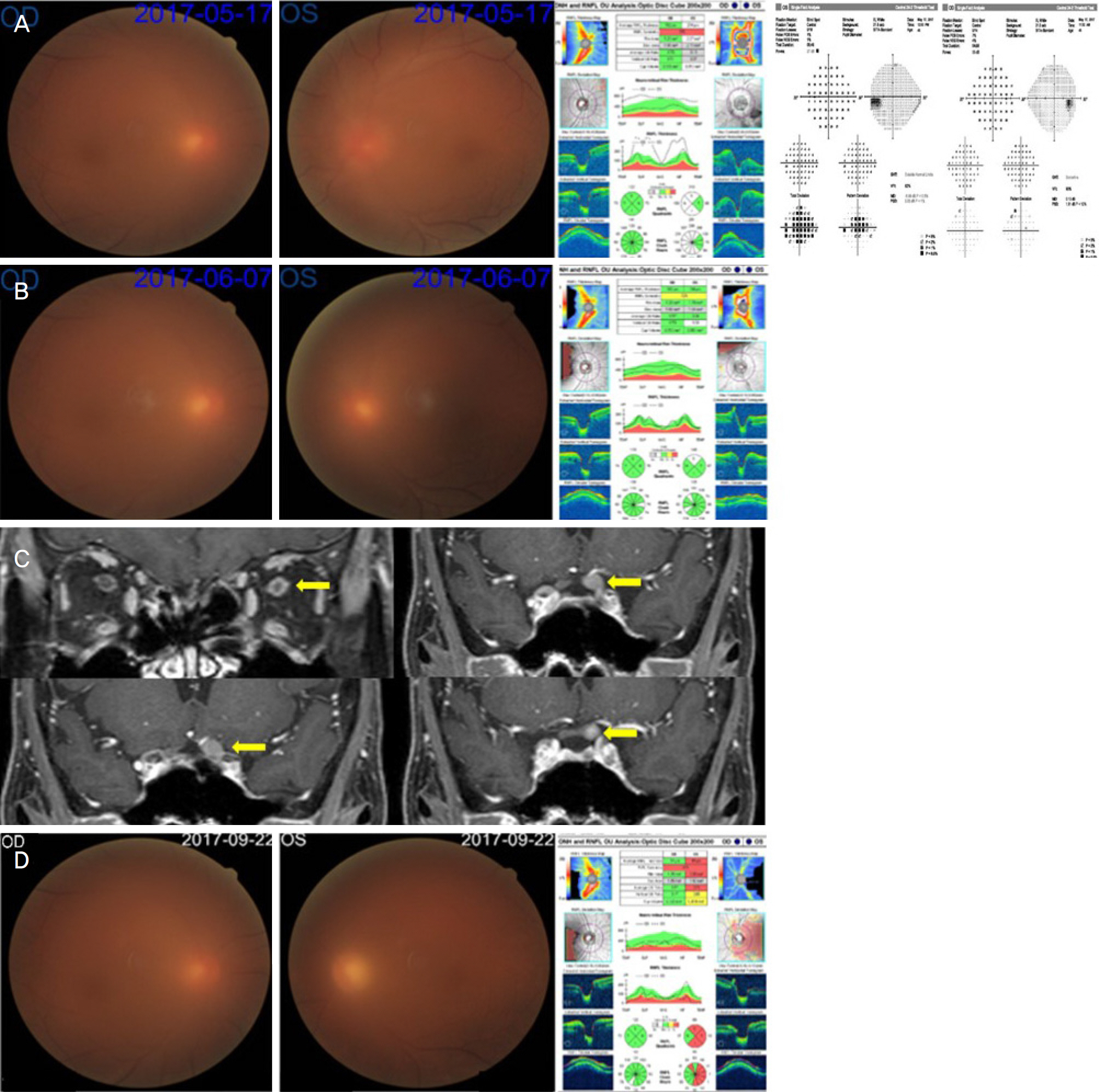
An 8-year-old male with acute lymphoblastic leukemia on the maintenance chemotherapy was referred for a decrease in visual acuity in the right eye. The visual acuity and optic disc swelling were completely resolved with high-dose steroid therapy. Two months after the initial presentation, the symptoms recurred and brain/orbit magnetic resonance imaging (MRI) showed high intensity along the right optic nerve from the retrobulbar area to the optic chiasm. The visual acuity was restored after high-dose steroid therapy. One month after the second attack, the symptoms recurred and the cerebrospinal fluid cytology was positive for lymphoblasts. Three weeks after the intrathecal chemotherapy, the visual acuity improved fully, but optic disc atrophy developed. A 45-year-old male, who received allogenic peripheral blood stem cell transplantation for acute myeloid leukemia, presented with a decrease in visual acuity in the left eye. The left optic disc swelling improved with high-dose steroid therapy, but the medication was restarted due to the recurrence of symptoms 3 weeks later. Brain MRI showed a mass lesion compressing the left optic nerve, presumed to be a myeloid sarcoma. One month after local irradiation, the visual acuity was no light perception in the left eye.
CONCLUSIONS
In patients with a prior history of acute leukemia, the recurrent involvement of the optic nerve should be considered as a central nerve system relapse, regardless of improvement with steroid treatment.
Keyword
MeSH Terms
-
Atrophy
Brain
Cerebrospinal Fluid
Child
Drug Therapy
Humans
Leukemia*
Leukemia, Myeloid, Acute
Magnetic Resonance Imaging
Maintenance Chemotherapy
Male
Middle Aged
Optic Chiasm
Optic Nerve*
Peripheral Blood Stem Cell Transplantation
Precursor Cell Lymphoblastic Leukemia-Lymphoma
Recurrence*
Sarcoma, Myeloid
Steroids
Visual Acuity
Steroids
Figure
Reference
-
References
1. Sharma T, Grewal J, Gupta S, Murray PI. Ophthalmic abdominal of acute leukaemias: the ophthalmologist's role. Eye (Lond). 2004; 18:663–72.2. Lin YC, Wang AG, Yen MY, Hsu WM. Leukaemic infiltration of the optic nerve as the initial manifestation of leukaemic relapse. Eye (Lond). 2004; 18:546–50.
Article3. Lee SY, Kim SH, Ha SG. Bilateral optic nerve involvement abdominal with unilateral facial palsy in a patient with acute myeloid leukaemia: a case report. Neuroophthalmology. 2017; 42:122–5.4. Park S, Park SK, Park TK. Leukemic infiltration of the optic nerve head as the initial manifestation of leukemic relapse. J Korean Ophthalmol Soc. 2011; 52:250–4.
Article5. Park YK, Jun RM, Ahn CS. A case of optic nerve infiltration of acute lymphocytic leukemia. J Korean Ophthalmol Soc. 2000; 41:2008–12.6. Kim JW, Baek CM, Kim KS. A case of chronic myelogenous leukemia involving retina and optic nerve. J Korean Ophthalmol Soc. 2003; 44:2687–93.7. Pui CH, Thiel E. Central nervous system disease in hematologic malignancies: historical perspective and practical applications. Semin Oncol. 2009; 36(4 Suppl 2):S2–16.
Article8. Castagnola C, Nozza A, Corso A, Bernasconi C. The value of abdominal therapy in adult acute myeloid leukemia with central abdominal system involvement. Haematologica. 1997; 82:577–80.9. Nikaido H, Mishima H, Ono H, et al. Leukemic involvement of the optic nerve. Am J Ophthalmol. 1988; 105:294–8.
Article10. Ranta S, Palomäki M, Levinsen M, et al. Role of neuroimaging in children with acute lymphoblastic leukemia and central nervous system involvement at diagnosis. Pediatr Blood Cancer. 2017; 64:64–70.
Article11. Okita Y, Narita Y, Miyakita Y, et al. abdominal follow-up of vanishing tumors in the brain: how should a lesion mimicking primary CNS lymphoma be managed? Clin Neurol Neurosurg. 2012; 114:1217–21.12. Barrantes-Freer A, Engel AS, Rodríguez-Villagra OA, et al. Diagnostic red flags: steroid-treated malignant CNS lymphoma mimicking autoimmune inflammatory demyelination. Brain Pathol. 2018; 28:225–33.
Article13. Shields JA, Stopyra GA, Marr BP, et al. Bilateral orbital myeloid sarcoma as initial sign of acute myeloid leukemia: case report and review of the literature. Arch Ophthalmol. 2003; 121:138–42.
Article14. Lee HS, Park JW, Yang SW. A case of granulocytic sarcoma involving the forniceal conjunctiva. J Korean Ophthalmol Soc. 2006; 47:986–90.15. Kim DJ, Chang MK. Case of acute myeloid leukemia with mass of eyelid and conjunctiva in the early stage. J Korean Ophthalmol Soc. 2016; 57:843–6.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Leukemic Infiltration of the Optic Nerve Head as the Initial Manifestation of Leukemic Relapse
- A Case of Optic Nerve Infiltration of Acute Lymphocytic Leukemia
- Enhancement of Optic Nerve in Leukemic Patients: Leukemic Infiltration of Optic Nerve versus Optic Neuritis
- A Case of Extramedullary Relapsed Acute Promyelocytic Leukemia Presenting as a Mass in the External Auditory Canal
- A Case of Temporal Bone Myeloid Sarcoma