A systematic review of the role of vitamin D and calcium in premenstrual syndrome
- Affiliations
-
- 1Student Research Committee, Nursing and Midwifery Faculty, Shahid Beheshti University of Medical Sciences, Tehran, Iran. F_rahnemaie@yahoo.com
- 2Department of Midwifery, Nursing and Midwifery Faculty, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
- KMID: 2471679
- DOI: http://doi.org/10.5468/ogs.2019.62.2.73
Abstract
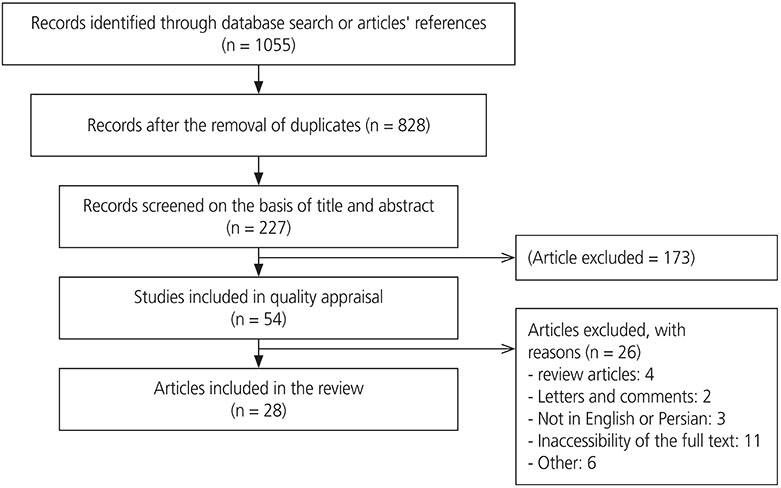
- Premenstrual syndrome (PMS) is a common disorder that affects millions of women of reproductive age worldwide. In recent years, there has been a focus on finding accessible, acceptable, and cost-effective therapeutic approaches with minimal side effects to treat the symptoms of PMS. This systematic review aimed to investigate the role of calcium and vitamin D in Premenstrual syndrome. The PubMed, EMBASE, Web of Science, Scopus, Science Direct, and Google Scholar databases were systematically searched for relevant articles from clinical trial, case-control, and cross-sectional studies. The Strengthening the Reporting of Observational Studies in Epidemiology checklist was used to assess the quality of the selected papers. A total of 28 eligible high-quality papers were reviewed. Low serum levels of calcium and vitamin D during the luteal phase of the menstrual cycle were found to cause or exacerbate the symptoms of PMS. Therefore, the administration of calcium and vitamin D supplements or the use of a diet rich in these two substances can restore serum levels and eliminate or reduce the symptoms of PMS. Calcium and vitamin D supplementation are recommended as an inexpensive, low-risk, acceptable, and accessible approach to eliminate or reduce the symptoms of PMS.
Keyword
MeSH Terms
Figure
Cited by 5 articles
-
Role of interleukin-6 (IL-6) in predicting gestational diabetes mellitus
Azam Amirian, Mahin Balouchi Mahani, Fatemeh Abdi
Obstet Gynecol Sci. 2020;63(4):407-416. doi: 10.5468/ogs.20020.Role of vitamin D and calcium in the relief of primary dysmenorrhea: a systematic review
Fatemeh Abdi, Marjan Akhavan Amjadi, Farzaneh Zaheri, Fatemeh Alsadat Rahnemaei
Obstet Gynecol Sci. 2021;64(1):13-26. doi: 10.5468/ogs.20205.Social determinants of domestic violence against suburban women in developing countries: a systematic review
Fatemeh Abdi, Zohreh Mahmoodi, Fatemeh Afsahi, Negin Shaterian, Fatemeh Alsadat Rahnemaei
Obstet Gynecol Sci. 2021;64(2):131-142. doi: 10.5468/ogs.20211.Social determinants of mental health of women living in slum: a systematic review
Fatemeh Abdi, Fatemeh Alsadat Rahnemaei, Parisa Shojaei, Fatemeh Afsahi, Zohreh Mahmoodi
Obstet Gynecol Sci. 2021;64(2):143-155. doi: 10.5468/ogs.20264.Vitamin D supplementation for primary dysmenorrhea: a double-blind, randomized, placebo-controlled trial
Fatemeh Alsadat Rahnemaei, Ali Gholamrezaei, Maryam Afrakhteh, Farid Zayeri, Mohammad Reza Vafa, Arian Rashidi, Giti Ozgoli
Obstet Gynecol Sci. 2021;64(4):353-363. doi: 10.5468/ogs.20316.
Reference
-
1. Abdnezhad R, Simbar M, Sheikhan Z, Mojab F, Nasiri M. The effect of Salvia (Sage) extract on the emotional symptoms of premenstrual syndrome. Iran J Obstet Gynecol Infertil. 2017; 20:84–94.2. Brahmbhatt S, Sattigeri BM, Shah H, Kumar A, Parikh D. A prospective survey study on premenstrual syndrome in young and middle aged women with an emphasis on its management. Int J Res Med Sci. 2013; 1:69–72.
Article3. Raval CM, Panchal BN, Tiwari DS, Vala AU, Bhatt RB. Prevalence of premenstrual syndrome and premenstrual dysphoric disorder among college students of Bhavnagar, Gujarat. Indian J Psychiatry. 2016; 58:164–170.
Article4. Halbreich U, O'Brien PM, Eriksson E, Bäckström T, Yonkers KA, Freeman EW. Are there differential symptom profiles that improve in response to different pharmacological treatments of premenstrual syndrome/premenstrual dysphoric disorder? CNS Drugs. 2006; 20:523–547.
Article5. Kahyaoglu Sut H, Mestogullari E. Effect of premenstrual syndrome on work-related quality of life in Turkish nurses. Saf Health Work. 2016; 7:78–82.
Article6. Sepehrirad M, Bahrami H, Noras M. The role of complementary medicine in control of premenstrual syndrome evidence based (Regular Review Study). Iran J Obstet Gynecol Infertil. 2016; 19:11–22.7. Freeman EW. Therapeutic management of premenstrual syndrome. Expert Opin Pharmacother. 2010; 11:2879–2889.
Article8. World Health Organization. National policy on traditional medicine and regulation of herbal medicines: report of a WHO global survey. Geneva: World Health Organization;2005.9. Babazadeh R, Keramat A. Premenstrual syndrome and complementary medicine in Iran: a systematic review. Feyz J Kashan Univ Med Sci. 2011; 15:174–187.10. Mun MJ, Kim TH, Hwang JY, Jang WC. Vitamin D receptor gene polymorphisms and the risk for female reproductive cancers: a meta-analysis. Maturitas. 2015; 81:256–265.
Article11. Kim TH, Lee HH, Kim JM, Lee A, Park J, Kim Y. A comparison in vitamin D receptor expression during oral menopausal hormone therapy and vaginal estrogen therapy. Clin Exp Obstet Gynecol. 2018; 45:39–43.12. Cioni F, Ferraroni F. Vitamin D and other nutrients in the treatment of premenstrual syndrome. In : Hollins-Martin C, van den Akker O, Martin C, Preedy VR, editors. Handbook of diet and nutrition in the menstrual cycle, periconception and fertility. Wageningen: Wageningen Academic Publishers;2014. p. 121–136.13. Lee A, Lee MR, Lee HH, Kim YS, Kim JM, Enkhbold T, et al. Vitamin D proliferates vaginal epithelium through RhoA expression in postmenopausal atrophic vagina tissue. Mol Cells. 2017; 40:677–684.
Article14. Taghizadeh Z, Shirmohammadi M, Feizi A, Arbabi M. The effect of cognitive behavioural psycho-education on premenstrual syndrome and related symptoms. J Psychiatr Ment Health Nurs. 2013; 20:705–713.
Article15. Sen AP, Gulati A. Use of magnesium in traumatic brain injury. Neurotherapeutics. 2010; 7:91–99.
Article16. Sharma G, Tandon P. Luteal phase serum calcium and serum magnesium levels in causation of premenstrual syndrome. Int J Basic Appl Physiol. 2015; 4:126–130.17. Vaidya A, Forman JP. Vitamin D and vascular disease: the current and future status of vitamin D therapy in hypertension and kidney disease. Curr Hypertens Rep. 2012; 14:111–119.
Article18. Forman JP, Williams JS, Fisher ND. Plasma 25-hydroxyvitamin D and regulation of the renin-angiotensin system in humans. Hypertension. 2010; 55:1283–1288.
Article19. Pambudi MF. Calcium level is lower in women with premenstrual syndrome. Majalah Obstet Ginekol Indones. 2013; 37:99–102.20. Rajaei S, Akbari Sene A, Norouzi S, Berangi Y, Arabian S, Lak P, et al. The relationship between serum vitamin D level and premenstrual syndrome in Iranian women. Int J Reprod Biomed (Yazd). 2016; 14:665–668.
Article21. Bahrami A, Bahrami-Taghanaki H, Afkhamizadeh M, Avan A, Mazloum Khorasani Z, Esmaeili H, et al. Menstrual disorders and premenstrual symptoms in adolescents: prevalence and relationship to serum calcium and vitamin D concentrations. J Obstet Gynaecol. 2018; 38:989–995.
Article22. Bertone-Johnson ER, Hankinson SE, Bendich A, Johnson SR, Willett WC, Manson JE. Calcium and vitamin D intake and risk of incident premenstrual syndrome. Arch Intern Med. 2005; 165:1246–1252.
Article23. Lo CK, Mertz D, Loeb M. Newcastle-Ottawa Scale: comparing reviewers' to authors' assessments. BMC Med Res Methodol. 2014; 14:45.
Article24. Roozbeh N, Banihashemi F, Mehraban M, Abdi F. Potential role of Factor V Leiden mutation in adverse pregnancy outcomes: an updated systematic review. Biomed Res Ther. 2017; 4:1832–1846.
Article25. Bahrami A, Avan A, Sadeghnia HR, Esmaeili H, Tayefi M, Ghasemi F, et al. High dose vitamin D supplementation can improve menstrual problems, dysmenorrhea, and premenstrual syndrome in adolescents. Gynecol Endocrinol. 2018; 34:659–663.
Article26. Dadkhah H, Ebrahimi E, Fathizadeh N. Evaluating the effects of vitamin D and vitamin E supplement on premenstrual syndrome: a randomized, double-blind, controlled trial. Iran J Nurs Midwifery Res. 2016; 21:159–164.27. Ghanbari Z, Haghollahi F, Shariat M, Foroshani AR, Ashrafi M. Effects of calcium supplement therapy in women with premenstrual syndrome. Taiwan J Obstet Gynecol. 2009; 48:124–129.
Article28. Karimi Z, Dehkordi MA, Alipour A, Mohtashami T. Treatment of premenstrual syndrome: appraising the effectiveness of cognitive behavioral therapy in addition to calcium supplement plus vitamin D. PsyCh J. 2018; 7:41–50.
Article29. Kermani AZ, Taavoni S, Hosseini AF. Effect of combined calcium and vitamin E consumption on premenstrual syndrome. Iran J Nurs. 2010; 23:8–14.30. Khajehei M, Abdali K, Parsanezhad ME, Tabatabaee HR. Effect of treatment with dydrogesterone or calcium plus vitamin D on the severity of premenstrual syndrome. Int J Gynaecol Obstet. 2009; 105:158–161.
Article31. Mandana Z, Azar A. Comparison of the effect of vit E, vitB6, calcium and omega-3 on the treatment of premenstrual syndrome: a clinical randomized trial. Annu Res Rev Biol. 2014; 4:1141–1149.
Article32. Samieipour S, Kiani F, Samiei Pour Y, Babaei Heydarabadi A, Tavassoli E, Rahim Zade R. Comparing the effects of vitamin B1 and calcium on premenstrual syndrome (PMS) among female students, Ilam-Iran. Int J Pediatr. 2016; 4:3519–3528.33. Samieipour S, Tavassoli E, Heydarabadi B, Daniali SS, Alidosti M, Kiani F, et al. Effect of calcium and vitamin B1 on the severity of premenstrual syndrome: a randomized control trial. Int J Pharm Technol. 2016; 8:18706–18717.34. Shehata NA. Calcium versus oral contraceptive pills containing drospirenone for the treatment of mild to moderate premenstrual syndrome: a double blind randomized placebo controlled trial. Eur J Obstet Gynecol Reprod Biol. 2016; 198:100–104.35. Shobeiri F, Araste FE, Ebrahimi R, Jenabi E, Nazari M. Effect of calcium on premenstrual syndrome: a double-blind randomized clinical trial. Obstet Gynecol Sci. 2017; 60:100–105.
Article36. Shobeiri F, Ezzati Arasteh F, Ebrahimi R, Nazari M.. Effect of calcium on physical symptoms of premenstrual syndrome. Iran J Obstet Gynecol Infertil. 2016; 19:1–8.37. Sutariya S, Talsania N, Shah C, Patel M. An interventional study (calcium supplementation & health education) on premenstrual syndrome - effect on premenstrual and menstrual symptoms. Natl J Community Med. 2011; 2:100–104.38. Tartagni M, Cicinelli MV, Tartagni MV, Alrasheed H, Matteo M, Baldini D, et al. Vitamin D supplementation for premenstrual syndrome-related mood disorders in adolescents with severe hypovitaminosis D. J Pediatr Adolesc Gynecol. 2016; 29:357–361.
Article39. Yonkers KA, Pearlstein TB, Gotman N. A pilot study to compare fluoxetine, calcium, and placebo in the treatment of premenstrual syndrome. J Clin Psychopharmacol. 2013; 33:614–620.
Article40. Akhlaghi F, Hamedi A, Javadi Z, Hosseinipoor F. Effects of calcium supplementation on premenstrual syndrome. Razi J Med Sci. 2004; 10:669–675.41. Bharati M. Comparing the effects of yoga & oral calcium administration in alleviating symptoms of premenstrual syndrome in medical undergraduates. J Caring Sci. 2016; 5:179–185.42. Bertone-Johnson ER, Chocano-Bedoya PO, Zagarins SE, Micka AE, Ronnenberg AG. Dietary vitamin D intake, 25-hydroxyvitamin D3 levels and premenstrual syndrome in a college-aged population. J Steroid Biochem Mol Biol. 2010; 121:434–437.
Article43. Mortola JF, Girton L, Beck L, Yen SS. Diagnosis of premenstrual syndrome by a simple, prospective, and reliable instrument: the calendar of premenstrual experiences. Obstet Gynecol. 1990; 76:302–307.
Article44. Obeidat BA, Alchalabi HA, Abdul-Razzak KK, Al-Farras MI. Premenstrual symptoms in dysmenorrheic college students: prevalence and relation to vitamin D and parathyroid hormone levels. Int J Environ Res Public Health. 2012; 9:4210–4222.
Article45. Abbasi ST, Abbasi P, Suhag AH, Qureshi MA. Serum magnesium and 25-hydroxy cholecalciferol in premenstrual syndrome during luteal phase. J Liaquat Uni Med Health Sci. 2017; 16:209–212.
Article46. Ghalwa NA, Qedra R, Wahedy K. Impact of calcium and magnesium dietary changes on women pain and discomfort from premenstrual syndrome at the Faculty of Pharmacy-Gaza strip. World J Pharm Pharm Sci. 2014; 3:981–1005.47. Saeedian Kia A, Amani R, Cheraghian B. The association between the risk of premenstrual syndrome and vitamin D, calcium, and magnesium status among university students: a case control study. Health Promot Perspect. 2015; 5:225–230.
Article48. Bertone-Johnson ER, Hankinson SE, Forger NG, Powers SI, Willett WC, Johnson SR, et al. Plasma 25-hydroxyvitamin D and risk of premenstrual syndrome in a prospective cohort study. BMC Womens Health. 2014; 14:56.
Article49. American College of Obstetricians and Gynecologists. Frequently asked questions FAQ057: gynecologic problems: premenstrual syndrome. Washington, D.C.: American College of Obstetricians and Gynecologists;2011.50. Thys-Jacobs S, McMahon D, Bilezikian JP. Cyclical changes in calcium metabolism across the menstrual cycle in women with premenstrual dysphoric disorder. J Clin Endocrinol Metab. 2007; 92:2952–2959.
Article51. Eyles DW, Burne TH, McGrath JJ. Vitamin D, effects on brain development, adult brain function and the links between low levels of vitamin D and neuropsychiatric disease. Front Neuroendocrinol. 2013; 34:47–64.
Article52. Skowrońska P, Pastuszek E, Kuczyński W, Jaszczoł M, Kuć P, Jakiel G, et al. The role of vitamin D in reproductive dysfunction in women - a systematic review. Ann Agric Environ Med. 2016; 23:671–676.53. Miyashita M, Koga K, Izumi G, Sue F, Makabe T, Taguchi A, et al. Effects of 1, 25-dihydroxy vitamin D3 on endometriosis. J Clin Endocrinol Metab. 2016; 101:2371–2379.54. Harris HR, Chavarro JE, Malspeis S, Willett WC, Missmer SA. Dairy-food, calcium, magnesium, and vitamin D intake and endometriosis: a prospective cohort study. Am J Epidemiol. 2013; 177:420–430.
Article55. Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, et al. Guidelines for preventing and treating vitamin D deficiency and insufficiency revisited. J Clin Endocrinol Metab. 2012; 97:1153–1158.
Article56. Bertone-Johnson ER. Vitamin D and the occurrence of depression: causal association or circumstantial evidence? Nutr Rev. 2009; 67:481–492.
Article57. Holick MF. Vitamin D: a D-Lightful health perspective. Nutr Rev. 2008; 66:S182–94.
Article58. Thys-Jacobs S. Micronutrients and the premenstrual syndrome: the case for calcium. J Am Coll Nutr. 2000; 19:220–227.
Article59. Bendich A. The potential for dietary supplements to reduce premenstrual syndrome (PMS) symptoms. J Am Coll Nutr. 2000; 19:3–12.
Article60. Bohrer T, Krannich JH. Depression as a manifestation of latent chronic hypoparathyroidism. World J Biol Psychiatry. 2007; 8:56–59.
Article61. Faghih S, Abdolahzadeh M, Mohammadi M, Hasanzadeh J. Prevalence of vitamin d deficiency and its related factors among university students in Shiraz, Iran. Int J Prev Med. 2014; 5:796–799.62. Kaykhaei MA, Hashemi M, Narouie B, Shikhzadeh A, Rashidi H, Moulaei N, et al. High prevalence of vitamin D deficiency in Zahedan, southeast Iran. Ann Nutr Metab. 2011; 58:37–41.
Article63. Hovsepian S, Amini M, Aminorroaya A, Amini P, Iraj B. Prevalence of vitamin D deficiency among adult population of Isfahan City, Iran. J Health Popul Nutr. 2011; 29:149–155.
Article64. Halbreich U. Selective serotonin reuptake inhibitors and initial oral contraceptives for the treatment of PMDD: effective but not enough. CNS Spectr. 2008; 13:566–572.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Correction of the name of author: A systematic review of the role of vitamin D and calcium in premenstrual syndrome
- A Study of Nutritional Intakes, Food Preference and Blood Composition in Female College Students with Premenstrual Syndrome
- Cardiovascular Impact of Calcium and Vitamin D Supplements: A Narrative Review
- Vitamin D and atopic dermatitis
- Premenstrual syndrome & premenstrual dysphoric disorder