Allergy Asthma Immunol Res.
2020 May;12(3):507-522. 10.4168/aair.2020.12.3.507.
Role of IL-17A in Chronic Rhinosinusitis With Nasal Polyp
- Affiliations
-
- 1Department of Otorhinolaryngology-Head and Neck Surgery, Soonchunhyang University College of Medicine, Cheonan, Korea.
- 2Department of Otorhinolaryngology, Dankook University College of Medicine, Cheonan, Korea. jihunmo@gmail.com
- 3Beckman Laser Institute Korea, Dankook University College of Medicine, Cheonan, Korea.
- KMID: 2471233
- DOI: http://doi.org/10.4168/aair.2020.12.3.507
Abstract
- PURPOSE
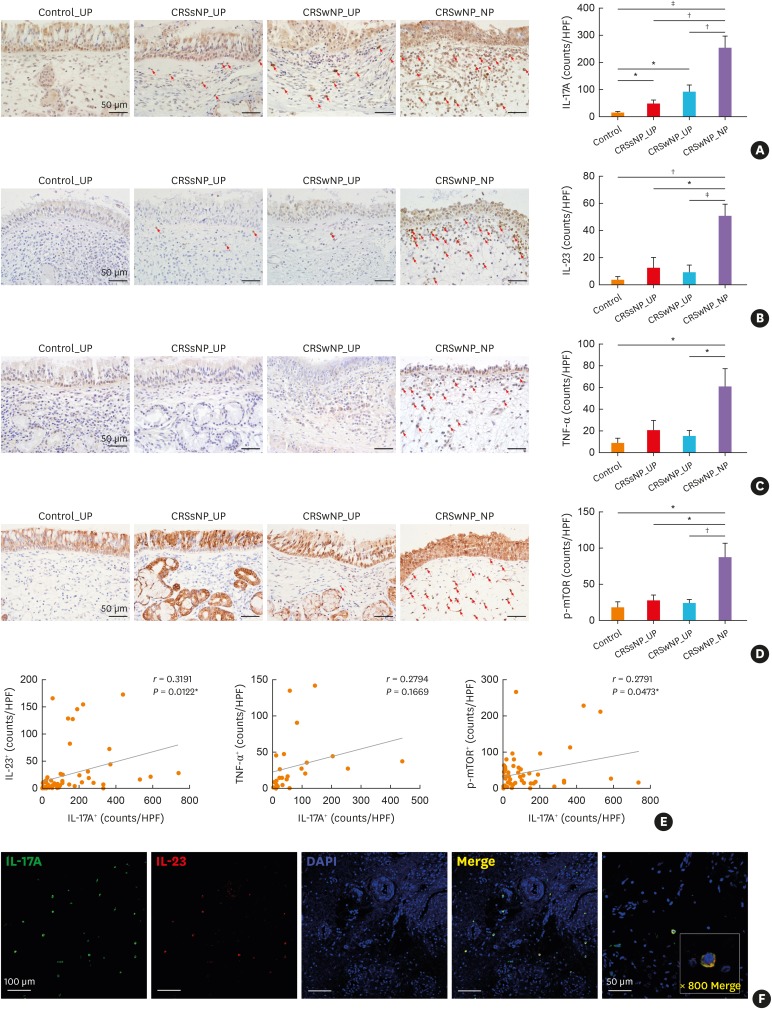
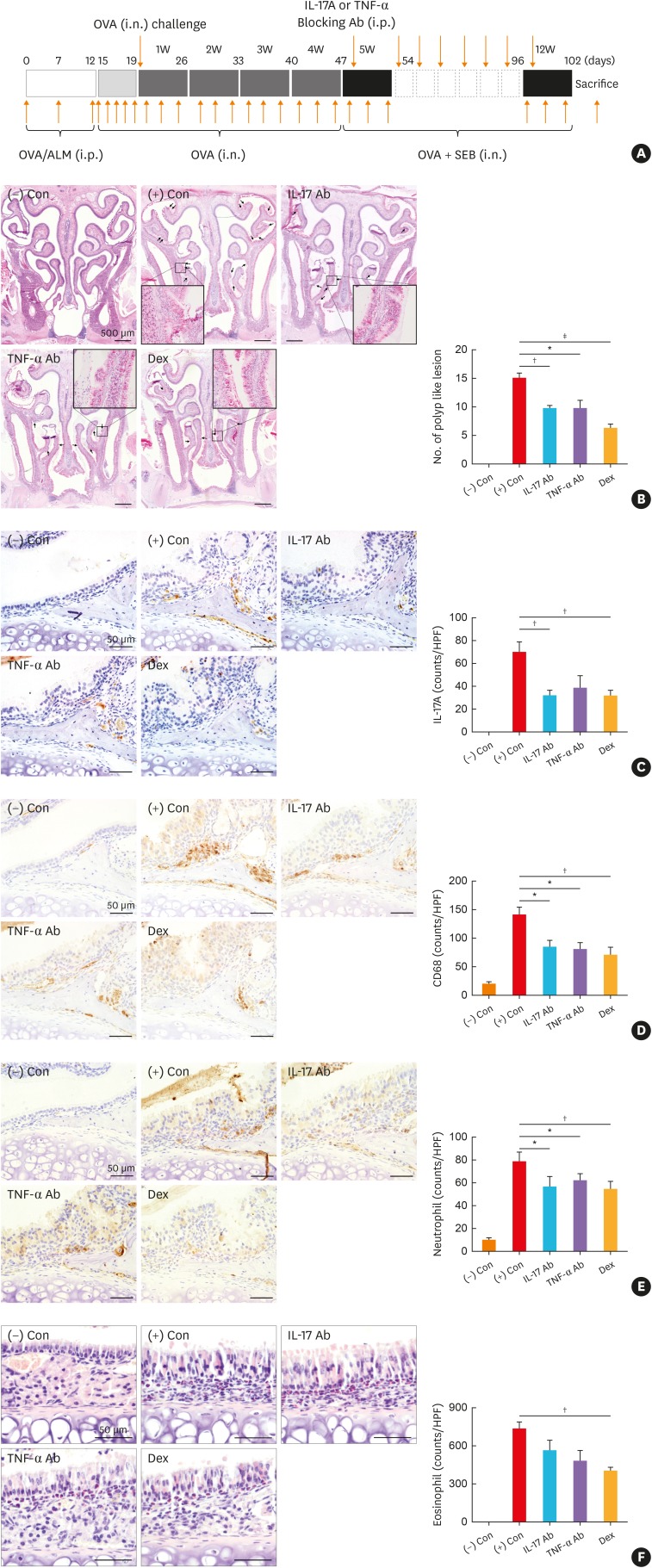
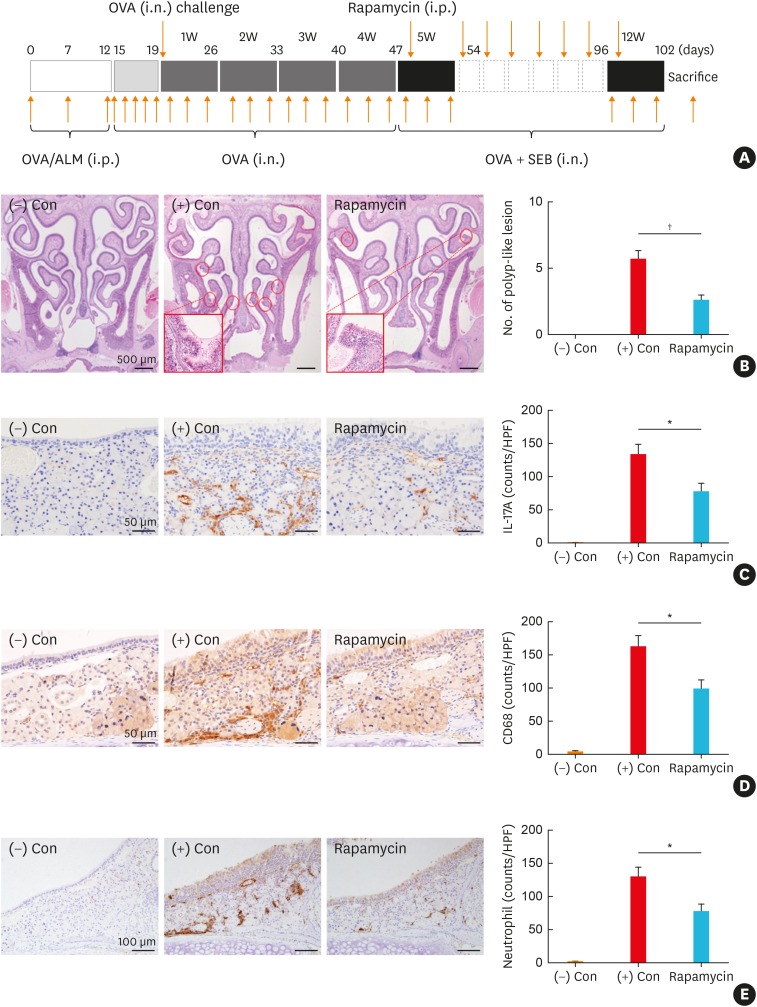
Th17-associated inflammation is increased in chronic rhinosinusitis with nasal polyp (CRSwNP), and is associated with disease severity and steroid resistance. Overexpressed interleukin (IL)-17A affects CRSwNP by tissue remodeling, eosinophilic accumulation, and neutrophilic infiltration. We aimed to identify the role of IL-17A in CRSwNP and to evaluate the effects of anti-IL-17A blocking antibody on nasal polyp (NP) formation using a murine NP model. Moreover, we sought to investigate whether the inhibition of mechanistic target of the rapamycin (mTOR) signal pathway could suppress IL-17A expression and NP formation.
METHODS
Human sinonasal tissues from control subjects and patients with chronic rhinosinusitis (CRS) were analyzed using immunohistochemistry (IHC) and immunofluorescence staining. The effects of IL-17A neutralizing antibody and rapamycin were evaluated in a murine NP model. Mouse samples were analyzed using IHC, quantitative real-time polymerase chain reaction, and enzyme-linked immunosorbent assay.
RESULTS
IL-17A+ inflammatory cells were significantly increased in number in NP from patients with CRSwNP compared to that in uncinate process tissues from control subjects and patients with CRS without NP or CRSwNP. CD68+ M1 macrophages dominantly expressed IL-17A, followed by neutrophils and T helper cells, in NP tissues. Neutralization of IL-17A effectively reduced the number of NPs, inflammatory cytokines, and IL-17A-producing cells, including M1 macrophages. Inhibition of IL-17A via the mTOR pathway using rapamycin also attenuated NP formation and inflammation in the murine NP model.
CONCLUSIONS
IL-17A possibly plays a role in the pathogenesis of CRSwNP, the major cellular source being M1 macrophage in NP tissues. Targeting IL-17A directly or indirectly may be an effective therapeutic strategy for CRSwNP.
Keyword
MeSH Terms
-
Animals
Antibodies, Neutralizing
Cytokines
Enzyme-Linked Immunosorbent Assay
Eosinophils
Fluorescent Antibody Technique
Humans
Immunohistochemistry
Inflammation
Interleukin-17*
Interleukins
Macrophages
Mice
Nasal Polyps*
Neutrophils
Real-Time Polymerase Chain Reaction
Signal Transduction
Sinusitis
Sirolimus
T-Lymphocytes, Helper-Inducer
Antibodies, Neutralizing
Cytokines
Interleukin-17
Interleukins
Sirolimus
Figure
Reference
-
1. Tomassen P, Vandeplas G, Van Zele T, Cardell LO, Arebro J, Olze H, et al. Inflammatory endotypes of chronic rhinosinusitis based on cluster analysis of biomarkers. J Allergy Clin Immunol. 2016; 137:1449–1456.e4. PMID: 26949058.
Article2. Zhang N, Van Zele T, Perez-Novo C, Van Bruaene N, Holtappels G, DeRuyck N, et al. Different types of T-effector cells orchestrate mucosal inflammation in chronic sinus disease. J Allergy Clin Immunol. 2008; 122:961–968. PMID: 18804271.
Article3. Wang X, Zhang N, Bo M, Holtappels G, Zheng M, Lou H, et al. Diversity of TH cytokine profiles in patients with chronic rhinosinusitis: a multicenter study in Europe, Asia, and Oceania. J Allergy Clin Immunol. 2016; 138:1344–1353. PMID: 27544740.4. Derycke L, Eyerich S, Van Crombruggen K, Pérez-Novo C, Holtappels G, Deruyck N, et al. Mixed T helper cell signatures in chronic rhinosinusitis with and without polyps. PLoS One. 2014; 9:e97581. PMID: 24911279.
Article5. Ghoreschi K, Laurence A, Yang XP, Tato CM, McGeachy MJ, Konkel JE, et al. Generation of pathogenic TH17 cells in the absence of TGF-β signalling. Nature. 2010; 467:967–971. PMID: 20962846.6. Annunziato F, Cosmi L, Santarlasci V, Maggi L, Liotta F, Mazzinghi B, et al. Phenotypic and functional features of human Th17 cells. J Exp Med. 2007; 204:1849–1861. PMID: 17635957.
Article7. Bettelli E, Oukka M, Kuchroo VK. TH-17 cells in the circle of immunity and autoimmunity. Nat Immunol. 2007; 8:345–350. PMID: 17375096.8. Park H, Li Z, Yang XO, Chang SH, Nurieva R, Wang YH, et al. A distinct lineage of CD4 T cells regulates tissue inflammation by producing interleukin 17. Nat Immunol. 2005; 6:1133–1141. PMID: 16200068.
Article9. Zhao Y, Yang J, Gao YD, Guo W. Th17 immunity in patients with allergic asthma. Int Arch Allergy Immunol. 2010; 151:297–307. PMID: 19844129.
Article10. Leonardi C, Matheson R, Zachariae C, Cameron G, Li L, Edson-Heredia E, et al. Anti-interleukin-17 monoclonal antibody ixekizumab in chronic plaque psoriasis. N Engl J Med. 2012; 366:1190–1199. PMID: 22455413.
Article11. Jaleel T, Elmets C, Weinkle A, Kassira S, Elewski B. Secukinumab (AIN-457) for the treatment of psoriasis. Expert Rev Clin Pharmacol. 2016; 9:187–202. PMID: 26647300.
Article12. Ferrières L, Konstantinou MP, Bulai Livideanu C, Hegazy S, Tauber M, Amelot F, et al. Long-term continuation with secukinumab in psoriasis: association with patient profile and initial psoriasis clearance. Clin Exp Dermatol. 2019; 44:e230–4. PMID: 31055846.
Article13. McKinley L, Alcorn JF, Peterson A, Dupont RB, Kapadia S, Logar A, et al. TH17 cells mediate steroid-resistant airway inflammation and airway hyperresponsiveness in mice. J Immunol. 2008; 181:4089–4097. PMID: 18768865.
Article14. Wang YH, Voo KS, Liu B, Chen CY, Uygungil B, Spoede W, et al. A novel subset of CD4+ TH2 memory/effector cells that produce inflammatory IL-17 cytokine and promote the exacerbation of chronic allergic asthma. J Exp Med. 2010; 207:2479–2491. PMID: 20921287.15. Irvin C, Zafar I, Good J, Rollins D, Christianson C, Gorska MM, et al. Increased frequency of dual-positive TH2/TH17 cells in bronchoalveolar lavage fluid characterizes a population of patients with severe asthma. J Allergy Clin Immunol. 2014; 134:1175–1186.e7. PMID: 25042748.16. Busse WW, Holgate S, Kerwin E, Chon Y, Feng J, Lin J, et al. Randomized, double-blind, placebo-controlled study of brodalumab, a human anti-IL-17 receptor monoclonal antibody, in moderate to severe asthma. Am J Respir Crit Care Med. 2013; 188:1294–1302. PMID: 24200404.
Article17. Makihara S, Okano M, Fujiwara T, Kariya S, Noda Y, Higaki T, et al. Regulation and characterization of IL-17A expression in patients with chronic rhinosinusitis and its relationship with eosinophilic inflammation. J Allergy Clin Immunol. 2010; 126:397–400.e11. PMID: 20621345.
Article18. Saitoh T, Kusunoki T, Yao T, Kawano K, Kojima Y, Miyahara K, et al. Role of interleukin-17A in the eosinophil accumulation and mucosal remodeling in chronic rhinosinusitis with nasal polyps associated with asthma. Int Arch Allergy Immunol. 2010; 151:8–16. PMID: 19672092.
Article19. Jiang XD, Li GY, Li L, Dong Z, Zhu DD. The characterization of IL-17A expression in patients with chronic rhinosinusitis with nasal polyps. Am J Rhinol Allergy. 2011; 25:e171–5. PMID: 22186234.
Article20. Buerger C, Shirsath N, Lang V, Berard A, Diehl S, Kaufmann R, et al. Inflammation dependent mTORC1 signaling interferes with the switch from keratinocyte proliferation to differentiation. PLoS One. 2017; 12:e0180853. PMID: 28700632.
Article21. Buerger C. Epidermal mTORC1 signaling contributes to the pathogenesis of psoriasis and could serve as a therapeutic target. Front Immunol. 2018; 9:2786. PMID: 30555471.
Article22. Xu G, Xia J, Hua X, Zhou H, Yu C, Liu Z, et al. Activated mammalian target of rapamycin is associated with T regulatory cell insufficiency in nasal polyps. Respir Res. 2009; 10:13. PMID: 19250527.
Article23. Chen JY, Hour TC, Yang SF, Chien CY, Chen HR, Tsai KL, et al. Autophagy is deficient in nasal polyps: implications for the pathogenesis of the disease. Int Forum Allergy Rhinol. 2015; 5:119–123. PMID: 25533020.
Article24. Fokkens WJ, Lund VJ, Mullol J, Bachert C, Alobid I, Baroody F, et al. EPOS 2012: European position paper on rhinosinusitis and nasal polyps 2012. A summary for otorhinolaryngologists. Rhinology. 2012; 50:1–12. PMID: 22469599.
Article25. Kim DW, Khalmuratova R, Hur DG, Jeon SY, Kim SW, Shin HW, et al. Staphylococcus aureus enterotoxin B contributes to induction of nasal polypoid lesions in an allergic rhinosinusitis murine model. Am J Rhinol Allergy. 2011; 25:e255–61. PMID: 22185735.26. Kim DK, Jin HR, Eun KM, Mo JH, Cho SH, Oh S, et al. The role of interleukin-33 in chronic rhinosinusitis. Thorax. 2017; 72:635–645. PMID: 27885166.
Article27. Wang H, Li ZY, Jiang WX, Liao B, Zhai GT, Wang N, et al. The activation and function of IL-36γ in neutrophilic inflammation in chronic rhinosinusitis. J Allergy Clin Immunol. 2018; 141:1646–1658. PMID: 29274415.
Article28. Xiu Q, Kong C, Gao Y, Gao Y, Sha J, Cui N, et al. Hypoxia regulates IL-17A secretion from nasal polyp epithelial cells. Oncotarget. 2017; 8:102097–102109. PMID: 29254228.
Article29. Jin W, Dong C. IL-17 cytokines in immunity and inflammation. Emerg Microbes Infect. 2013; 2:e60. PMID: 26038490.
Article30. Ono N, Kusunoki T, Ikeda K. Relationships between IL-17A and macrophages or MUC5AC in eosinophilic chronic rhinosinusitis and proposed pathological significance. Allergy Rhinol (Providence). 2012; 3:e50–4. PMID: 23342289.
Article31. Sergejeva S, Ivanov S, Lötvall J, Lindén A. Interleukin-17 as a recruitment and survival factor for airway macrophages in allergic airway inflammation. Am J Respir Cell Mol Biol. 2005; 33:248–253. PMID: 15901616.
Article32. Kato A. Immunopathology of chronic rhinosinusitis. Allergol Int. 2015; 64:121–130. PMID: 25838086.
Article33. Wang M, Zhang N, Zheng M, Li Y, Meng L, Ruan Y, et al. Cross-talk between TH2 and TH17 pathways in patients with chronic rhinosinusitis with nasal polyps. J Allergy Clin Immunol. 2019; 144:1254–1264. PMID: 31271788.34. Golebski K, Ros XR, Nagasawa M, van Tol S, Heesters BA, Aglmous H, et al. IL-1β, IL-23, and TGF-β drive plasticity of human ILC2s towards IL-17-producing ILCs in nasal inflammation. Nat Commun. 2019; 10:2162. PMID: 31089134.
Article35. Hong SL, Zhang YL, Kim SW, Kim DW, Cho SH, Chang YS, et al. Interleukin-17A-induced inflammation does not influence the development of nasal polyps in murine model. Int Forum Allergy Rhinol. 2015; 5:363–370. PMID: 25754984.
Article36. Wang CQ, Akalu YT, Suarez-Farinas M, Gonzalez J, Mitsui H, Lowes MA, et al. IL-17 and TNF synergistically modulate cytokine expression while suppressing melanogenesis: potential relevance to psoriasis. J Invest Dermatol. 2013; 133:2741–2752. PMID: 23732752.
Article37. Chiricozzi A, Guttman-Yassky E, Suárez-Fariñas M, Nograles KE, Tian S, Cardinale I, et al. Integrative responses to IL-17 and TNF-α in human keratinocytes account for key inflammatory pathogenic circuits in psoriasis. J Invest Dermatol. 2011; 131:677–687. PMID: 21085185.
Article38. Ortega C, Fernández-A S, Carrillo JM, Romero P, Molina IJ, Moreno JC, et al. IL-17-producing CD8+ T lymphocytes from psoriasis skin plaques are cytotoxic effector cells that secrete Th17-related cytokines. J Leukoc Biol. 2009; 86:435–443. PMID: 19487306.39. Zaba LC, Cardinale I, Gilleaudeau P, Sullivan-Whalen M, Suárez-Fariñas M, Fuentes-Duculan J, et al. Amelioration of epidermal hyperplasia by TNF inhibition is associated with reduced Th17 responses. J Exp Med. 2007; 204:3183–3194. PMID: 18039949.
Article40. Shah SA, Ishinaga H, Takeuchi K. Clarithromycin inhibits TNF-α-induced MUC5AC mucin gene expression via the MKP-1-p38MAPK-dependent pathway. Int Immunopharmacol. 2017; 49:60–66. PMID: 28550735.41. Oakley GM, Harvey RJ, Lund VJ. The role of macrolides in chronic rhinosinusitis (CRSsNP and CRSwNP). Curr Allergy Asthma Rep. 2017; 17:30. PMID: 28429305.
Article42. Nagai S, Kurebayashi Y, Koyasu S. Role of PI3K/Akt and mTOR complexes in Th17 cell differentiation. Ann N Y Acad Sci. 2013; 1280:30–34. PMID: 23551100.
Article43. Linke R, Pries R, Könnecke M, Bruchhage KL, Böscke R, Gebhard M, et al. Increased activation and differentiated localization of native and phosphorylated STAT3 in nasal polyps. Int Arch Allergy Immunol. 2013; 162:290–298. PMID: 24157808.
Article44. Shin HW, Cho K, Kim DW, Han DH, Khalmuratova R, Kim SW, et al. Hypoxia-inducible factor 1 mediates nasal polypogenesis by inducing epithelial-to-mesenchymal transition. Am J Respir Crit Care Med. 2012; 185:944–954. PMID: 22323302.
Article45. Zhang H, Zhou X, Chen X, Lin Y, Qiu S, Zhao Y, et al. Rapamycin attenuates Tc1 and Tc17 cell responses in cigarette smoke-induced emphysema in mice. Inflamm Res. 2019; 68:957–968. PMID: 31468083.
Article46. Yu R, Bo H, Villani V, Spencer PJ, Fu P. The inhibitory effect of rapamycin on Toll like receptor 4 and interleukin 17 in the early stage of rat diabetic nephropathy. Kidney Blood Press Res. 2016; 41:55–69. PMID: 26849067.
Article47. Ko DY, Shin JM, Um JY, Kang B, Park IH, Lee HM. Rapamycin inhibits transforming growth factor beta 1 induced myofibroblast differentiation via the phosphorylated-phosphatidylinositol 3-kinase mammalian target of rapamycin signal pathways in nasal polyp-derived fibroblasts. Am J Rhinol Allergy. 2016; 30:211–217. PMID: 28124643.
Article48. Chen F, Cao A, Yao S, Evans-Marin HL, Liu H, Wu W, et al. mTOR mediates IL-23 induction of neutrophil IL-17 and IL-22 production. J Immunol. 2016; 196:4390–4399. PMID: 27067005.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Update on Biologics in Treatment of Chronic Rhinosinusitis With Nasal Polyposis
- The Role of Allergy in the Severity of Chronic Rhinosinusitis
- Nucleotide-Binding Oligomerization Domain-Like Receptor 3 Inflammasome Inhibition by MCC950 Reduces the Lipopolysaccharide-Induced Interleukin-1β in Cultured Dispersed Nasal Polyp Cells
- Clinical Characteristics and Expression Pattern of IL-33 and IL-25 According to Histologic Classification in Chronic Rhinosinusitis with Nasal Polyposis
- Biomarkers in Chronic Rhinosinusitis with Nasal Polyp: Personalized Medicine Based on Endotype