J Neurocrit Care.
2019 Dec;12(2):98-101. 10.18700/jnc.190095.
Oxygen supplementation via high-flow nasal cannula is an effective treatment for pneumocephalus
- Affiliations
-
- 1Department of Neurology, Stroke Center, Dong-A University Hospital, Dong-A University College of Medicine, Busan, Republic of Korea. jhjeong@dau.ac.kr
- 2Department of Intensive Care Medicine, Dong-A University Hospital, Dong-A University College of Medicine, Busan, Republic of Korea.
- KMID: 2470471
- DOI: http://doi.org/10.18700/jnc.190095
Abstract
- BACKGROUND
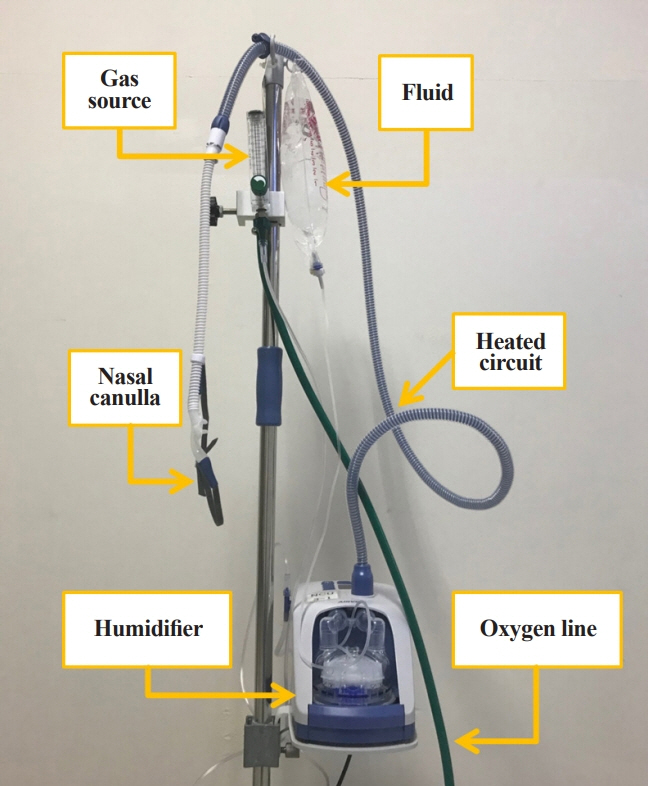
Oxygen supplementation through a high-flow nasal cannula (HFNC) is a powerful technique that promotes the absorption of air by delivering high concentrations of oxygen to patients who are not intubated, and may be a viable treatment option for pneumocephalus.
CASE REPORT
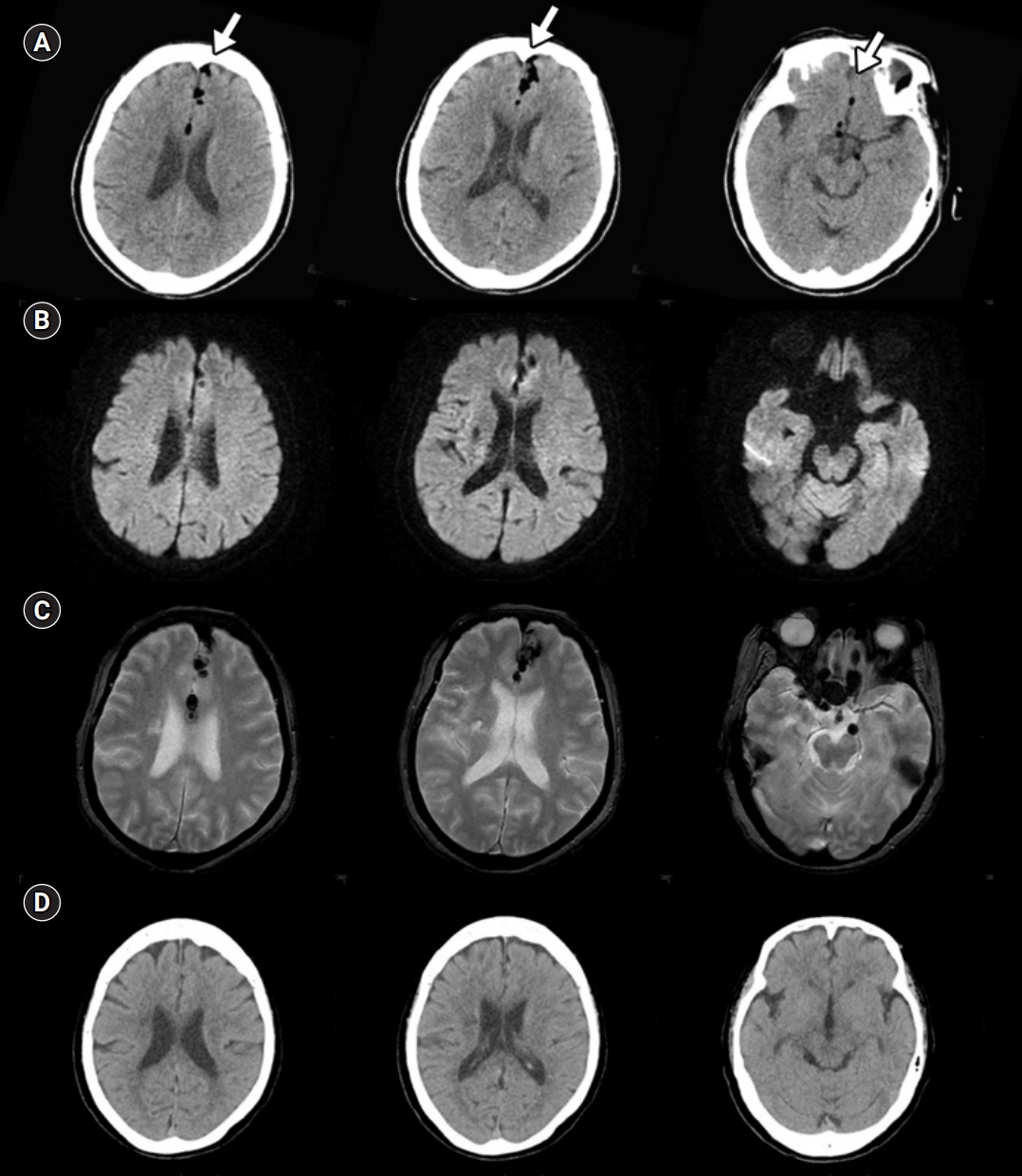
A 75-year-old female presented in a stuporous state. She had received an epidural injection due to back pain 2 hours ago. Non-contrast brain computed tomography revealed a pneumocephalus at the interhemispheric fissure and the prepontine cistern. HFNC oxygen therapy at 60 L/min with a fraction of inspired oxygen of 1 was started. By the next morning, her mental status had recovered and a repeat brain computed tomography 15 hours later revealed complete absorption of the pneumocephalus.
CONCLUSION
Supplemental high oxygen via HFNC can be successfully used in patients with pneumocephalus who are not intubated and mechanically ventilated.
MeSH Terms
Figure
Reference
-
1. Schirmer CM, Heilman CB, Bhardwaj A. Pneumocephalus: case illustrations and review. Neurocrit Care. 2010; 13:152–8.
Article2. Dexter F, Reasoner DK. Theoretical assessment of normobaric oxygen therapy to treat pneumocephalus. Anesthesiology. 1996; 84:442–7.
Article3. Gore PA, Maan H, Chang S, Pitt AM, Spetzler RF, Nakaji P. Normobaric oxygen therapy strategies in the treatment of postcraniotomy pneumocephalus. J Neurosurg. 2008; 108:926–9.
Article4. Hong B, Biertz F, Raab P, Scheinichen D, Ertl P, Grosshennig A, et al. Normobaric hyperoxia for treatment of pneumocephalus after posterior fossa surgery in the semisitting position: a prospective randomized controlled trial. PLoS One. 2015; 10:e0125710.
Article5. Hernández G, Roca O, Colinas L. High-flow nasal cannula support therapy: new insights and improving performance. Crit Care. 2017; 21:62.
Article6. Roca O, Riera J, Torres F, Masclans JR. High-flow oxygen therapy in acute respiratory failure. Respir Care. 2010; 55:408–13.7. Sztrymf B, Messika J, Bertrand F, Hurel D, Leon R, Dreyfuss D, et al. Beneficial effects of humidified high flow nasal oxygen in critical care patients: a prospective pilot study. Intensive Care Med. 2011; 37:1780–6.
Article8. Siegel JL, Hampton K, Rabinstein AA, McLaughlin D, Diaz-Gomez JL. Oxygen therapy with high-flow nasal cannula as an effective treatment for perioperative pneumocephalus: case illustrations and pathophysiological review. Neurocrit Care. 2018; 29:366–73.
Article9. Jeong JH. Brain and lung: lung injury in patients with brain injury. J Neurocrit Care. 2017; 10:1–6.
Article10. Chew YW, Suppan VK, Ashutosh SR, Tew MM, Jimmy-Tan JH. Pneumocephalus following combined spinal epidural anaesthesia for total knee arthroplasty: a case report. Malays Orthop J. 2017; 11:42–4.11. Markham JW. The clinical features of pneumocephalus based upon a survey of 284 cases with report of 11 additional cases. Acta Neurochir (Wien). 1967; 16:1–78.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Study on the Changes of SaO2, According to the Different Type of Oxygen Suppliers
- Factors about Failure after High Flow Oxygen through Nasal Cannula Therapy in Hypoxic Respiratory Failure Patients at Emergency Department Presentation
- Development of Nursing Practice Guidelines for Non-humidified Low Flow Oxygen Therapy by Nasal Cannula
- High Flow Nasal Cannula Assisted Tracheostomy for Securing Airways in Patients with Acute Respiratory Distress Induced by Glottic Cancer
- The Effect of Different Oxygen Flow Rates on Arterial Oxygenation and End-Tidal CO2 Measurements via a Nasal Cannula in Spinal Anesthesia