Diabetes Metab J.
2020 Feb;44(1):91-102. 10.4093/dmj.2018.0251.
Changes in the Quality of Life in Patients with Type 2 Diabetes Mellitus According to Physician and Patient Behaviors
- Affiliations
-
- 1Outcomes Research/Real World Data Team, Corporate Affairs and Health & Value Division, Pfizer Pharmaceuticals Korea Ltd., Seoul, Korea.
- 2Department of Endocrinology and Metabolism, Kyung Hee University Hospital at Gangdong, Kyung Hee University School of Medicine, Seoul, Korea.
- 3Department of Internal Medicine, Korea University Anam Hospital, Korea University College of Medicine, Seoul, Korea.
- 4Department of Endocrinology and Metabolism, Chonnam National University Hospital, Chonnam National University Medical School, Gwangju, Korea.
- 5Department of Endocrine and Metabolism, Sejong General Hospital, Bucheon, Korea.
- 6Department of Internal Medicine, Hallym University Sacred Heart Hospital, Hallym University College of Medicine, Anyang, Korea.
- 7Department of Endocrinology and Metabolism, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 8Department of Internal Medicine, Yeungnam University Medical Center, Yeungnam University College of Medicine, Daegu, Korea.
- 9Department of Biostatistics, Korea University College of Medicine, Seoul, Korea.
- 10Department of Internal Medicine, Hallym University Kangdong Sacred Heart Hospital, Hallym University College of Medicine, Seoul, Korea. dm@hallym.or.kr
- KMID: 2470958
- DOI: http://doi.org/10.4093/dmj.2018.0251
Abstract
- BACKGROUND
Diabetes mellitus (DM) is the most common chronic metabolic disorder with an increasing prevalence worldwide. According to a previous study, physicians' treatment patterns or patients' behaviors change when they become aware of the risk for cardiovascular (CV) disease in patients with DM. However, there exist controversial reports from previous studies in the impact of physicians' behaviors on the patients' quality of life (QoL) improvements. So we investigate the changes in QoL according to physicians and patients' behavioral changes after the awareness of CV risks in patients with type 2 DM.
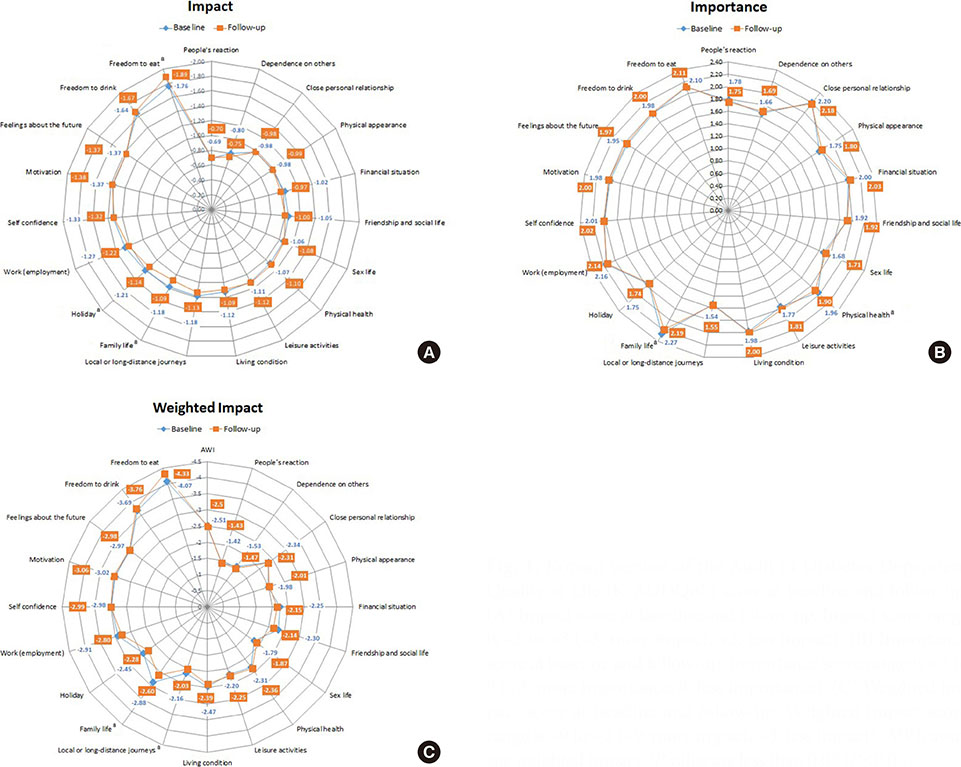
METHODS
Data were obtained from a prospective, observational study where 799 patients aged ≥40 years with type 2 DM were recruited at 24 tertiary hospitals in Korea. Changes in physicians' behaviors were defined as changes in the dose/type of antihypertensive, lipid-lowering, and anti-platelet therapies within 6-month after the awareness of CV risks in patients. Changes in patients' behaviors were based on lifestyle modifications. Audit of Diabetes Dependent Quality of Life comprising 19-life-domains was used.
RESULTS
The weighted impact score change for local or long-distance journey (P=0.0049), holidays (P=0.0364), and physical health (P=0.0451) domains significantly differed between the two groups; patients whose physician's behaviors changed showed greater improvement than those whose physician's behaviors did not change.
CONCLUSION
This study demonstrates that changes in physicians' behaviors, as a result of perceiving CV risks, improve QoL in some domains of life in DM patients. Physicians should recognize the importance of understanding CV risks and implement appropriate management.
MeSH Terms
Figure
Cited by 1 articles
-
Characteristics of Glycemic Control and Long-Term Complications in Patients with Young-Onset Type 2 Diabetes
Han-sang Baek, Ji-Yeon Park, Jin Yu, Joonyub Lee, Yeoree Yang, Jeonghoon Ha, Seung Hwan Lee, Jae Hyoung Cho, Dong-Jun Lim, Hun-Sung Kim
Endocrinol Metab. 2022;37(4):641-651. doi: 10.3803/EnM.2022.1501.
Reference
-
1. Kim DJ. The epidemiology of diabetes in Korea. Diabetes Metab J. 2011; 35:303–308.
Article2. World Health Organization. Global report on diabetes. Geneva: WHO Press;2016.3. Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care. 2004; 27:1047–1053.
Article4. International Diabetes Federation. IDF diabetes atlas. 8th ed. Brussels: International Diabetes Federation;2017.5. Al-Shehri AH, Taha AZ, Bahnassy AA, Salah M. Health-related quality of life in type 2 diabetic patients. Ann Saudi Med. 2008; 28:352–360.
Article6. Ryu J, Lee HA, Lee WK, Kim M, Min J, Hong YS, Park H. The association of self-care behavior and the quality of life among outpatients with diabetes. Korean J Fam Pract. 2014; 4:122–130.7. Bozorgmanesh M, Hadaegh F, Sheikholeslami F, Azizi F. Cardiovascular risk and all-cause mortality attributable to diabetes: Tehran lipid and glucose study. J Endocrinol Invest. 2012; 35:14–20.8. Fu AZ, Qiu Y, Radican L, Luo N. Marginal differences in health-related quality of life of diabetic patients with and without macrovascular comorbid conditions in the United States. Qual Life Res. 2011; 20:825–832.
Article9. Maddigan SL, Feeny DH, Johnson JA. Health-related quality of life deficits associated with diabetes and comorbidities in a Canadian National Population Health Survey. Qual Life Res. 2005; 14:1311–1320.
Article10. Haffner SM, Lehto S, Ronnemaa T, Pyorala K, Laakso M. Mortality from coronary heart disease in subjects with type 2 diabetes and in nondiabetic subjects with and without prior myocardial infarction. N Engl J Med. 1998; 339:229–234.
Article11. Standards of medical care in diabetes-2016: summary of revisions. Diabetes Care. 2016; 39:S4–S5.12. International Diabetes Federation. Global guideline for type 2 diabetes. Brussels: International Diabetes Federation;2012.13. Naghavi M, Falk E, Hecht HS, Jamieson MJ, Kaul S, Berman D, Fayad Z, Budoff MJ, Rumberger J, Naqvi TZ, Shaw LJ, Faergeman O, Cohn J, Bahr R, Koenig W, Demirovic J, Arking D, Herrera VL, Badimon J, Goldstein JA, Rudy Y, Airaksinen J, Schwartz RS, Riley WA, Mendes RA, Douglas P, Shah PK. SHAPE Task Force. From vulnerable plaque to vulnerable patient. Part III: executive summary of the Screening for Heart Attack Prevention and Education (SHAPE) task force report. Am J Cardiol. 2006; 98:2H–15H.14. Stevens RJ, Kothari V, Adler AI, Stratton IM. United Kingdom Prospective Diabetes Study (UKPDS) Group. The UKPDS risk engine: a model for the risk of coronary heart disease in type II diabetes (UKPDS 56). Clin Sci Lond. 2001; 101:671–679.
Article15. Jeong IK, Kim SG, Cho DH, Kim CH, Kim CS, Lee WY, Won KC, Kim DM. Impact of carotid atherosclerosis detection on physician and patient behavior in the management of type 2 diabetes mellitus: a prospective, observational, multicenter study. BMC Cardiovasc Disord. 2016; 16:220.
Article16. U.K. Prospective Diabetes Study Group. Quality of life in type 2 diabetic patients is affected by complications but not by intensive policies to improve blood glucose or blood pressure control (UKPDS 37). Diabetes Care. 1999; 22:1125–1136.17. Rubin RR, Peyrot M. Quality of life and diabetes. Diabetes Metab Res Rev. 1999; 15:205–218.
Article18. Ministry of Health and Welfare, Korea Institute for Health and Social Affairs. The third National Health and Nutrition Examination Survey (NHANES). Sejong: KIHASA;2005.19. Ministry of Health and Welfare, Korea Health Promotion Foundation. Customized visiting health management project. Sejong: KIHASA;2008.20. Morisky DE, Levine DM, Green LW, Shapiro S, Russell RP, Smith CR. Five-year blood pressure control and mortality following health education for hypertensive patients. Am J Public Health. 1983; 73:153–162.
Article21. Speight J, Reaney MD, Barnard KD. Not all roads lead to Rome: a review of quality of life measurement in adults with diabetes. Diabet Med. 2009; 26:315–327.22. Bradley C, Todd C, Gorton T, Symonds E, Martin A, Plowright R. The development of an individualized questionnaire measure of perceived impact of diabetes on quality of life: the ADDQoL. Qual Life Res. 1999; 8:79–91.
Article23. Bradley C, Speight J. Patient perceptions of diabetes and diabetes therapy: assessing quality of life. Diabetes Metab Res Rev. 2002; 18:S64–S69.
Article24. Chung JO, Cho DH, Chung DJ, Chung MY. An assessment of the impact of type 2 diabetes on the quality of life based on age at diabetes diagnosis. Acta Diabetol. 2014; 51:1065–1072.
Article25. Chung JO, Cho DH, Chung DJ, Chung MY. Assessment of factors associated with the quality of life in Korean type 2 diabetic patients. Intern Med. 2013; 52:179–185.
Article26. Shim YT, Lee J, Toh MP, Tang WE, Ko Y. Health-related quality of life and glycaemic control in patients with type 2 diabetes mellitus in Singapore. Diabet Med. 2012; 29:e241–e248.
Article27. Sundaram M, Kavookjian J, Patrick JH, Miller LA, Madhavan SS, Scott VG. Quality of life, health status and clinical outcomes in type 2 diabetes patients. Qual Life Res. 2007; 16:165–177.
Article28. Jannoo Z, Yap BW, Musa KI, Lazim MA, Hassali MA. An audit of diabetes-dependent quality of life in patients with type 2 diabetes mellitus in Malaysia. Qual Life Res. 2015; 24:2297–2302.
Article29. Pichon-Riviere A, Irazola V, Beratarrechea A, Alcaraz A, Carrara C. Quality of life in type 2 diabetes mellitus patients requiring insulin treatment in Buenos Aires, Argentina: a cross-sectional study. Int J Health Policy Manag. 2015; 4:475–480.
Article30. Wang HF, Yeh MC. The quality of life of adults with type 2 diabetes in a hospital care clinic in Taiwan. Qual Life Res. 2013; 22:577–584.
Article31. Papazafiropoulou AK, Bakomitrou F, Trikallinou A, Ganotopoulou A, Verras C, Christofilidis G, Bousboulas S, Μelidonis Α. Diabetes-dependent quality of life (ADDQOL) and affecting factors in patients with diabetes mellitus type 2 in Greece. BMC Res Notes. 2015; 8:786.
Article32. Holmanova E, Ziakova K. Audit diabetes-dependent quality of life questionnaire: usefulness in diabetes self-management education in the Slovak population. J Clin Nurs. 2009; 18:1276–1286.33. Yon M, Lee Y, Kim D, Lee J, Koh E, Nam E, Shin H, Kang BW, Kim JW, Heo S, Cho HY, Kim CI. Major sources of sodium intake of the Korean population at prepared dish level: based on the KNHANES 2008 & 2009. Korean J Community Nutr. 2011; 16:473–487.34. Kaya Erten Z, Zincir H, Ozkan F, Selcuk A, Elmali F. Sexual lives of women with diabetes mellitus (type 2) and impact of culture on solution for problems related to sexual life. J Clin Nurs. 2014; 23:995–1004.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Role of Sarcopenia in Diabetes Mellitus
- The Effect of a Community-Based Selp-Help Management Program for Patients with Diabetes Mellitus
- Social Support for Diabetes Patients
- Social Welfare Information for Patients with Diabetes Mellitus
- Association of Self-Care Behaviors and Quality of Life among Patients with Type 2 Diabetes Mellitus: Chaldoran County, Iran