J Korean Acad Nurs.
2020 Feb;50(1):147-157. 10.4040/jkan.2020.50.1.147.
Menstrual Cycle Characteristics and Premenstrual Syndrome Prevalence Based on the Daily Record of Severity of Problems in Korean Young Adult Women
- Affiliations
-
- 1Health Insurance Review & Assessment Service, Seoul, Korea.
- 2College of Nursing, Korea University, Seoul, Korea. yjpark@korea.ac.kr
- KMID: 2471257
- DOI: http://doi.org/10.4040/jkan.2020.50.1.147
Abstract
- PURPOSE
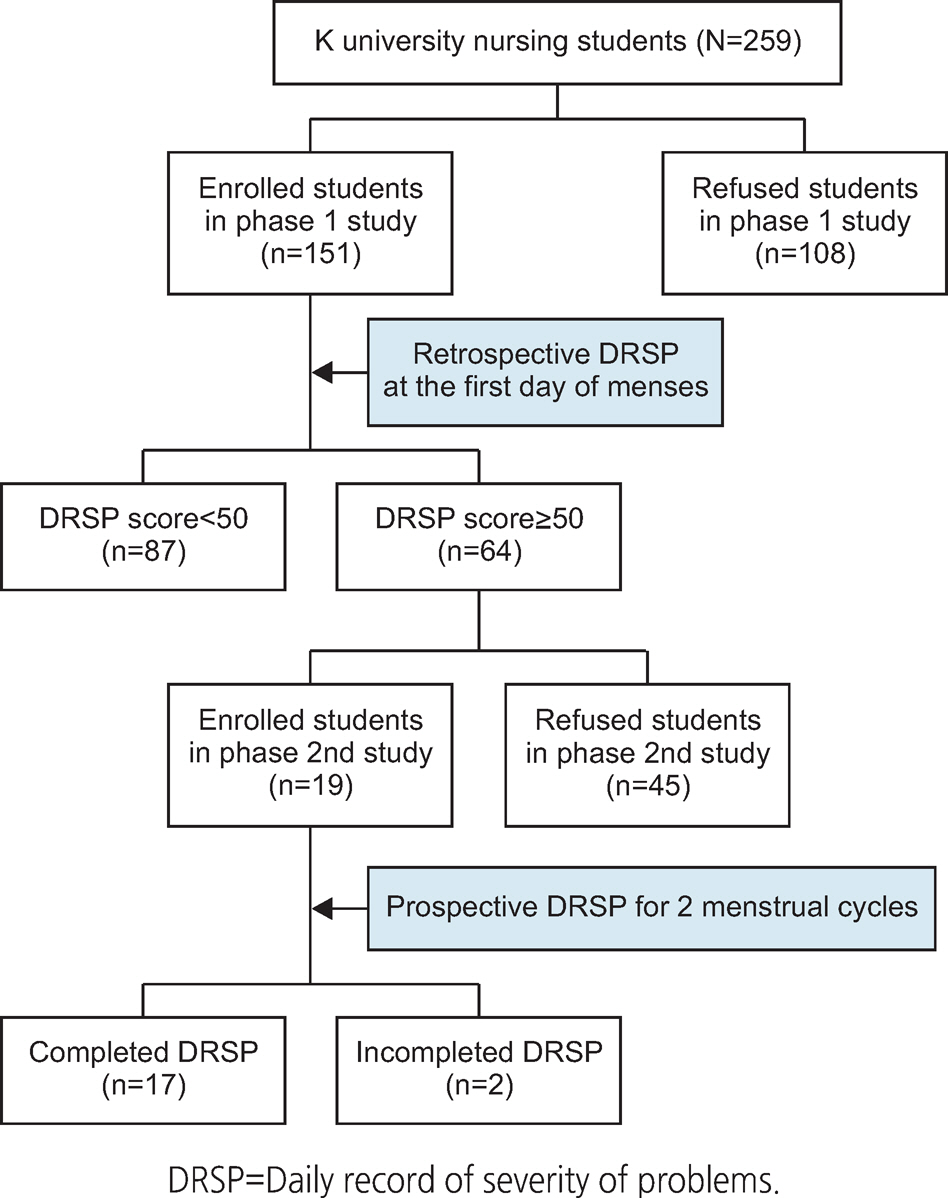
This descriptive study aimed to identify the menstrual cycle characteristics and premenstrual syndrome (PMS) prevalence in Korean young adult women using the retrospective and prospective Daily Record of Severity of Problems (DRSP).
METHODS
In the first stage, participants included 151 nursing students studying in a university located in Seoul. Data were collected from April 20 to June 2, 2017, using the questionnaire on menstrual characteristics, pictorial blood assessment chart, and retrospective DRSP. In the second stage, participants included 17 students with PMS, based on the screening conducted in the first stage. Data were collected using the prospective DRSP from May 29 to 2 September 2, 2017.
RESULTS
Of the study sample, 104 participants (68.9%) had regular periods. Those with regular periods had 11.97 periods annually with a menstrual cycle of 29.38 days and a period duration of 5.72 days. Fifty-five participants (37.4%) showed menorrhagia. Sixty-four participants (42.4%) were found to have PMS based on their retrospective DRSP. When the ratio of women (52.9%) with PMS shown in the prospective DRSP was used as a positive predictive value, the estimated PMS prevalence was 22.4%.
CONCLUSION
This study provides clinically significant PMS prevalence among Korean young adult women, positive predictive value of the retrospective DRSP, and valid data to basically understand the menstrual cycle characteristics experienced by these women.
Keyword
MeSH Terms
Figure
Reference
-
1. Kadian, S. O’Brien S. Classification of premenstrual disorders as proposed by the International Society for Premenstrual Disorders. Menopause International. 2012; 18(2):43–47. https://doi.org/10.1258/mi.2012.012017.2. Dennerstein L, Lehert P, Heinemann K. Epidemiology of premenstrual symptoms and disorders. Menopause International. 2012; 18(2):48–51. https://doi.org/10.1258/mi.2012.012013.
Article3. Dean BB, Borenstein JE, Knight K, Yonkers K. Evaluating the criteria used for identification of PMS. Journal of Women’s Health. 2006; 15(5):546–555. https://doi.org/10.1089/jwh.2006.15.546.
Article4. Direkvand-Moghadam A, Sayehmiri K, Delpisheh A, Kaikha-vandi S. Epidemiology of premenstrual syndrome (PMS)-a systematic review and meta-analysis study. Journal of Clinical and Diagnostic Research. 2014; 8(2):106–109. https://doi.org/10.7860/JCDR/2014/8024.4021.5. Steiner M, Macdougall M, Brown E. The premenstrual symptoms screening tool (PSST) for clinicians. Archives of Women’s Mental Health. 2003; 6(3):203–209. https://doi.org/10.1007/s00737-003-0018-4.
Article6. Borenstein JE, Dean BB, Yonkers KA, Endicott J. Using the daily record of severity of problems as a screening instrument for premenstrual syndrome. Obstetrics and Gynecology. 2007; 109(5):1068–1075. https://doi.org/10.1097/01.AOG.0000259920.73000.3b.
Article7. Ryu A, Kim TH. Premenstrual syndrome: A mini review. Ma-turitas. 2015; 82(4):436–440. https://doi.org/10.1016/j.maturitas.2015.08.010.
Article8. Nevatte T, O’Brien PMS, Bäckström T, Brown C, Dennerstein L, Endicott J, et al. ISPMD consensus on the management of premenstrual disorders. Archives of Women’s Mental Health. 2013; 16(4):279–291. https://doi.org/10.1007/s00737-013-0346-y.
Article9. Biggs WS, Demuth RH. Premenstrual syndrome and premenstrual dysphoric disorder. American Family Physician. 2011; 84(8):918–924.10. Henz A, Ferreira CF, Oderich CL, Gallon CW, Castro JRS, Conzatti M, et al. Premenstrual syndrome diagnosis: A comparative study between the daily record of severity of problems (DRSP) and the premenstrual symptoms screening tool (PSST). Revista Brasileira de Ginecologia e Obstetricia. 2018; 40(1):20–25. https://doi.org/10.1055/s-0037-1608672.
Article11. Endicott J, Nee J, Harrison W. Daily record of severity of problems (DRSP): Reliability and validity. Archives of Women’s Mental Health. 2006; 9(1):41–49. https://doi.org/10.1007/s00737-005-0103-y.
Article12. Higham JM, O’Brien PM, Shaw RW. Assessment of menstrual blood loss using a pictorial chart. British Journal of Obstetrics and Gynaecology. 1990; 97(8):734–739. https://doi.org/10.1111/j.1471-0528.1990.tb16249.x.
Article13. Ahn JH, Lim SW, Song BS, Seo J, Lee JA, Kim DH, et al. Age at menarche in the Korean female: Secular trends and relationship to adulthood body mass index. Annals of Pediatric Endocrinology and Metabolism. 2013; 18(2):60–64. https://doi.org/10.6065/apem.2013.18.2.60.
Article14. Lee JC, Yu BK, Byeon JH, Lee KH, Min JH, Park SH. A study on the menstruation of Korean adolescent girls in Seoul. Kore- an Journal of Pediatrics. 2011; 54(5):201–206. https://doi.org/10.3345/kjp.2011.54.5.201.
Article15. Hahn KA, Wise LA, Riis AH, Mikkelsen EM, Rothman KJ, Banholzer K, et al. Correlates of menstrual cycle characteristics among nulliparous Danish women. Clinical Epidemiology. 2013; 5:311–319. https://doi.org/10.2147/CLEP.S46712.
Article16. Rigon F, De Sanctis V, Bernasconi S, Bianchin L, Bona G, Bozzola M, et al. Menstrual pattern and menstrual disorders among adolescents: An update of the Italian data. Italian Journal of Pediatrics. 2012; 38:38. https://doi.org/10.1186/1824-7288-38-38.
Article17. Kumar D, Goel NK, Puri S, Pathak R, Sarpal SS, Gupta S, et al. Menstrual pattern among unmarried women from Northern India. Journal of Clinical and Diagnostic Research. 2013; 7(9):1926–1929. https://doi.org/10.7860/JCDR/2013/6702.3359.18. Jung EK, Kim SW, Ock SM, Jung KI, Song CH. Prevalence and related factors of irregular menstrual cycles in Korean women: The 5th Korean national health and nutrition examination survey (KNHANES-V, 2010-2012). Journal of Psychosomatic Obstetrics and Gynecology. 2018; 39(3):196–202. https://doi.org/10.1080/0167482X.2017.1321631.
Article19. Jung AN, Park JH, Kim J, Kim SH, Jee BC, Cha BH, et al. Detrimental effects of higher body mass index and smoking habits on menstrual cycles in Korean women. Journal of Women’s Health. 2017; 26(1):83–90. https://doi.org/10.1089/jwh.2015.5634.
Article20. Chung SH, Kim TH, Lee HH, Lee A, Jeon DS, Park J, et al. Premenstrual syndrome and premenstrual dysphoric disorder in perimenopausal women. Journal of Menopausal Medicine. 2014; 20(2):69–74. https://doi.org/10.6118/jmm.2014.20.2.69.
Article21. Kwak Y, Kim Y, Baek KA. Prevalence of irregular menstruation according to socioeconomic status: A population-based nationwide cross-sectional study. PLoS One. 2019; 14(3):e0214071. https://doi.org/10.1371/journal.pone.0214071.
Article22. Gursel T, Biri A, Kaya Z, Sivaslıoglu S, Albayrak M. The frequency of menorrhagia and bleeding disorders in university students. Pediatric Hematology and Oncology. 2014; 31(5):467–474. https://doi.org/10.3109/08880018.2014.886316.
Article23. Bahrami A, Bahrami-Taghanaki H, Afkhamizadeh M, Avan A, Mazloum Khorasani Z, Esmaeili H, et al. Menstrual disorders and premenstrual symptoms in adolescents: Prevalence and relationship to serum calcium and vitamin D concentrations. Journal of Obstetrics and Gynaecology. 2018; 38(7):989–995. https://doi.org/10.1080/01443615.2018.1434764.
Article24. Tolossa FW, Bekele ML. Prevalence, impacts and medical managements of premenstrual syndrome among female students: Cross-sectional study in College of Health Sciences, Mekelle University, Mekelle, Northern Ethiopia. BMC Women’s Health. 2014; 14:52. https://doi.org/10.1186/1472-6874-14-52.
Article25. Qiao M, Zhang H, Liu H, Luo S, Wang T, Zhang J, et al. Prevalence of premenstrual syndrome and premenstrual dysphoric disorder in a population-based sample in China. European Journal of Obstetrics, Gynecology and Reproductive Biology. 2012; 162(1):83–86. https://doi.org/10.1016/j.ejogrb.2012.01.017.
Article26. Farrokh-Eslamlou H, Oshnouei S, Heshmatian B, Akbari E. Premenstrual syndrome and quality of life in Iranian medical students. Sexual and Reproductive Healthcare. 2015; 6(1):23–27. https://doi.org/10.1016/j.srhc.2014.06.009.
Article27. Bertone-Johnson ER, Whitcomb BW, Rich-Edwards JW, Hankinson SE, Manson JE. Premenstrual syndrome and subsequent risk of hypertension in a prospective study. American Journal of Epidemiology. 2015; 182(12):1000–1009. https://doi.org/10.1093/aje/kwv159.
Article28. Jane ZY, Chang CC, Lin HK, Liu YC, Chen WL. The association between the exacerbation of irritable bowel syndrome and menstrual symptoms in young Taiwanese women. Gastroenterology Nursing. 2011; 34(4):277–286. https://doi.org/10.1097/SGA.0b013e3182248708.
Article29. Ducasse D, Jaussent I, Olié E, Guillaume S, Lopez-Castroman J, Courtet P. Personality traits of suicidality are associated with premenstrual syndrome and premenstrual dysphoric disorder in a suicidal women sample. PLoS One. 2016; 11(2):e0148653. https://doi.org/10.1371/journal.pone.0148653.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Menstruation and Sleep
- Vulnerability to Minor Stressful Events in Young Women with Premenstrual Syndrome
- Premenstrual Symptom Patterns and Coping Style in Women with Premenstrual Change
- Effect of calcium on premenstrual syndrome: A double-blind randomized clinical trial
- Dysmenorrhea and Premenstrual Syndrome of School Girls in Ansan