Korean Circ J.
2020 Mar;50(3):220-233. 10.4070/kcj.2019.0176.
One-Year Clinical Outcomes between Single- versus Multi-Staged PCI for ST Elevation Myocardial Infarction with Multi-Vessel Coronary Artery Disease: from Korea Acute Myocardial Infarction Registry-National Institute of Health (KAMIR-NIH)
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Chungnam National University Hospital, Chungnam National University College of Medicine, Daejeon, Korea. jojeong@cnu.ac.kr
- 2Division of Cardiology, Department of Internal Medicine, Chonnam National University Hospital, Gwangju, Korea.
- 3Division of Cardiology, Department of Internal Medicine, Kyungpook National University Hospital, Daegu, Korea.
- 4Division of Cardiology, Department of Internal Medicine, Yeungnam University Hospital, Daegu, Korea.
- 5Division of Cardiology, Department of Internal Medicine, Kyunghee University College of Medicine, Seoul, Korea.
- 6Division of Cardiology, Department of Internal Medicine, Seoul National University Hospital, Seoul, Korea.
- 7Division of Cardiology, Department of Internal Medicine, Chungbuk National University Hospital, Cheongju, Korea.
- 8Division of Cardiology, Department of Internal Medicine, Samsung Medical Center, Sungkyunkwan University, School of Medicine, Seoul, Korea.
- KMID: 2470906
- DOI: http://doi.org/10.4070/kcj.2019.0176
Abstract
- BACKGROUND AND OBJECTIVES
Although complete revascularization is known superior to incomplete revascularization in ST elevation myocardial infarction (STEMI) patients with multi-vessel coronary artery disease (MVCD), there are no definite instructions on the optimal timing of non-culprit lesions percutaneous coronary intervention (PCI). We compared 1-year clinical outcomes between 2 different complete multi-vessel revascularization strategies.
METHODS
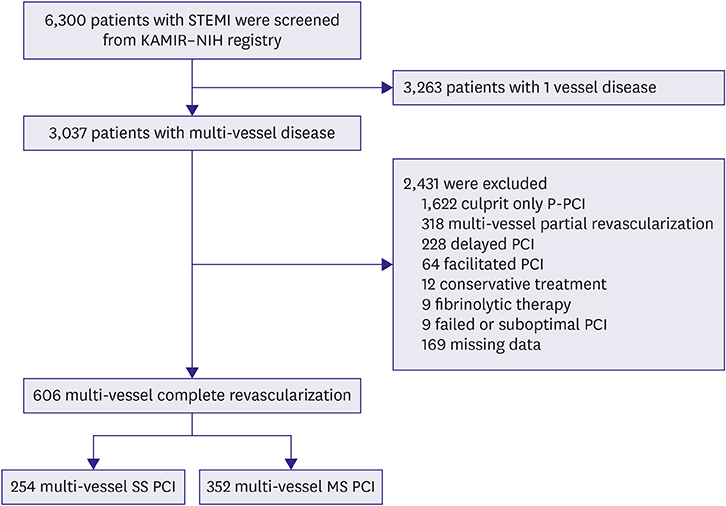
From the Korea Acute Myocardial Infarction Registry-National Institute of Health, 606 patients with STEMI and MVCD who underwent complete revascularization were enrolled from November 2011 to December 2015. The patients were assigned to multi-vessel single-staged PCI (SS PCI) group (n=254) or multi-vessel multi-staged PCI (MS PCI) group (n=352). Propensity score matched 1-year clinical outcomes were compared between the groups.
RESULTS
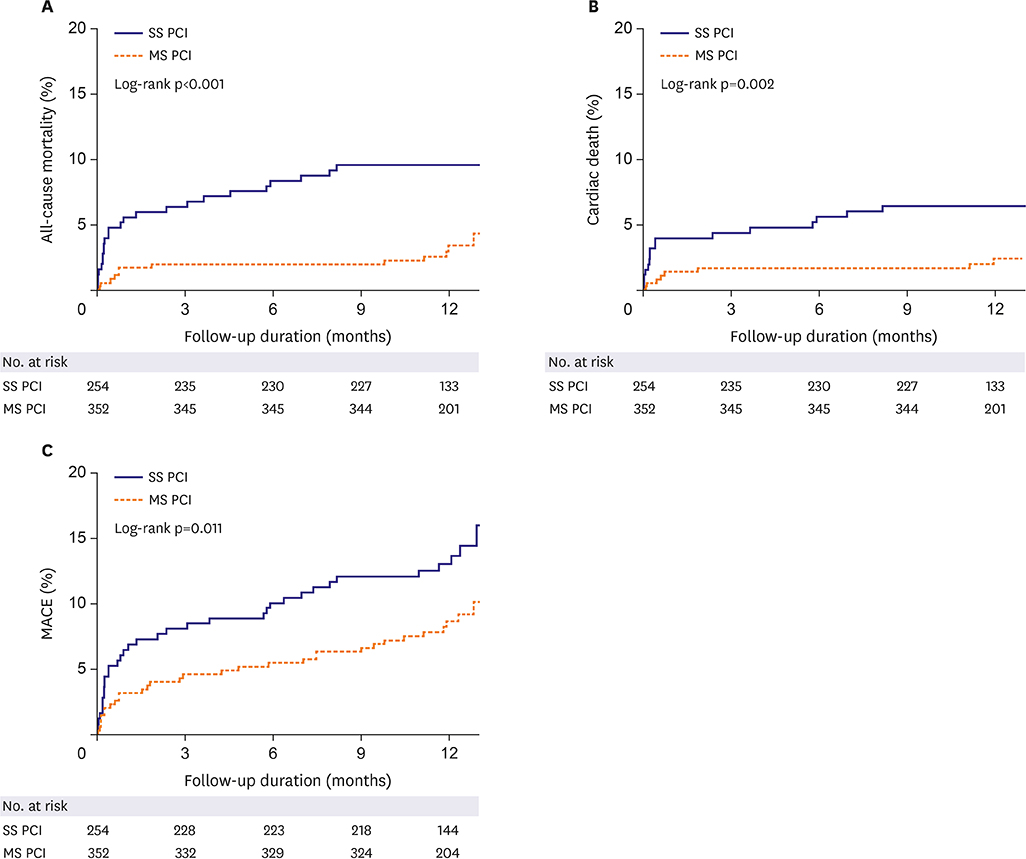
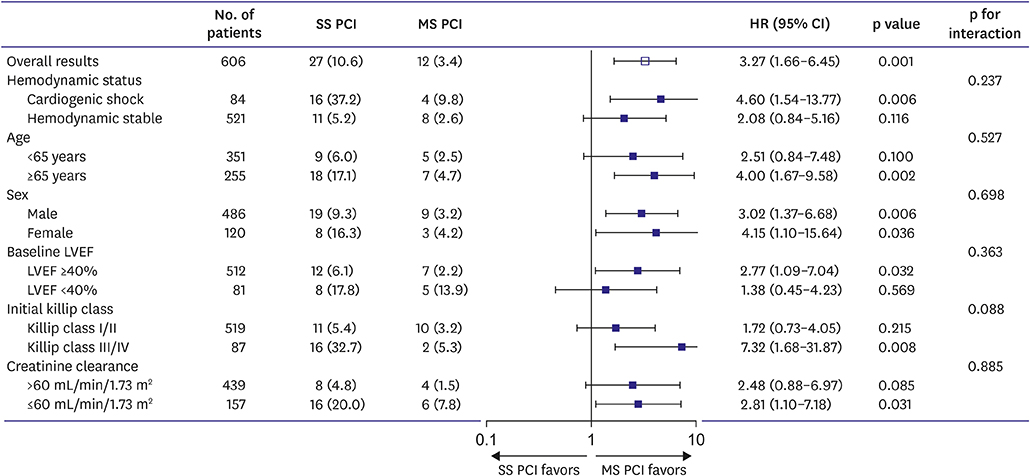
At one year, MS PCI showed a significantly lower rate of all-cause mortality (hazard ratio [HR], 0.42; 95% confidential interval [CI], 0.19-0.92; p=0.030) compared with SS PCI. In subgroup analysis, all-cause mortality increased in SS PCI with cardiogenic shock (HR, 4.60; 95% CI, 1.54-13.77; p=0.006), age ≥65 years (HR, 4.00; 95% CI, 1.67-9.58, p=0.002), Killip class III/IV (HR, 7.32; 95% CI, 1.68-31.87; p=0.008), and creatinine clearance ≤60 mL/min (HR, 2.81; 95% CI, 1.10-7.18; p=0.031). After propensity score-matching, MS PCI showed a significantly lower risk of major adverse cardiovascular event than SS PCI.
CONCLUSIONS
SS PCI was associated with worse clinical outcomes compared with MS PCI. MS PCI for non-infarct-related artery could be a better option for patients with STEMI and MVCD, especially high-risk patients.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Optimal Timing of Coronary Intervention in Non-Culprit Lesion in ST Elevation Myocardial Infarction with Multi-Vessel Disease
Jongkwon Seo, Jung-Sun Kim
Korean Circ J. 2020;50(3):234-235. doi: 10.4070/kcj.2020.0041.
Reference
-
1. Muller DW, Topol EJ, Ellis SG, et al. Multivessel coronary artery disease: a key predictor of short-term prognosis after reperfusion therapy for acute myocardial infarction. Am Heart J. 1991; 121:1042–1049.
Article2. Toma M, Buller CE, Westerhout CM, et al. Non-culprit coronary artery percutaneous coronary intervention during acute ST-segment elevation myocardial infarction: insights from the APEX-AMI trial. Eur Heart J. 2010; 31:1701–1707.
Article3. Corpus RA, House JA, Marso SP, et al. Multivessel percutaneous coronary intervention in patients with multivessel disease and acute myocardial infarction. Am Heart J. 2004; 148:493–500.
Article4. Vlaar PJ, Mahmoud KD, Holmes DR Jr, et al. Culprit vessel only versus multivessel and staged percutaneous coronary intervention for multivessel disease in patients presenting with ST-segment elevation myocardial infarction: a pairwise and network meta-analysis. J Am Coll Cardiol. 2011; 58:692–703.5. Cavender MA, Milford-Beland S, Roe MT, Peterson ED, Weintraub WS, Rao SV. Prevalence, predictors, and in-hospital outcomes of non-infarct artery intervention during primary percutaneous coronary intervention for ST-segment elevation myocardial infarction (from the National Cardiovascular Data Registry). Am J Cardiol. 2009; 104:507–513.
Article6. Varani E, Balducelli M, Aquilina M, et al. Single or multivessel percutaneous coronary intervention in ST-elevation myocardial infarction patients. Catheter Cardiovasc Interv. 2008; 72:927–933.
Article7. Kalarus Z, Lenarczyk R, Kowalczyk J, et al. Importance of complete revascularization in patients with acute myocardial infarction treated with percutaneous coronary intervention. Am Heart J. 2007; 153:304–312.
Article8. Levine GN, Bates ER, Blankenship JC, et al. 2015 ACC/AHA/SCAI focused update on primary percutaneous coronary intervention for patients with ST-elevation myocardial infarction: an update of the 2011 ACCF/AHA/SCAI Guideline for percutaneous coronary intervention and the 2013 ACCF/AHA Guideline for the management of ST-elevation myocardial infarction. J Am Coll Cardiol. 2016; 67:1235–1250.9. Ibanez B, James S, Agewall S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018; 39:119–177.10. Kornowski R, Mehran R, Dangas G, et al. Prognostic impact of staged versus “one-time” multivessel percutaneous intervention in acute myocardial infarction: analysis from the HORIZONS-AMI (harmonizing outcomes with revascularization and stents in acute myocardial infarction) trial. J Am Coll Cardiol. 2011; 58:704–711.11. Politi L, Sgura F, Rossi R, et al. A randomised trial of target-vessel versus multi-vessel revascularisation in ST-elevation myocardial infarction: major adverse cardiac events during long-term follow-up. Heart. 2010; 96:662–667.
Article12. Di Mario C, Mara S, Flavio A, et al. Single vs multivessel treatment during primary angioplasty: results of the multicentre randomised HEpacoat for cuLPrit or multivessel stenting for Acute Myocardial Infarction (HELP AMI) Study. Int J Cardiovasc Intervent. 2004; 6:128–133.13. Kim JH, Chae SC, Oh DJ, et al. Multicenter cohort study of acute myocardial infarction in Korea: interim analysis of the Korea Acute Myocardial Infarction Registry-National Institutes of Health registry. Circ J. 2016; 80:1427–1436.14. Claessen BE, Henriques JP, Jaffer FA, Mehran R, Piek JJ, Dangas GD. Stent thrombosis: a clinical perspective. JACC Cardiovasc Interv. 2014; 7:1081–1092.15. Kolte D, Sardar P, Khera S, et al. Culprit vessel-only versus multivessel percutaneous coronary intervention in patients with cardiogenic shock complicating ST-segment-elevation myocardial infarction: a collaborative meta-analysis. Circ Cardiovasc Interv. 2017; 10:e005582.
Article16. de Waha S, Jobs A, Eitel I, et al. Multivessel versus culprit lesion only percutaneous coronary intervention in cardiogenic shock complicating acute myocardial infarction: a systematic review and meta-analysis. Eur Heart J Acute Cardiovasc Care. 2018; 7:28–37.
Article17. Thiele H, Akin I, Sandri M, et al. One-year outcomes after PCI strategies in cardiogenic shock. N Engl J Med. 2018; 379:1699–1710.
Article18. Lee JM, Rhee TM, Hahn JY, et al. Multivessel percutaneous coronary intervention in patients with ST-segment elevation myocardial infarction with cardiogenic shock. J Am Coll Cardiol. 2018; 71:844–856.19. Galvão Braga C, Cid-Álvarez AB, Redondo Diéguez A, et al. Multivessel versus culprit-only percutaneous coronary intervention in ST-segment elevation acute myocardial infarction: analysis of an 8-year registry. Rev Esp Cardiol (Engl Ed). 2017; 70:425–432.
Article20. Bangalore S, Toklu B, Wetterslev J. Complete versus culprit-only revascularization for ST-segment-elevation myocardial infarction and multivessel disease: a meta-analysis and trial sequential analysis of randomized trials. Circ Cardiovasc Interv. 2015; 8:e002142.
Article21. Smits PC, Abdel-Wahab M, Neumann FJ, et al. Fractional flow reserve–guided multivessel angioplasty in myocardial infarction. N Engl J Med. 2017; 376:1234–1244.
Article22. Engstrøm T, Kelbæk H, Helqvist S, et al. Complete revascularisation versus treatment of the culprit lesion only in patients with ST-segment elevation myocardial infarction and multivessel disease (DANAMI-3—PRIMULTI): an open-label, randomised controlled trial. Lancet. 2015; 386:665–671.
Article23. Gershlick AH, Khan JN, Kelly DJ, et al. Randomized trial of complete versus lesion-only revascularization in patients undergoing primary percutaneous coronary intervention for STEMI and multivessel disease: the CvLPRIT trial. J Am Coll Cardiol. 2015; 65:963–972.24. Wald DS, Morris JK, Wald NJ, et al. Randomized trial of preventive angioplasty in myocardial infarction. N Engl J Med. 2013; 369:1115–1123.
Article25. Heusch G, Kleinbongard P, Böse D, et al. Coronary microembolization: from bedside to bench and back to bedside. Circulation. 2009; 120:1822–1836.26. Sianos G, Papafaklis MI, Daemen J, et al. Angiographic stent thrombosis after routine use of drug-eluting stents in ST-segment elevation myocardial infarction: the importance of thrombus burden. J Am Coll Cardiol. 2007; 50:573–583.27. Peterson ED, Dai D, DeLong ER, et al. Contemporary mortality risk prediction for percutaneous coronary intervention: results from 588,398 procedures in the National Cardiovascular Data Registry. J Am Coll Cardiol. 2010; 55:1923–1932.28. Hanratty CG, Koyama Y, Rasmussen HH, Nelson GI, Hansen PS, Ward MR. Exaggeration of nonculprit stenosis severity during acute myocardial infarction: implications for immediate multivessel revascularization. J Am Coll Cardiol. 2002; 40:911–916.
Article29. Assali AR, Brosh D, Ben-Dor I, et al. The impact of renal insufficiency on patients’ outcomes in emergent angioplasty for acute myocardial infarction. Catheter Cardiovasc Interv. 2007; 69:395–400.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Differences in Clinical Outcomes Between Patients With ST-Elevation Versus Non-ST-Elevation Acute Myocardial Infarction in Korea
- Long-term outcomes in ST-elevation myocardial infarction patients treated according to hospital visit time
- Differences in the Korea Acute Myocardial Infarction Registry Compared with Western Registries
- Current Status of Coronary Intervention in Patients with ST-Segment Elevation Myocardial Infarction and Multivessel Coronary Artery Disease
- Current status of acute myocardial infarction in Korea