Obstet Gynecol Sci.
2020 Mar;63(2):117-125. 10.5468/ogs.2020.63.2.117.
Determination of maternal risk factors of preterm delivery: adjusted for sparse data bias; results from a population-based case-control study in Iran
- Affiliations
-
- 1Department of Epidemiology, School of Public Health, Iran University of Medical Sciences, Tehran, Iran.
- 2Department of Communicable Disease Control and Prevention, Deputy of Health, Lorestan University of Medical Sciences, Khorramabad, Iran.
- 3Department of Community Medicine, School of Medicine, Zahedan University of Medical Sciences, Zahedan, Iran.
- 4Department of Epidemiology, School of Public Health, Iran University of Medical Sciences, Tehran, Iran.
- 5Lorestan University of Medical Sciences, Khorramabad, Iran.
- 6South Tehran Branch, Islamic Azad University, Tehran, Iran.
- 7Department of Nursing and Midwifery, Sanandaj Branch, Islamic Azad University, Sanandaj, Iran.
- 8Department of Biostatistics and Epidemiology, School of Medicine, Zanjan University of Medical Sciences, Zanjan, Iran. kamyarmansori@yahoo.com
- KMID: 2471748
- DOI: http://doi.org/10.5468/ogs.2020.63.2.117
Abstract
OBJECTIVE
To determine the maternal risk factors associated with preterm delivery in Iran.
METHODS
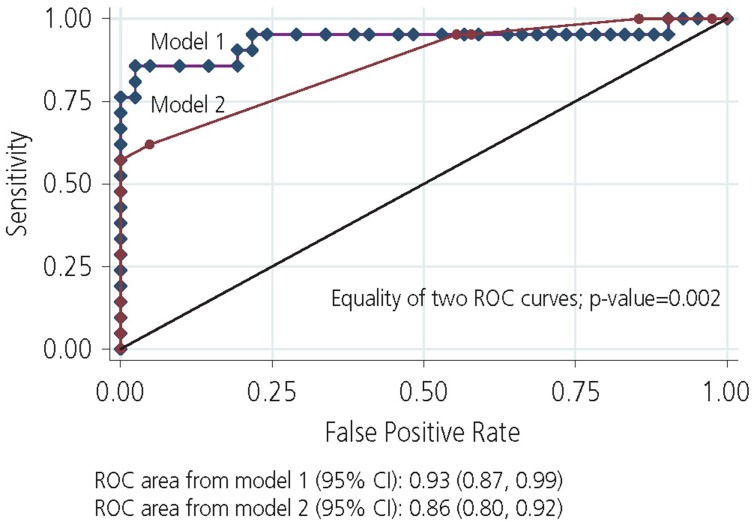
A population-based case-control study was conducted including 48 women having preterm delivery (case group) and 100 women having term delivery (control group) between March 2007 and March 2012 in the maternity hospitals of the Selseleh County, Lorestan province, Iran. Information regarding maternal risk factors was collected by structured interview and reviewing the medical records. The maternal risk factors associated with preterm delivery were identified using univariate and multivariable logistic regression analysis after adjusting the sparse data bias. The area under the receiver operating characteristic (ROC) curves was estimated to evaluate the discrimination power of the statistical models.
RESULTS
Multivariable analysis demonstrated that multiparty (odds ratio [OR], 14.23; 95% confidence interval [CI], 1.60-127.05), history of gestational diabetes (OR, 0.10; 95% CI, 0.01-0.99), thyroid dysfunction (OR, 97.32; 95% CI, 5.78-1,637.80), urinary tract infection (OR, 16.60; 95% CI, 3.20-85.92), and taking care during pregnancy (OR, 0.12; 95% CI, 0.03-0.50) had significant impact on preterm delivery after adjusting the potential confounders. The area under the ROC curve for the aforementioned maternal risk factors was 0.86 (95% CI, 0.80-0.92).
CONCLUSION
Our study provides evidence for the associations between multiparty, history of gestational diabetes, thyroid dysfunction, urinary tract infection, as well as taking care during pregnancy, and preterm delivery.
Keyword
MeSH Terms
Figure
Reference
-
1. Obstetrics Subgroup, Chinese Society of Obstetrics and Gynecology, Chinese Medical Association. Diagnosis and therapy guideline of preterm birth (2014). Zhonghua Fu Chan Ke Za Zhi. 2014; 49:481. PMID: 25327726.2. Simmons LE, Rubens CE, Darmstadt GL, Gravett MG. Preventing preterm birth and neonatal mortality: exploring the epidemiology, causes, and interventions. Semin Perinatol. 2010; 34:408–415. PMID: 21094415.
Article3. Goldenberg RL, Culhane JF, Iams JD, Romero R. Epidemiology and causes of preterm birth. Lancet. 2008; 371:75–84. PMID: 18177778.
Article4. Hamilton BE, Martin JA, Ventura SJ. Births: preliminary data for 2006. Natl Vital Stat Rep. 2007; 56:1–18.6. Hamilton BE, Ventura SJ. Births: preliminary data for 2005. Health E-Stats [Internet]. Hyattsville (MD): Centers for Disease Control and Prevention;2006. cited 2007 Jul 15. Available from: http://www.cdc.gov/nchs/products/pubs/pubd/hestats/prelimbirths05/prelimbirths05.htm.7. Hamilton BE, Kirmeyer SE. Trends and Variations in reproduction and intrinsic rates: United States, 1990-2014. Natl Vital Stat Rep. 2017; 66:1–14.8. Beck S, Wojdyla D, Say L, Betran AP, Merialdi M, Requejo JH, et al. The worldwide incidence of preterm birth: a systematic review of maternal mortality and morbidity. Bull World Health Organ. 2010; 88:31–38. PMID: 20428351.
Article9. Kamali Fard M, Alizadeh R, Sehati Shafaei F. The effect of lifestyle on the rate of preterm birth. J Ardabil Univ Med Sci. 2010; 10:55–63.10. Honest H, Bachmann LM, Sundaram R, Gupta JK, Kleijnen J, Khan KS. The accuracy of risk scores in predicting preterm birth--a systematic review. J Obstet Gynaecol. 2004; 24:343–359. PMID: 15203570.
Article11. Selling KE, Carstensen J, Finnström O, Sydsjö G. Intergenerational effects of preterm birth and reduced intrauterine growth: a population-based study of Swedish mother-offspring pairs. BJOG. 2006; 113:430–440. PMID: 16553655.
Article12. Langhoff-Roos J, Kesmodel U, Jacobsson B, Rasmussen S, Vogel I. Spontaneous preterm delivery in primiparous women at low risk in Denmark: population based study. BMJ. 2006; 332:937–939. PMID: 16497733.
Article13. Jiang M, Mishu MM, Lu D, Yin X. A case control study of risk factors and neonatal outcomes of preterm birth. Taiwan J Obstet Gynecol. 2018; 57:814–818. PMID: 30545533.
Article14. Zhang YP, Liu XH, Gao SH, Wang JM, Gu YS, Zhang JY, et al. Risk factors for preterm birth in five maternal and child health hospitals in Beijing. PLoS One. 2012; 7:e52780. PMID: 23300774.
Article15. Greenland S, Mansournia MA, Altman DG. Sparse data bias: a problem hiding in plain sight. BMJ. 2016; 352:i1981. PMID: 27121591.
Article16. Greenland S, Mansournia MA. Penalization, bias reduction, and default priors in logistic and related categorical and survival regressions. Stat Med. 2015; 34:3133–3143. PMID: 26011599.
Article17. Mohammadian S, Vakili M, Tabandeh A. Survey of related factors in prematurity birth. J Guilan Univ Med Sci. 2000; 9:117–122.18. Namakin K, Sharifzadeh G, Malekizadeh AJ. To identify the risk factors in prematurity birth in Birjand, Iran: a case-control study. Iran J Edpidemiol. 2011; 7:1–5.19. Heman ML, Albini M. Risk factors for spontaneous preterm birth among aboriginal and nonaboriginal women in Manitoba. J Obstet Gynecol. 2000; 90:43–49.20. Lotfalizadeh M, Mohammadzadeh A, Kamandi S, Bagheri S. Incidence and risk factors of preterm birth in Imam Reza hospital-2000-2001. J North Khorasan Univ Med Sci. 2005; 8:93–100.21. Zafarghandi N, Zafarghandi AS, Torkestani F, Fallah N, Jadidi F. Prevalence of risk factors for preterm birth. J Shahed Univ. 2004; 12:25–29.22. Rajaeefard A, Mohammadbeigi A, Mohammadi M, Jolaee H, Alipour H. Evaluation of risk factors in preterm delivery and impact of education in its prevention. Daneshvar Med. 2010; 17:11–18.23. Shoja M, Shoja E, Gharaei M. Prevalence and affecting factors on preterm birth in pregnant women Referred to Bentolhoda hospital-Bojnurd. J North Khorasan Univ Med Sci. 2016; 7:855–863.24. Jakobsson M, Gissler M, Sainio S, Paavonen J, Tapper AM. Preterm delivery after surgical treatment for cervical intraepithelial neoplasia. Obstet Gynecol. 2007; 109:309–313. PMID: 17267829.
Article25. Hedderson MM, Ferrara A, Sacks DA. Gestational diabetes mellitus and lesser degrees of pregnancy hyperglycemia: association with increased risk of spontaneous preterm birth. Obstet Gynecol. 2003; 102:850–856. PMID: 14551018.
Article26. Derakhshi B, Esmailnasab N, Ghaderi E, Hemmatpour S. Risk factor of preterm labor in the west of Iran: a case-control study. Iran J Public Health. 2014; 43:499–506. PMID: 26005661.27. Nabavizadeh SH, Malekzadeh M, Mousavizadeh A, Shirazi HR, Ghaffari P, Karshenas N, et al. Retrospective study of factors related to preterm labor in Yasuj, Iran. Int J Gen Med. 2012; 5:1013–1017. PMID: 23271920.28. Magee MS, Walden CE, Benedetti TJ, Knopp RH. Influence of diagnostic criteria on the incidence of gestational diabetes and perinatal morbidity. JAMA. 1993; 269:609–615. PMID: 8421365.
Article29. Tallarigo L, Giampietro O, Penno G, Miccoli R, Gregori G, Navalesi R. Relation of glucose tolerance to complications of pregnancy in nondiabetic women. N Engl J Med. 1986; 315:989–992. PMID: 3762619.
Article30. Stagnaro-Green A. Maternal thyroid disease and preterm delivery. J Clin Endocrinol Metab. 2009; 94:21–25. PMID: 18984665.
Article31. Casey BM, Dashe JS, Wells CE, McIntire DD, Byrd W, Leveno KJ, et al. Subclinical hypothyroidism and pregnancy outcomes. Obstet Gynecol. 2005; 105:239–245. PMID: 15684146.
Article32. Nazarpour S, Ramezani Tehrani F, Simbar M, Azizi F. Thyroid dysfunction and pregnancy outcomes. Iran J Reprod Med. 2015; 13:387–396. PMID: 26494985.33. Idris I, Srinivasan R, Simm A, Page RC. Maternal hypothyroidism in early and late gestation: effects on neonatal and obstetric outcome. Clin Endocrinol (Oxf). 2005; 63:560–565. PMID: 16268809.
Article34. Blazer S, Moreh-Waterman Y, Miller-Lotan R, Tamir A, Hochberg Z. Maternal hypothyroidism may affect fetal growth and neonatal thyroid function. Obstet Gynecol. 2003; 102:232–241. PMID: 12907094.
Article35. Romero R, Espinoza J, Kusanovic JP, Gotsch F, Hassan S, Erez O, et al. The preterm parturition syndrome. BJOG. 2006; 113(Suppl 3):17–42.
Article36. Goldenberg RL, Hauth JC, Andrews WW. Intrauterine infection and preterm delivery. N Engl J Med. 2000; 342:1500–1507. PMID: 10816189.
Article37. Srinivas SK, Ma Y, Sammel MD, Chou D, McGrath C, Parry S, et al. Placental inflammation and viral infection are implicated in second trimester pregnancy loss. Am J Obstet Gynecol. 2006; 195:797–802. PMID: 16949414.
Article38. Yadani S, Bouzari Z, Akhondi S. The comparison of the risk factors in the term and preterm delivery. J Babol Univ Med Sci. 2015; 17:7–12.39. Valadan M, Kaveh M, Bagherzadeh S, Hasanzade M. Risk factors for recurrent preterm delivery in three university hospitals. Tehran Univ Med J. 2008; 65:24–29.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Unexplained Elevated Levels Of Midtrimester Maternal Serum alpha-fetoprotein Are Associated With Spontaneous Preterm Birth
- Risk factors for maternal mortality in the west of Iran: a nested case-control study
- Obstetrical Management of Late Preterm Pregnancy
- A Study on Risk Factors of Preterm Delivery
- Association between assisted reproductive technology and autism spectrum disorders in Iran: a case-control study